18 Open technique rhinoplasty
Synopsis
 Accurate preoperative analysis and clinical diagnosis set the foundation for successful primary open rhinoplasty.
Accurate preoperative analysis and clinical diagnosis set the foundation for successful primary open rhinoplasty.
 Open rhinoplasty allows anatomic exposure, identification, and correction of nasal deformities.
Open rhinoplasty allows anatomic exposure, identification, and correction of nasal deformities.
 Component dorsal hump reduction allows accurate and incremental reduction of the nasal dorsum while preventing problems with internal valve collapse or dorsal irregularities.
Component dorsal hump reduction allows accurate and incremental reduction of the nasal dorsum while preventing problems with internal valve collapse or dorsal irregularities.
 Nasal tip suturing techniques allow control of definition without damaging the osseocartilaginous framework and compromising support.
Nasal tip suturing techniques allow control of definition without damaging the osseocartilaginous framework and compromising support.
 Knowledge of the normal course of recovery and potential complications is key to managing patient expectations in the postoperative period.
Knowledge of the normal course of recovery and potential complications is key to managing patient expectations in the postoperative period.
Introduction
Rhinoplasty remains one of the most commonly performed aesthetic surgical procedures in plastic surgery, with over 279 000 performed in 2008.1 The trend over the past 20 years in modern rhinoplasty has shifted away from ablative techniques involving reduction of the osseocartilaginous framework to conserving the native anatomy with cartilage sparing, augmentation of deficient areas, and suture techniques to correct contour deformities and restore structural support.2 Emphasis on preoperative analysis and clinical diagnosis, refinements in techniques, and the popularization of the open approach in rhinoplasty (Table 18.1)3 have advanced the understanding of nasal anatomy and nasal surgery, leading to more predictable and consistent aesthetic and functional outcomes.
Table 18.1 Advantages and disadvantages of the open approach
| Advantages | Disadvantages |
|---|---|
| Binocular visualization | External nasal incision (transcolumellar scar) |
| Evaluation of complete deformity without distortion | Prolonged operative time |
| Precise diagnosis and correction of deformities | Protracted nasal tip edema |
| Allows use of both hands | Columellar incision separation |
| More options with original tissues and cartilage grafts | Delayed wound healing |
| Direct control of bleeding with electrocautery | |
| Suture stabilization of grafts (invisible and visible) |
Historical perspective
The first recorded treatment of nasal injuries dates back to approximately 3000 bc on the Egyptian surgical papyrus.4–8 Translated by Edwin Smith and later by James H Breasted,4,5 this document contained descriptions of the diagnosis and treatment of three nasal fractures. Reconstructive surgery for nasal deformities is described as early as 600 bc.9,10 In India, facial mutilation, especially of the nose, was practiced on adulterers, thieves, and other criminals, as a method of humiliation and stigmatization. In northern India, Sushruta, a member of a lowly priestly class, described techniques to transfer forehead and cheek skin to reconstruct the nose.8 In the 14th century, descriptions of nasal reconstruction again appear after a long period of quiescence during the dark ages, as the Renaissance brought forth advances in science and medicine. In Italy, Branca practiced the Indian methods for nasal reconstruction.11 His son modified these techniques by utilizing a delayed pedicled skin flap from the arm. This technique came to be known as the Italian method and was later reported by Benedetti,12 predating Gaspare Taglicozzi’s description in 1597. In the early 19th century, Carl von Graefe modified the Italian method by using a skin graft from the arm instead of a delayed pedicled skin flap. In 1845, another German, Johann Friedrich Dieffenbach, described external excisions of nasal soft tissue and cartilage to reduce excessively large noses.13 Dieffenbach was one of the first to describe nasal surgery for aesthetic improvement of the nose.7,8 John Orlando Roe, an American otolaryngologist, is credited with describing the first aesthetic rhinoplasty and introduced the endonasal approach.14,15 In 1887, Roe published The Deformity Termed “Pug Nose” and its Correction, by a Simple Operation and in 1891, The Correction of Angular Deformities of the Nose by a Subcutaneous Operation. Roe’s descriptions precede those of Jacques Joseph, a German orthopedic surgeon often regarded as the father of modern rhinoplasty, by 11 years.14 In 1898, Joseph published his experience with reduction rhinoplasty using external excisions similar to Dieffenbach. Joseph’s first report of the endonasal approach was in 1905.14 However, Joseph is often regarded as the father of modern rhinoplasty given his contribution to the analysis, classification, and repair of various nasal deformities.8 In the first half of the 20th century, the emergence of plastic surgery as a specialty was spurred forward by experience gained reconstructing devastating war injuries. The second half of the 20th century saw significant contributions to the rhinoplasty literature, enhancing preoperative assessment and diagnosis, management of the nasal airway, cartilage grafting techniques and popularization of the open approach to rhinoplasty.
Basic science/disease process
A thorough knowledge of nasal anatomy and understanding of nasal airflow and physiology are the foundations for successful aesthetic and functional rhinoplasty. Nasal anatomy is covered in detail in Chapter 17 and nasal airflow and physiology are covered in depth in Chapter 20. Deformities of the external and internal nose can be congenital or acquired, and may be secondary to soft-tissue and/or osseocartilaginous abnormalities, leading to aesthetic and/or functional consequences.
Diagnosis/patient presentation
Consultation
The initial consultation for rhinoplasty serves as an opportunity for the surgeon to obtain the patient’s nasal history and perform an anatomic examination. In addition, the surgeon should solicit the expectations of the patient. If the patient is a suitable candidate for rhinoplasty, informed consent should be obtained and preoperative instructions are given along with a general overview of postoperative care. Each patient should receive an information sheet containing the information shown in Figure 18.1.
Nasal history
During the nasal history, the surgeon should obtain information on the patient’s medical and emotional suitability to undergo rhinoplasty. In addition to reviewing the patient’s past medical history, the patient should be asked specifically about a history of allergic disorders, including hayfever and asthma, and other problems, including vasomotor rhinitis and sinusitis.16 These conditions should be well controlled prior to rhinoplasty. However, exacerbations of these conditions may occur in the postoperative period and may persist for several weeks to months; the patient should be informed about this before surgery. Nasal obstruction is usually found in patients with a long history of allergic rhinitis secondary to inferior turbinate hypertrophy.17 Engorgement of the inferior turbinates causes these symptoms to be worse at night. The patient may also complain of headache because of the inadequacy of the inferior turbinate to warm inspired air. Prior nasal trauma and surgeries, including rhinoplasty, septal reconstruction/septoplasty and sinus surgery, should be noted. Smoking, alcohol consumption, and use of illicit drugs, in particular cocaine, can compromise outcomes. Medications including acetylsalicylic acid, nonsteroidal anti-inflammatory drugs, fish oil, and certain herbal supplements may cause increased risk of bleeding18 and postoperative ecchymosis.
As with other aesthetic procedures, assessment of the emotional stability of the patient is critical when evaluating the patient seeking rhinoplasty.19–21 Motivating factors should be identified and the surgeon must differentiate between healthy and unhealthy reasons for seeking rhinoplasty. Feelings of inadequacy, immaturity, family conflicts, divorce, and other major life changes may be unhealthy motivating factors behind the patient seeking aesthetic surgery. Poor postoperative patient satisfaction is often based on emotional dissatisfaction as opposed to technical failure, and this can be avoided by the preoperative identification of these unhealthy motivating factors.18
Anatomic examination
Anatomic examination includes both external nasal analysis (Table 18.2) and internal nasal exam (Table 18.3). In addition, facial analysis plays a key role in achieving facial harmony after rhinoplasty.22 External nasal examination provides information about the underlying osseocartilaginous framework. Nasal skin is typically thinner and more mobile superiorly and thicker around the nasal tip.23,24 Skin is thinnest over the osseocartilaginous junction and thickest over the nasion and supratip area. Nasal skin characteristics such as thick sebaceous or thin skin will influence the outcome and recovery following rhinoplasty. Patients with thick nasal skin are prone to prolonged postoperative edema and scar formation requiring a longer recovery. More dramatic intraoperative manipulation of the osseocartilaginous framework is required in patients with thick nasal skin while subtle changes will be visible in patients with thin skin. Systematic nasal analysis is important to identify deformities, evaluate anatomical relationships, and establish goals for surgery. This is covered in depth in Chapter 17.
Table 18.2 External nasal analysis
| Frontal view | |
| Facial proportions | |
| Skin type/quality | Fitzpatrick type, thin or thick, sebaceous |
| Symmetry and nasal deviation | Midline, C-, reverse C-, S- or S-shaped deviation |
| Bony vault | Narrow or wide, asymmetrical, short or long nasal bones |
| Midvault | Narrow or wide, collapse, inverted-V deformity |
| Dorsal aesthetic lines | Straight, symmetrical or asymmetrical, well or ill defined, narrow or wide |
| Nasal tip | Ideal/bulbous/boxy/pinched, supratip, tip defining points, infratip lobule |
| Alar rims | Gull-shaped, facets, notching, retraction |
| Alar base | Width |
| Upper lip | Long or short, dynamic depressor septi muscles, upper lip crease |
| Lateral view | |
| Nasofrontal angle | Acute or obtuse, high or low radix |
| Nasal length | Long or short |
| Dorsum | Smooth, hump, scooped out |
| Supratip | Break, fullness, pollybeak |
| Tip projection | Over- or underprojected |
| Tip rotation | Over- or underrotated |
| Alar–columellar relationship | Hanging or retracted alae, hanging or retracted columella |
| Periapical hypoplasia | Maxillary or soft-tissue deficiency |
| Lip–chin relationship | Normal, deficient |
| Basal view | |
| Nasal projection | Over- or underprojected, columellar–lobular ratio |
| Nostril | Symmetrical or asymmetrical, long or short |
| Columella | Septal tilt, flaring of medial crura |
| Alar base | Width |
| Alar flaring |
Table 18.3 Internal nasal exam
| External valve | Collapse |
| Internal valve | Narrowing, collapse |
| Mucosa | Edema, irritation |
| Inferior turbinates | Hypertrophy |
| Septum | Deviation, tilt, spurs, perforation, cartilage |
| Masses | Polyps, tumors |
Imaging
Standardized photography is obtained for every patient presenting for rhinoplasty and includes frontal, lateral, oblique, and basal views of the patient.25 These are a critical component of the medical record for preoperative planning and evaluation of postoperative results. It is useful to review photographs with the patient to identify areas of concern that can be addressed with surgery and deformities that may persist after surgery, including notches, grooves, and irregularities. In addition, facial disproportions and asymmetries should be pointed out to the patient as these may require orthognathic surgery to address.
Informed consent
Prior to surgery, informed consent should be obtained following discussion about the surgery, alternative treatments, and disclosure of risks. The patient should be made aware of the possibility of additional surgery in the event of a complication or the need for revisionary surgery and his or her financial responsibilities if this situation were to arise.18
Patient selection
After completion of a detailed nasal history and anatomic examination, and the patient’s concerns and expectations have been discussed, the surgeon can decide if the patient is a good candidate for rhinoplasty. In general, the ideal candidate for surgery has legitimate concerns and realistic expectations, and is secure, well informed and understands the limitations of surgery. The acronym SYLVIA has been used to describe the ideal patient: secure, young, listens, verbal, intelligent, and attractive. The poor candidate for surgery has excessive concerns about minimal deformities and unrealistic expectations, and is insecure, poorly informed, and fails to recognize the limitations of surgery. The acronym SIMON has been used to describe this patient: single, immature, male, overly expectant, and narcissistic traits.19,26 These patients are likely to be unsatisfied following surgery regardless of the aesthetic improvement. They should be approached with caution and in most cases should not be operated on.
Treatment surgical technique
Anesthesia and preoperative management
Prior to sterile prep, the nose and septum are infiltrated with a total of 10 mL 1% lidocaine with 1 : 100 000 epinephrine. Injection in the submucoperichondrial plane of the nasal septum is performed followed by infiltration of the soft-tissue envelope. Injection of the highly vascular areas of the nose, including the columella, tip, dorsum, lateral side walls, alar base, and along the caudal margin of the lower lateral cartilages, is important for hemostasis. If inferior turbinoplasty is anticipated, the anterior head of the inferior turbinates is also injected. Oxymetazoline-soaked cottonoid pledgets are inserted into the nasal cavities. One drop of methylene blue is instilled in the oxymetazoline to differentiate this from the local anesthesia and prevent inadvertent injection. Typically, two or three cottonoid pledgets are placed in each nasal cavity. Comparable hemostasis can be obtained using lidocaine with oxymetazoline while avoiding the use of a controlled substance with potential cardiac effects, as seen with cocaine.27,28
Incisions and approach
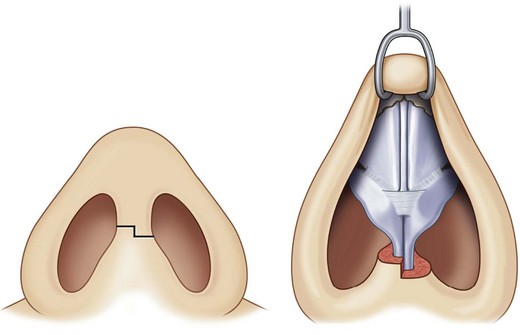
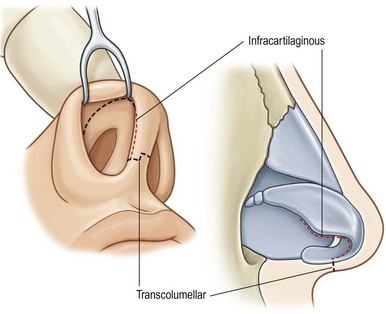
Adequate exposure during primary open rhinoplasty is best obtained using a transcolumellar incision with infracartilaginous extensions. Several transcolumellar incisions are commonly used, including stair-step, inverted-V, and transverse. Blood supply to the nasal tip is preserved with the transcolumellar incision provided that extensive defatting of the nasal tip or extensive alar base resections above the alar grooves are not performed.29,30 We prefer to use a stair-step incision which camouflages the scar, provides landmarks for accurate closure, and prevents linear scar contracture. Broken-line transcolumellar incisions may lead to better scar formation and less notching.31
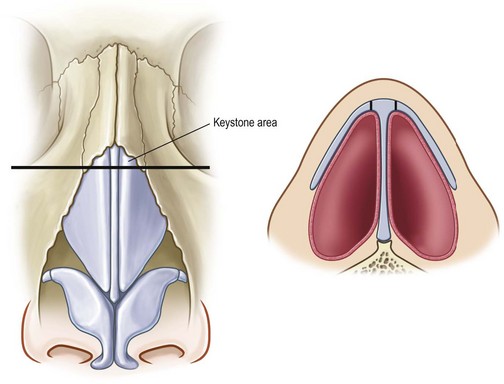
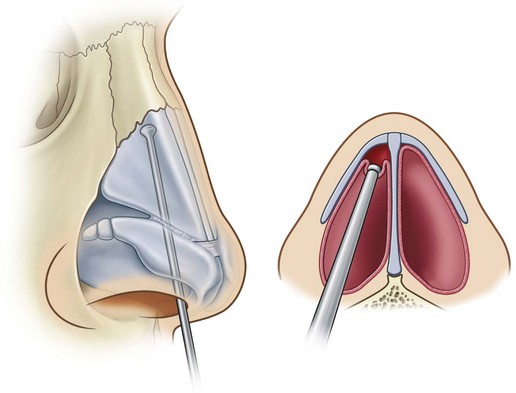
The stair-step transcolumellar incision is made at the narrowest part of the columella, which is typically at its midportion (Fig. 18.2). A 15-blade scalpel is used to incise the skin superficially, avoiding damage to the underlying medial crura. The incision is carried into the nasal vestibule and then continued along the caudal border of the medial crus towards the middle crus of the lower lateral cartilage. After everting the ala using external digital pressure against a double hook placed within the alar rim, a separate incision is started at the caudal border of the lateral crura and connected with the medial incision, caudal to the middle crus (Fig. 18.3). The lower edge of the lateral crus can be palpated after the ala has been everted to assure precise infracartilaginous incision placement. Fine dissecting scissors are used to elevate the nasal skin in a supraperichondrial plane starting from the columellar incision in a superior direction to the nasal tip. Next, dissection is started over the lateral crus and continued in a medial direction connecting the supraperichondrial dissection planes over the middle crus. Dissection to elevate the nasal skin in the supraperichondrial plane is carried superiorly to 2 mm above the keystone area. A Joseph elevator is then used to elevate nasal skin in a subperiosteal plane off nasal bones to radix. This dissection over the nasal bones is only performed in the central area to allow for bony dorsal hump reduction while the lateral periosteal attachments of the bony side wall should not be disrupted as they provide necessary stability to the bony vault after percutaneous osteotomies have been performed.32
Component dorsal hump reduction
An aesthetically pleasing nasal dorsum is critical to a successful result after rhinoplasty. Dorsal hump reduction without careful attention to the anatomic and physiologic functions of the nasal dorsum and internal nasal valve can lead to irregularities of the nasal dorsum, excessive narrowing of the midvault, the inverted-V deformity, and underresection or overresection of the osseocartilaginous hump.33 We prefer a graduated approach using component dorsal hump reduction (Box 18.1) over earlier techniques of composite dorsal hump reduction.33,34 This incremental reduction of the osseocartilaginous structures of the nasal dorsum offers increased control and reproducibility over composite dorsal hump reduction performed with an osteotome.
The nasal dorsum is initially modified prior to addressing the nasal tip, which establishes balance between the dorsum and tip essential to achieving the optimal aesthetic result.34 Component dorsal hump reduction is performed using five essential steps: (1) separation of the upper lateral cartilage from the septum; (2) incremental reduction of the septum proper; (3) incremental dorsal bony reduction (using a rasp); (4) verification by palpation; and (5) final modifications, if indicated (spreader grafts, suturing techniques, osteotomies).33,34
After dorsal undermining of the nasal soft tissues has been carried over the central aspect of the bony vault, the lower lateral cartilages are separated from each other and the septum by taking down the interdomal suspensory ligament. The creation of bilateral submucoperichondrial tunnels along the dorsal septum is essential prior to component dorsal hump reduction. This allows extramucosal resection of the osseocartilaginous components of the dorsal hump preventing late cicatricial narrowing of the internal nasal valve and webbing of the vestibule causing potential nasal airway obstruction. The perichondrium is scored at the nasal septal angle with a 15-blade scalpel and then, using a Cottle elevator, dissection in a submucoperichondrial plane is performed from caudal to cephalad along the dorsal septum until the nasal bones are reached. Once in the correct plane, there should be little resistance elevating the mucoperichondrium off the septal cartilage. The upper lateral cartilages are separated from the septum sharply using a 15-blade scalpel. By incising along the surface of the septal cartilage to separate the upper lateral cartilages, the transverse projections of the T-shaped dorsal septum are kept attached to the upper lateral cartilages (Fig. 18.4). This helps to minimize the need for spreader grafts to maintain the internal valve. Following this, angled septal scissors are used to reduce the septal cartilage incrementally. This cartilage is saved and can be used later for grafts, including as a columellar strut graft if large enough.35 Preservation of the upper lateral cartilages during dorsal reduction of the cartilaginous septum is important in achieving smooth dorsal aesthetic lines while equal resection of the septum and upper lateral cartilages results in rounding of the dorsum and excessive resection of the upper lateral cartilages results in the inverted-V deformity. For dorsal reduction of the bony hump less than 3 mm, a down-biting diamond rasp is used to reduce the bony dorsum incrementally. Rasping should proceed along left and right dorsal aesthetic lines and then centrally, employing short excursions of the rasp for maximal control. Care is taken to avoid avulsing the attachments of the upper lateral cartilages from the undersurface of the nasal bones. If a larger reduction of the bony dorsum is required, a guarded 8-mm osteotome can be used. The osteotomy should start at the caudal aspect of the nasal bones and is directed towards the radix. A rasp is used for final adjustments. Only in limited circumstances is reduction of the upper lateral cartilages indicated. Overresection must be avoided to prevent internal valve collapse or long-term dorsal irregularities. Patients with short nasal bones and high and narrow osseocartilaginous framework are at higher risk for these problems.35 Most importantly, after each incremental modification of the dorsum, the nasal skin is replaced and the contour of the nasal dorsum is assessed using the three-point dorsal palpation test in order to avoid overresection of the dorsum.33,34
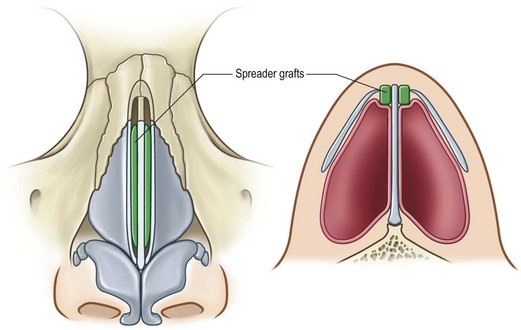
When the transverse projections of the T-shaped dorsal septum are kept attached to the upper lateral cartilages, they act as autospreader grafts, maintaining the patency of the internal valves and contour of the dorsal aesthetic lines. In thicker-skinned patients, upper lateral cartilage-septal sutures are used to reapproximate the upper lateral cartilages to the septum to re-establish the integrity of the nasal dorsum. They can be reapproximated into their anatomic position, or rolled inward as cartilaginous spreader flaps. Spreader grafts may be added, and are indicated in primary rhinoplasty to recreate the dorsal aesthetic lines, widen the midvault, or correct the deviated nose (Fig. 18.5).36 They may be fashioned from harvested septal cartilage and are typically 5–6 mm in height and 30–32 mm in length. They can be placed either unilaterally or bilaterally parallel to the dorsal septum. If indicated for improvement of the dorsal aesthetic lines they can be visible, placed above the plane of the dorsal septum, and if indicated to improve function of the internal nasal valve they can be invisible, placed below the plane of the dorsal septum. Additionally, an extended spreader graft with its caudal extent projecting below the caudal septum can be used to lengthen the short nose.37 Spreader grafts are secured to the septum using 5-0 PDS horizontal mattress sutures. Overuse of spreader grafts in primary rhinoplasty can lead to excessive width of the midvault.33,34
Following re-establishment of the cartilaginous midvault, percutaneous osteotomies are performed to correct widened or asymmetrical nasal bones, or close the open-roof deformity if present after dorsal reduction.33,34 Osteotomies will be discussed later in this chapter.
The nasal airway
Proper identification of causative factors of nasal airway obstruction is key to successful treatment. Nasal airway obstruction can have both medically and surgically correctable causes. Common surgically correctable causes include nasoseptal deviation, internal or external valve dysfunction, and inferior turbinate hypertrophy.17 Management of issues related to the nasal airway is covered in detail in Chapter 20. However, septal reconstruction and inferior turbinoplasty/submucous resection are discussed here as they are commonly performed during primary open rhinoplasty in the patient with nasal airway obstruction secondary to septal deviation or inferior turbinate hypertrophy, respectively.
Septal reconstruction
Septal deviation can involve deviation of the septal cartilage, perpendicular plate of the ethmoid bone, or vomer away from the midline and can cause obstruction of one or both of the nasal airways, along with external deviation of the nose. In our experience, nasal deviations can be classified into three basic types: (1) caudal septal deviations; (2) concave dorsal deformities; and (3) concave/convex dorsal deformities (Box 18.2).38,39 Septal tilt is the most common type where the quadrangular cartilage and perpendicular plate of the ethmoid are straight but the quadrangular cartilage is tilted to one side internally and to the opposite side externally. Hypertrophy of the inferior turbinate contralateral to the side of internal deviation is usually present. Correction of septal deviation is key to improving nasal airflow and correcting the deviated nose and is executed using the following principles: (1) exposure of all deviated structures through the open approach; (2) release of all mucoperichondrial attachments to the septum, especially the deviated part; (3) straightening of the septum, and if necessary septal reconstruction, while maintaining an 8–10-mm caudal and dorsal L-strut; (4) restoration of long-term support with buttressing caudal septal batten or dorsal nasal spreader grafts; (5) if necessary, submucous resection of hypertrophied inferior turbinates; and (6) precisely planned and executed external percutaneous osteotomies.38
Inferior turbinoplasty/outfracture/submucous resection
The turbinates exist as three or four bilateral extensions from the lateral nasal cavity. The inferior turbinate consists of highly vascular mucoperiosteum covering a thin semicircular conchal bone.40 It is involved in regulation of filtration and humidification of inspired air. In combination with the internal nasal valve, the anterior extent of the inferior turbinate can be responsible for up to two-thirds of the upper airway resistance.17,41 Posteriorly, the inferior turbinate diverges away from the nasal septum, allowing for reduced upper-airway resistance in this area.17,42
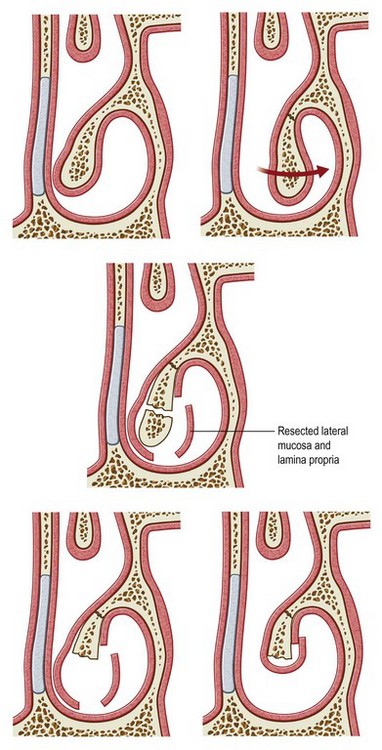
Inferior turbinoplasty is performed in patients with nasal airway obstruction secondary to inferior turbinate hypertrophy refractory to medical management. We prefer a more conservative surgical approach to correct inferior turbinate hypertrophy as we have found it to be effective with low morbidity. Overly aggressive surgical management may be complicated by bleeding, mucosal crusting and desiccation, ciliary dysfunction, chronic infection, malodorous nasal drainage, or atrophic rhinitis.17 In most cases, inferior turbinoplasty with outfracture of the inferior turbinate or submucous resection is adequate to achieve significant improvement (Fig. 18.6).
Harvesting autologous cartilage
The trend over the past two decades in rhinoplasty has shifted away from ablative techniques involving reducing the osseocartilaginous framework to conserving the native anatomy and augmentation of deficient areas to correct contour deformities and restore structural support. As such, certain situations require harvest of autologous cartilage for graft material. Autologous grafts are preferential to homografts and alloplastic implants because of their high biocompatibility and low risk of infection and extrusion.43 Their disadvantages include donor site morbidity, graft resorption, and unavailability of sufficient quantities for graft material.43 Autologous cartilage grafts are most commonly obtained from septal, ear, and costal cartilage. Other donor sites for autologous grafts include calvarial and nasal bone, and the olecranon process of the ulna.43 Concerns regarding donor site morbidity, graft availability, and graft resorption will necessitate the use of homologous or alloplastic implants.44
Septal cartilage
Open rhinoplasty allows for ease of septal cartilage harvest with improved exposure and visualization. Septal cartilage harvest is performed only after component dorsal hump reduction is complete as it is essential to preserve an 8–10-mm L-strut for nasal support. Dorsal reduction of the septum after septal cartilage harvest may leave an L-strut that is too narrow to provide adequate nasal support. Septal cartilage harvest is performed after the lower and upper lateral cartilages have been separated from the quadrangular cartilage. A 15-blade scalpel is used to score the mucoperichondrium of the septal angle and then a Cottle elevator is used to develop the submucoperichondrial pocket on one side of the septum (Fig. 18.7). Once in the correct plane, the denuded septal cartilage has a gray-blue hue, the septal cartilage has a gritty texture, and there should be little resistance elevating the mucoperichondrium off the septal cartilage until the dissection reaches the osseocartilaginous junction between the quadrangular cartilage and the vomer.
Dissection of the submucoperichondrial pocket is done towards the floor of the nasal cavity to the maxillary crest and posteriorly to the vomer (Fig. 18.8). The contralateral mucoperichondrium may be left attached to the septum and only the portion of the septal cartilage to be harvested is released. This method leaves contralateral mucoperichondrium attached to the L-strut for more support and decreases the amount of dissection and dead space with the potential for hematoma formation. Alternatively, development of these submucoperichondrial pockets can be performed bilaterally, allowing for improved visualization. During development of the submucoperichondrial pockets, care is taken to avoid perforations of the mucosa. Anterior perforations should be repaired with 5-0 chromic gut sutures while posterior perforations can be left as they allow for drainage of any blood. An 8–10-mm wide dorsal and caudal L-strut is created using a 15-blade scalpel to incise the septal cartilage parallel to the dorsal edge of the septum from the perpendicular plate of the ethmoid to a point 8–10 mm from the caudal edge of the septum (Fig. 18.9). This incision is then continued posteriorly and parallel to the caudal edge of the septum until the crest of the maxilla. Straight Mayo scissors are used to continue the dorsal incision across the osseocartilaginous junction of the quadrangular cartilage and the perpendicular plate of the ethmoid. A Cottle elevator is then used to elevate the septal cartilage from the maxillary crest and vomer and then to fracture the perpendicular plate between the dorsal incision and the vomer, liberating the septal cartilage. This septal cartilage is placed in a saline-moistened gauze until it is needed. During septal cartilage harvest, pressure on the L-strut must be avoided to prevent its fracture. If this occurs, it should be repaired to restore nasal support.45 Once the septal cartilage has been removed, any remaining septal spurs or deviations of the perpendicular plate of the ethmoid or vomer can be osteotomized or rongeured to remove these potential sites for nasal airflow interference. After cartilage grafts have been fashioned, any excess material should be replaced between the mucoperichondrial flaps in case it is required in subsequent procedures. The mucoperichondrial flaps can be sutured together using a 5-0 chromic gut quilting suture and are bolstered by placement of Doyle splints to support the mucoperichondrial flaps and minimize dead space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree