Open Retroperitoneal Nephrectomy
Leigh Anne Dageforde
Derek E. Moore
DEFINITION
Open donor nephrectomy is performed to recover a kidney for living donor kidney transplantation with minimal injury and risk to the donor. Open donor nephrectomy was the standard operation for live donors from 1954 until the mid-1990s. Recently, most centers have transitioned to laparoscopic donor nephrectomy; it has less postoperative pain and a faster recovery.1,2 Open donor nephrectomies continue to be important for donors with prior abdominal operations.
Some surgeons feel open donor nephrectomy facilitates longer donor vessel length and fewer abdominal complications (i.e., ileus) due to the retroperitoneal approach.2 Traditionally, open donor nephrectomy has had a shorter operative time than laparoscopic donor nephrectomy, but the operating times are approaching equivalence as surgeons have increasing experience and comfort with laparoscopic techniques. Current data indicate that kidneys removed by laparoscopic techniques have a longer warm ischemic time without clinical implications. In a systematic review of six randomized control trials of laparoscopic versus open donor nephrectomy, there was no significant difference in postoperative complications between laparoscopic and open donor nephrectomy.3
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients are eligible to be live kidney donors only after completing a comprehensive medical workup. A detailed history, including family history, and physical exam are performed. Generally, patients with hypertension, diabetes, obesity, renal insufficiency, or a history of cancer are not eligible. Patients must also have a normal urologic history including no history of hematuria, extensive nephrolithiasis, pyelonephritis, renal cysts, or tumors. Potential donors should be screened for a history of back pain or spine instrumentation due to positioning for the operation. The comprehensive workup has been described in detail in the chapter on laparoscopic donor nephrectomy (see Chapter 4). Surgeon experience with open donor nephrectomy (or lack of experience with laparoscopic donor nephrectomy) is the primary indication for choosing the open approach. Some patients with a numerous abdominal operations should have an open donor nephrectomy.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The preoperative imaging and diagnostic workup for living kidney donation is comprehensive and has also been detailed in a prior chapter. Specific to planning for the operating room, either an abdomen and pelvis computed tomography with contrast or computed tomography angiogram (CTA) are used to assess for any intraabdominal pathology and to define renal anatomy.4 Presence of multiple renal vessels may alter the operative approach (FIG 1). If there is any question, donors always retain the most normal kidney.
SURGICAL MANAGEMENT
Preoperative Planning
The risks of kidney donation must be discussed in detail with the donor and consent must be signed before proceeding to the operating room. The risks of the operation including bleeding, infection, damage to surrounding structures, deep vein thrombosis, and risks of anesthesia including death must be discussed. Long-term risks of kidney donation include the risk of hernia development, hypertension, and renal insufficiency or failure. Finally, both the donor and the recipient must understand there is a risk of graft failure in the transplanted kidney in the recipient.
Patients are given 5,000 units of subcutaneous heparin, and sequential compression devices are used on bilateral lower extremities throughout the operation as prophylaxis against deep vein thrombosis.
A one-time cefazolin dose or another appropriate broad spectrum antibiotic is given within 1 hour of incision for perioperative antibiotic prophylaxis.
Central venous access and invasive arterial monitoring are not necessary for the donor nephrectomy procedure. Large-bore peripheral intravenous (IV) lines are sufficient vascular access. A Foley catheter should be placed before the procedure begins.
Some patients undergoing open donor nephrectomy may benefit from having an epidural for pain control. The anesthesia team usually discusses this approach with the patient and places the epidural in the preoperative holding room.
Positioning
Patients are placed in the lateral decubitus position.
The arms are placed at a 90-degree angle at the shoulders. The lower arm is placed on an arm board and the upper on an arm holder.
The bed is flexed to the maximum extent and the kidney rest elevated so that the area between the anterior superior iliac spine (ASIS) and 12th rib is maximally extended.
All pressure points are padded to prevent nerve damage and pressure ulcers.
The patient is secured at three points to the operating room table.
TECHNIQUES
INCISION, EXPOSURE, AND ENTRY OF THE RETROPERITONEAL SPACE
Center the incision between the ASIS and the 12th rib, just anterior of the midaxillary line.
Divide the anterior portion of the latissimus dorsi and external oblique muscles.
Removing the 12th rib is no longer standard practice for a donor nephrectomy, but rib removal may be required in obese patients with difficult anatomy. Rib removal increases postoperative pain and discomfort.
Divide the internal oblique and transversus abdominis muscles using electrocautery. Then divide the transversalis fascia to expose the peritoneum.
The peritoneum is swept medially with blunt dissection to enter the retroperitoneal space and expose the perinephric fat.
EXPOSURE OF KIDNEY AND RENAL VESSELS
To expose the kidney and renal vessels, the perinephric fat and Gerota’s fascia must be divided.
Dissect away the perinephric fat from the kidney using blunt dissection and electrocautery (FIG 2).
The adrenal gland can be difficult to differentiate from the surrounding perinephric fat. Carefully dissect the adrenal gland away from superior surface of the kidney.
For a left nephrectomy, the left adrenal vein and gonadal vein must be ligated and divided (FIG 3). Lumbar veins are frequently present and must also be ligated with care; they tend to be thin and easily torn.
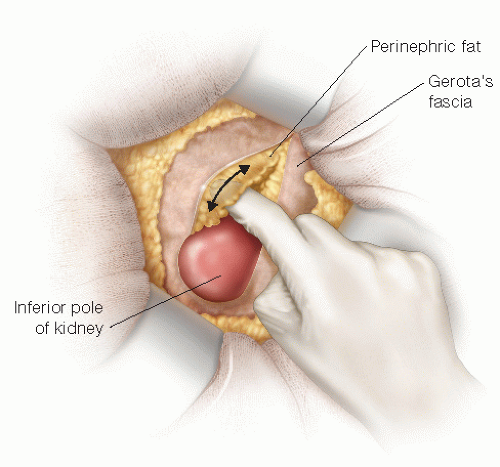
FIG 2 • Once the retroperitoneal space is entered, proceed with careful blunt dissection of Gerota’s fascia and perinephric fat.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access







