div class=”ChapterContextInformation”>
47. Prevention of Prosthetic Infection: Penile Implants and Artificial Urinary Sphincters
Keywords
Penile prosthesisArtificial urinary sphincterInfectionProsthetic surgery47.1 Introduction
Infection remains the most feared complication in all prosthetic surgical disciplines. Significant advances have been made to combat this rare but devastating complication over the past several decades, resulting in substantial declines in prosthetic urology infection rates. In this chapter we review prevention and management of infections of penile prostheses (IPP) and artificial urinary sphincters (AUS).
47.2 Historical Perspective
The first inflatable penile prosthesis was introduced in 1973 by Dr. F. Brantley Scott [1, 2]. The original surgical procedure was meticulous. Patients were shaved in the operating room and then underwent a 10-minute povidone-iodine scrub. The operative team was made to scrub in povidone-iodine, and their hands were then sprayed with iodine. They waited for it to completely dry before gowning and gloving. Patients received perioperative antibiotics, but Dr. Scott did not continue them in the post-operative period. Infectious complications of these early IPPs were low. Device failure and malfunction were more likely to cause complications and re-operations. Dr. Scott performed the surgeries within a closed encasement called a surgical isolation bubble system. In addition to pioneering this chamber (which is no longer used today), he contributed to the invention of the Lone Star Retractor (also known as the Scott Retractor ) [1].
47.3 Inflatable Penile Prosthesis Infection
Penile prostheses remain the gold standard for medical-refractory erectile dysfunction with high patient and partner satisfaction rates following successful surgery [3–5]. Over 25,000 penile prosthesis procedures are performed annually in the United States [6]. The procedure is safe and effective but not without risk. Device infection is perhaps the most devastating complication for both surgeons and patients. Infection rates at primary implantation range from 1–3% but can increase to up to 18% at revision surgery [7–10]. Infections are physically and emotionally challenging, expensive, and fraught with potential legal repercussions [6, 11–13]. Significant advances in both surgical technique and device development have resulted in substantial declines in infectious complications over the past several decades [6, 14, 15].
47.3.1 Types of Infection

Immediate penile prosthesis infection. Note the visible edema and erythema
Immediate penile prosthesis infection. Note the purulent fluid. (Image courtesy of Dr. Rafael Carrion)

Indolent penile prosthesis infection. Note the pump fixation to the scrotal wall
47.3.2 Pathophysiology
The classic teaching is that infection in prosthetic surgery is primarily due to contact with skin flora, although hematogenous spread of infection has also rarely been described [20]. An important concept to clarify is the distinction between infection and colonization. Almost all IPPs will be colonized after placement, whereas an actual infection is much rarer. In a large study of re-operations, Henry et al. found that 70% of prosthesis culture swabs from non-infection-related redo prosthetic procedures were positive for bacteria. Staphylococcus epidermidis, a skin bacteria of low virulence, was the most commonly isolated bacteria in that series [21]. Bacteria are thought to persist on the implant surface through a protective biofilm.
- 1.
Attachment
- 2.
Accumulation of extracellular polymeric substances
- 3.
Maturation
- 4.
Detachment [24].
When the bacteria are detached during IPP revision they can migrate and create new biofilm or cause infection elsewhere. Biofilm acts as a barrier to protect the bacteria from host immune response and antibiotics while simultaneously providing nourishment. The increased prevalence of infections at IPP revision surgeries is due to biofilm disruption and persistent bacterial presence [23].
47.3.3 Risk Factors
Certain medical comorbidities place patients at higher risk for IPP infections during primary placement. While the exact relationship between diabetes and infectious risk in IPP placement is still undefined, higher glucose levels theoretically favor bacterial growth and reproduction. Many studies have examined this relationship with mixed results, but the majority of research suggests that poorly controlled diabetics are at increased risk of infection [4, 6, 25–30]. Varied results also exist regarding spinal cord injury patients. The majority of studies show higher rates of infection, while one showed no difference [27, 31–33]. Definitive relationships between infection and implants in other distinct medical populations is yet to be determined. Sidi et al. followed penile implants in 14 renal transplant patients and concluded that this population was not at increased risk of infection [34]. However, when examining long term immunosuppression, Wilson et al. found that this was significantly associated with increased infection rates [27]. Along these lines, HIV positivity is associated with increased infectious rates, perhaps related to CD4 count [27, 33, 35].
Other inherent patient risk factors relate to patient lifestyle choices. Balen et al. examined socioeconomic and health risk factors for infection over a 12-year period. They concluded that active polysubstance abuse, homeless status, and poor preoperative glycemic control were all associated with increased infection at primary implantation [33].
Modifiable risk factors at primary and revision IPP surgery
Modifiable risk factors at primary surgery and proposed intervention | |
Medically manage intra-operatively | |
Careful patient selection; thorough counseling | |
Careful patient selection; thorough counseling | |
Immunosuppression [27] | Modify as able |
Polysubstance Abuse [33] | Pre-operative therapy and drug cessation |
Modifiable risk factors at revision surgery and proposed intervention | |
Medical optimization; intra-operative glucose control; anti-fungal prophylaxis | |
Prior implant Surgery [61] | Careful patient selection; thorough counseling |
Biofilm [61] | Peri-operative antibiotic selection; wound irrigation and washout |
47.4 Inflatable Penile Prosthesis Infection Prevention
Substantial effort and research has been devoted to reducing IPP infection rates in the last four decades. There are a number of evidence-based infection prevention techniques that are widely utilized, as well as other options that are not evidence-based but are widely implemented and anecdotally successful. Infection prevention begins well before surgery and continues throughout the perioperative period, as detailed below.
47.4.1 Preoperative Steps
Infection prevention starts during the preoperative evaluation in the clinic. A thorough history and physical exam is essential, especially paying close attention to the infectious risk factors discussed earlier. Modifiable health issues, like glucose control and use of antiretroviral therapy, should be addressed before surgery. The patient’s groin should be evaluated for bacterial or fungal skin infection, as this must be treated with oral medication before surgery. Preoperative urine cultures are commonly performed and should be treated if positive. More recently, their role in the preoperative evaluation is being questioned, but they remain a standard preoperative lab test [36, 37]. A Hemoglobin A1c may be obtained but, as mentioned earlier, the exact role of long-term preoperative glucose control in infections is unclear. One study reported higher rates of infection in diabetics with a HbA1c higher than 11.5% at the time of surgery [30]. Other authors have suggested that HbA1c of 8.5% is predictive of infection, although the studied population predominantly consisted of patients with malleable penile prostheses [38].
Preoperative diagnosis of staphylococcus aureus colonization, followed by appropriate treatment, has been associated with 20% lower rates of surgical site infections in other surgical disciplines. We use s. aureus nasal swab testing and pretreat positive patients with nasal mupirocin. All patients are ordered to scrub with chlorhexidine while bathing once a day for a week prior to surgery [39]. Historically this practice has been shown to be beneficial in other surgical disciplines, although more recent reviews of the data have been mixed regarding a significant benefit [40].
A final physical exam in the preoperative holding area is imperative, and any worrisome findings such as open sores, fungal infections, or rashes, must result in delay of the procedure. Preoperative glucose should be checked in the preoperative holding area, and values that increase risk of IPP infection should delay surgery. An insulin drip may be utilized for certain patients, but surgical delay until proper glucose control is achieved is preferred [33].
Preoperative hair removal remains a question. This is routinely performed for surgical exposure and to decrease any potential risk of infection from the hair. Overall, data suggests no difference in infection rates for hair removal the day prior to surgery when compared to the day of surgery. This was best analyzed in a Cochrane review that demonstrated multiple findings [41]. First, any hair removal vs no hair removal had no impact on incidence of surgical site infections. Next, when hair is removed, clippers have lower rates of infection vs shaving and this is thought to be due to less skin trauma and bacterial seeding [42]. No trials have examined cream hair removal vs clipping but when comparing creams to shaving, no surgical site infection difference was found. Hair clipping one day prior to vs the day of surgery similarly has no effect on infection rates. Based on the above data, the Sexual Medicine Society of North America (SMSNA) recommends either clippers or razors for hair removal prior to prosthetic surgery [43].
The American Urological Association and the European Association of Urology have recommended guidelines for preoperative antibiotic intravenous prophylaxis [44]. Recent research has questioned the utility of these guidelines in covering the most common infectious organisms seen during salvage or explant [45]. Antibiotics should be instilled within two hours of surgery and can be safely continued for 24 hours [46]. Many prosthetic urologists continue oral antibiotics postoperatively however there are no data to recommend this practice.
47.4.2 Intraoperative Steps
Significant variation exists among urologic prosthetic surgeons in hand scrub technique. A randomized control trial compared traditional preoperative scrubbing with an aqueous alcohol-based hand rub in reducing rates of infection in a variety of cases from a range of surgical fields. The study found that not only was there no difference in surgical site infection rates between the two groups but also that the hand rub group demonstrated higher compliance rates [47]. In addition to the type of surgical scrub, the duration has also been examined. The Centers for Disease Control and Prevention (CDC) recommend a 2–6 minute hand scrub prior to any surgical procedure but shorter times have also been studied to be equally effective [48]. No studies specifically examine these questions in the prosthetic urology literature. Gowning and gloving follows hand washing. A Cochrane review found no difference in surgical site infections based on wearing one or multiple pairs of gloves [49]. We recommended double gloving in case a break in a single glove introduces bacteria into the surgical site.
In addition to an appropriate sterile preparation, the surgical team is vitally important. We recommended a consistent operative team with minimal transitions and no extraneous traffic through the operating room. The anesthesia team also plays a role in reducing infection by maintaining body temperature and oxygenation [50, 51].
The patient’s skin should be prepped with chlorhexidine-alcohol (or another alcohol containing solution), as recommended by the North American Consensus Document on Infection of Penile Prostheses [52]. Two major studies contributed to this recommendation and are described below. The first study, by Yeung et al., examined efficacy of chlorhexidine-alcohol vs. povidone-iodine skin preparation in their ability to sterilize skin in urologic prosthetic surgery. They found a 50% lower post-preparation positive culture in the chlorhexidine group. Furthermore, the chlorhexidine preparation more effectively sterilized against coagulase negative staphylococcus [53]. In 2010, a study by Darouiche et al. examined surgical-site infections of clean-contaminated surgery using either chlorhexidine-alcohol or povidone-iodine skin preparation in over 800 patients. The group found an almost 50% decrease in surgical site infections when using the chlorhexidine-alcohol solution (9.5% vs 16.1%, p = 0.004). The benefit was observed in both superficial and deep infections [54].
IPP infection rates were substantially reduced in the early 2000s when both Coloplast (Minnetonka, Minnesota) and AMS (Marlborough, Massachusetts) released infection retardant coatings (IRCs). AMS (now Boston Scientific) devices use InhibiZone® , a proprietary blend of rifampin and gentamicin that is placed on the devices during manufacture. Coloplast devices have a hydrophilic coating that allows for surgeon selection of appropriate antibiotic solutions. When compared to their non-coated counterparts, these device changes have resulted in a 50–70% reduction in infectious complications [55].
As the most common bacterial offenders in prosthetic infections are skin flora, the no-touch technique (NTT) was pioneered by Eid in 2011 to minimize skin contact [ 56]. This surgical approach includes covering the entire surgical field with an adherent sterile drape such as the Steri-Drape® or Ioban® (3 M, Maplewood, Minnesota) and making the skin incision through this drape. The surgical team undergoes multiple glove changes throughout the case as new gloves are required after any contact with skin or with a change in instruments. A retrospective analysis of the no-touch technique revealed a 77% decrease in infection rates in IRC coated devices when using the NTT [57].
There are a variety of surgical approaches for the implantation of a penile prosthesis, including subcoronal, infrapubic, and peno-scrotal, and there does not appear to be any association between approach and surgical site infections. A large retrospective review by Garber et al. looked at over 300 patients stratified based on penoscrotal vs infrapubic approach and found no difference in infection rates [58].
Many studies across all fields suggest that centers with high surgical volumes have fewer complications and exhibit shorter operative times [59]. As increasing operative time is associated with IPP infection, the procedure should be kept as brief as possible [60]. Conducting other procedures at the time of IPP implantation is not recommended as this contributes to longer operative times and potentially to higher infectious rates.
47.4.3 Postoperative Steps
Steps to reduce post-operative hematoma include the application of a constricting surgical bandage. This Mummy wrap bandage technique was described by Henry in 2009 and a retrospective analysis demonstrated an over 80% decrease in infection rates, attributed to decrease in hematoma formation [33, 61]. In addition to the appropriate surgical dressing, tight closure of corporotomy sites, device inflation, and surgical drain placement have been associated with decreased hematoma formation. A multicenter study examining hematoma and infection rates with drain placement revealed no increase in infection and an overall low rate of hematoma formation [62]. Many experienced surgeons use a 7 mm Jackson-Pratt® (Cardinal Health, Ohio) drain for 12–24 hours post-operatively.
47.4.4 Revision Surgery Steps
In 2005, Henry et al. published a study of aggressive surgical site washout at the time of revision surgery [63]. This has been, arguably, the single most important factor in reducing infectious complications at revision procedures. In their multicenter retrospective study, a 75% decrease in infectious complications was noted for patients who received an antiseptic irrigation during revision surgery compared to those who did not. Another study conducted with saline irrigation found similar results [57]. Based on these studies, with similar data and different irrigation techniques, it is likely the process of vigorous irrigation that leads to decreased infections and not necessarily the type of irrigation.
47.5 Inflatable Penile Prosthesis Infection Treatment
47.5.1 Nonoperative
Some urologists have attempted to treat early infections with conservative management. One study treated 37 men with early signs of local penile prosthesis infection with oral antibiotics only. Approximately 80% of these patients avoided surgery. The inclusion criteria for this study were very strict, however, and included a WBC <13 k and no temperatures >37.5 °C [64]. These findings have not been duplicated in larger studies. We feel very strongly that patient selection for conservative management must be highly selective and adequate guidelines do not currently exist.
47.5.2 Operative
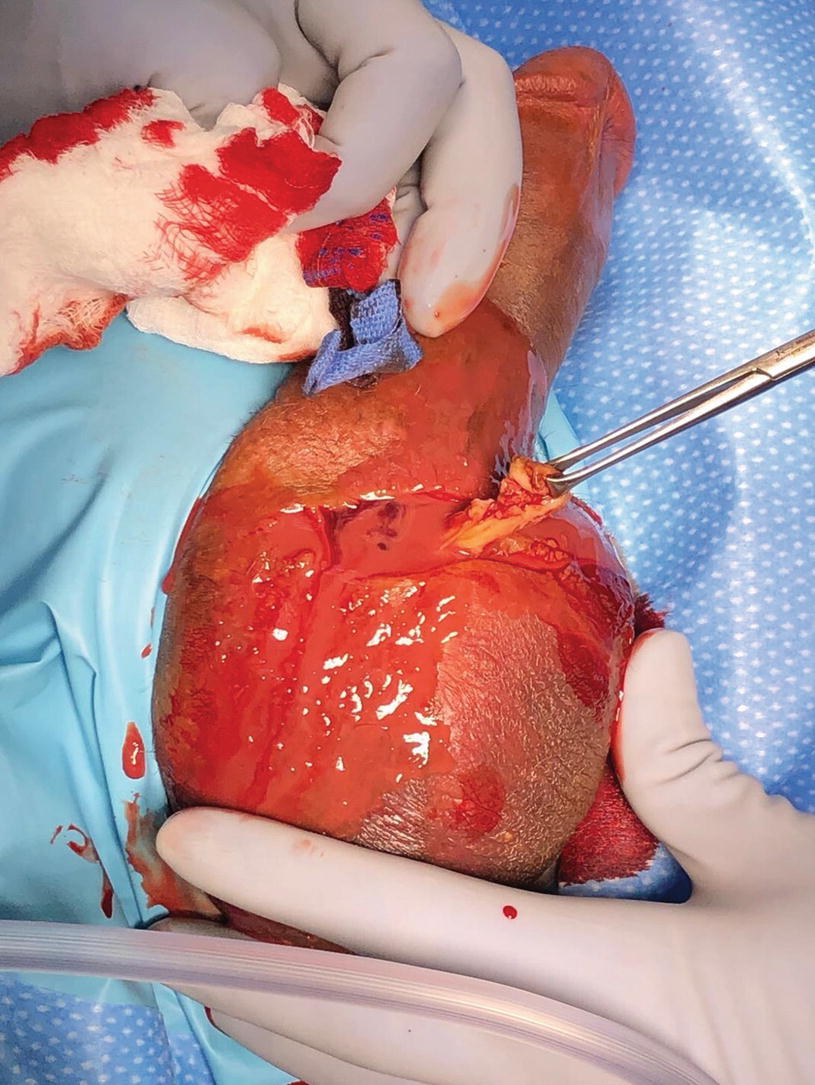
Once the diagnosis of IPP infection is made, the next step is surgical salvage or explant. Infection management was transformed in 1996 with the introduction of three-piece IPP salvage by Mulcahy. In this technique, the infected device is removed, a thorough washout is performed, and a new three-piece IPP is placed. Data have shown an 82% infection-free rate as well as decreased penile inactivity, fibrosis, and length loss when compared to delayed re-implantation [65]. This technique was updated in 2016 with the introduction of the Malleable Implant Salvage Technique, where a malleable implant is placed instead of an inflatable device, which results in a 93% infection-free rate. Salvage is the gold standard in IPP infection treatment for appropriate patients, however it is likely underutilized [66].
- 1.
Aspirate/swab the device for culture

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree