Fig. 18.1
Preoperative image: upper outer quadrantectomy of the right breast

Fig. 18.2
Postoperative results 6 months after subpectoral 90-cm3 implant insertion and external radiotherapy
18.3 Oncoplastic Surgery Plus Intraoperative Radiotherapy and Bilateral Breast Augmentation with Implants
This is a technique performed routinely in the European Institute of Oncology (IEO) for patients with small tumors and small breasts who wish for conservative surgery and also to increase the volume of the breast [10–12]. To avoid postoperative complications due to the traditional external radiotherapy, intraoperative radiotherapy can be done. All patients are treated with breast-conserving surgery (quadrantectomy). Electron beam intraoperative therapy is delivered by two mobile linear accelerators immediately after breast resection with a single dose of 21 Gy, which in radiobiology terms is similar to the 45-Gy of external radiotherapy. In young patients, only a boost in the tumor bed of 10 Gy is given and complementary external radiotherapy is provided after the surgery [13].
The quadrantectomy approach can be done through a periareolar incision. After tumor resection, the lateral glandular flaps are undermined to allow the insertion of two metallic disks (lead and aluminum) to protect the thoracic wall from diffusion of radiotherapy. Then, the mobile radiotherapy equipment is placed and the calculated dose is applied in the gland around the quadrantectomy. Then, the reconstructive step begins with insertion of the prosthesis below the pectoralis major muscle and with use of glandular flaps to cover the defect from quadrantectomy. The same implant is also used in the contralateral breast augmentation (Figs. 18.3, 18.4, 18.5 and 18.6).





Fig. 18.3
Preoperative drawings: T1 tumor located between the internal quadrants of the left breast

Fig. 18.4
After excision of the tumor, the metallic disks (aluminum and lead) are placed to protect the thoracic wall before starting the electron beam intraoperative therapy

Fig. 18.5
Intraoperative image: sterile collimator adjustment to deliver the intraoperative radiotherapy

Fig. 18.6
Postoperative image at 6 months: good cosmetic results without capsula contracture or radiodystrophy
18.4 Combined Mammaplasty Techniques
The oncoplastic surgeon with good experience with the main mammaplasty techniques can in special indications, such as breast size and tumor localization, combine two or more techniques to achieve a good cosmetic result. The basic requirement is good knowledge of breast blood supply in order to avoid skin and/or glandular necrosis.
A useful technique in cases of large tumors in the upper outer quadrant and huge and ptotic breasts is the double pedicle technique. One pedicle is similar to that in Skoog technique, in order to pull up the nipple and areola complex with good blood supply [14, 15]. A second pedicle is a skin glandular pedicle, based on the vascular pedicles from the lateral border of the pectoralis major muscle and will be used to cover the glandular defect in the upper outer quadrant. This is a good solution in this situation with tumors that are very superficial and it where it is oncologically necessary to remove the skin over the lump, the only disadvantage being the large scars (Figs. 18.7, 18.8, 18.9, and 18.10).
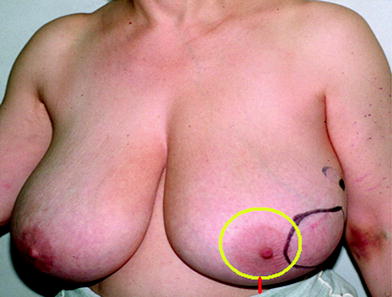
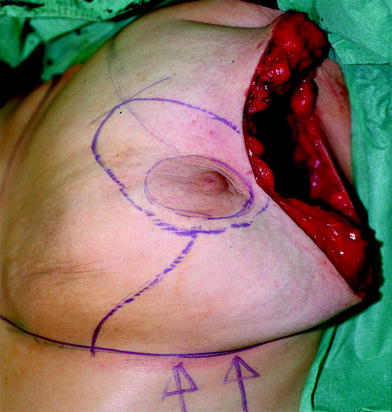


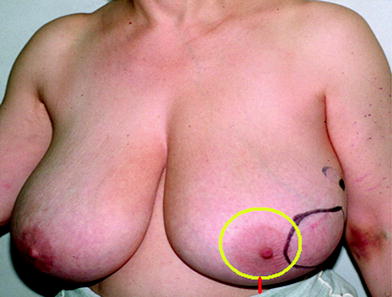
Fig. 18.7
Preoperative image: the black line is the tumor circumference
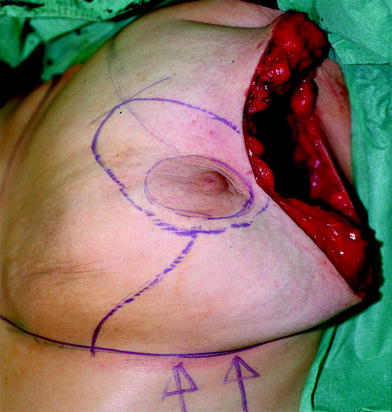
Fig. 18.8
Intraoperative image after the quadrantectomy (weight 420 g) and the drawing for Skoog and lower outer pedicle technique

Fig. 18.9
On-table view

Fig. 18.10
Cosmetic results 3 months after radiotherapy
Another option for tumors located in the upper outer quadrant is a technique similar to Lejour’s technique, but using the inferior triangle of glandular tissue rotated to cover the quadrantectomy defect (Figs. 18.11, 18.12, 18.13, 18.14, and 18.15). This technique can be used in large breasts with a medium degree of ptosis, the advantage being the shortness of the scars.

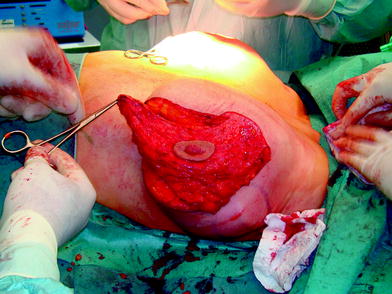
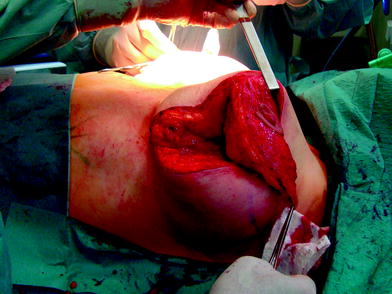



Fig. 18.11
Preoperative image: trifocal tumor in the upper outer quadrant. The drawing pattern is similar to that for the Lejour technique
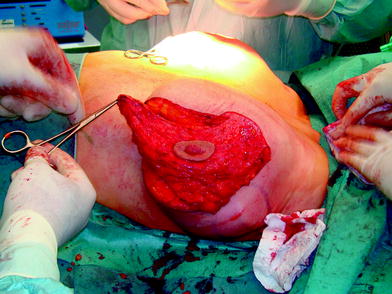
Fig. 18.12
Intraoperative image: after the quadrantectomy, a glandular flap is prepared on the basis of the upper inner quadrant
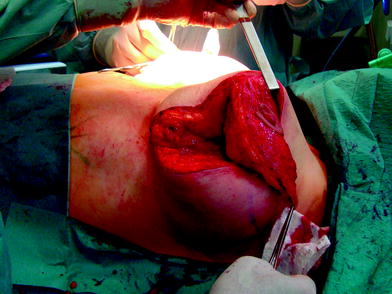
Fig. 18.13
Intraoperative image: the inferior triangle of glandular tissue normally removed with this technique will be rotated to cover the upper outer defect

Fig. 18.14
Intraoperative image showing the final reshaping with only periareolar and vertical scars

Fig. 18.15
Postoperative image after 6 months
18.5 Fasciocutaneous Abdominal Flaps
It is always a challenge to achieve good cosmetic results with conservative surgery for small tumors in small breasts. In the case of thin patients with a small breast without ptosis and small tumors located in the inferior quadrant, a fasciocutaneous flap harvest just above the inframammary fold and rotation to cover the defect can be indicated [16, 17]. The flap should be taken just above the inframammary fold and the pedicle oriented in the medial portion to preserve the perforator vessels coming through the upper part of the rectus abdominis muscle. The flap orientations follow the inframammary fold in order to maintain the scar exactly at this level so it is less visible (Figs. 18.16, 18.17, and 18.18) [18].




Fig. 18.16
Preoperative drawings: skin excision for lower tumor resection and flap drawing in order to put the final scar in the inframammary fold

Fig. 18.17
Intraoperative image: flap rotation and the abdominal skin flap should be undermined to fix the final scar at the level of the inframammary fold

Fig. 18.18
Postoperative image after 1 month
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








