Fig. 39.1
Immediate breast reconstruction decision algorithm in pregnancy and lactation
1.
First trimester. Immediate reconstruction in one-step surgery with breast implants and contralateral symmetrization by breast reduction or mastopexy, or in two-step surgery with temporary expanders (Fig. 39.2).
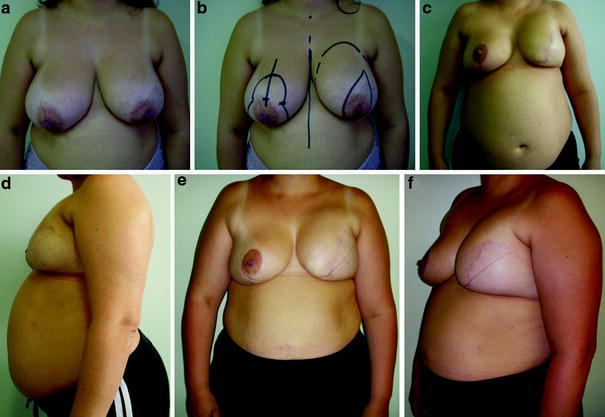
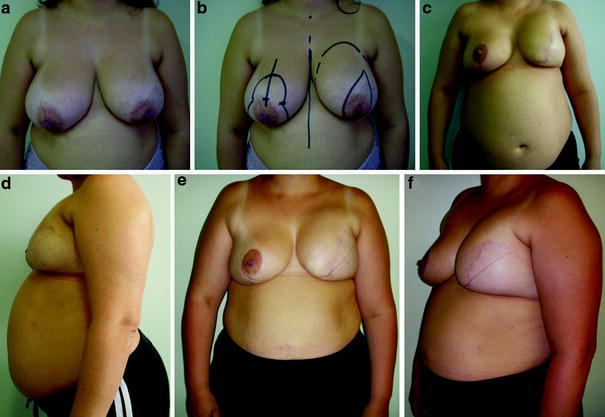
Fig. 39.2
a, b Preoperative views of a 32-year-old patient, in the eighth week of pregnancy, with diagnosis of an invasive ductal carcinoma of the left breast, G2, T2N1, estrogen receptor (ER)/progesterone receptor (PgR) positive, human epidermal growth factor receptor 2 (HER2) negative. c, d Eight months after left skin-sparing mastectomy, axillary dissection, immediate breast reconstruction with a form-stable implant, and contralateral breast reduction for achievement of symmetry. e, f Results 4 months after delivery
2.
Second and third–trimester. Temporary expanders.
3.
Lactation. Temporary expanders, autologous flaps, or breast-conserving therapy (BCT). If the lactation ceased at least 3 months earlier, it is possible to perform one-step surgery with a definitive implant and contralateral breast symmetrization (Fig. 39.3). In this situation, a breast conservative surgery approach is possible too.
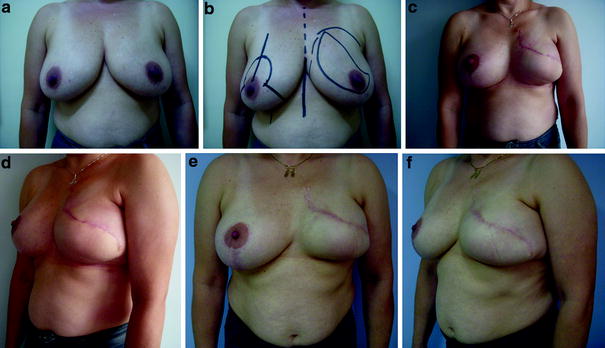
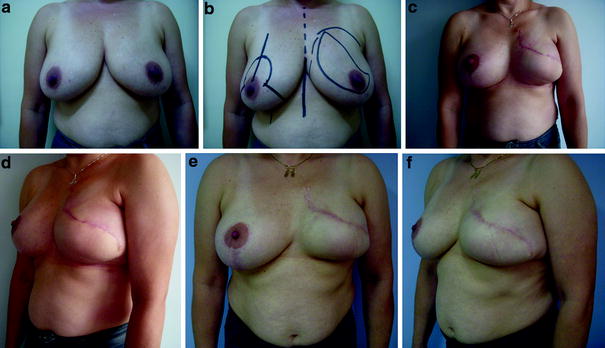
Fig. 39.3
a, b Preoperative views of a 37-year-old patient with a multicentric invasive ductal carcinoma of the left breast, T2N0, ER/PgR negative, HER2 negative, and lactation that ceased 3 months earlier. c, d Three months after left skin-sparing mastectomy, sentinel node biopsy, immediate breast reconstruction with a definitive form-stable implant and contralateral breast reduction for achievement of symmetry. e, f Long-term result: 2 years after surgery
39.3 Rationale
Although BCT is a good alternative in selected cases of PABC, larger tumors than those found in nonpregnant patients, associated with the fact that radiotherapy should be avoided until after delivery, result in a low rate for this kind of surgery in this group of patients [17]. In our breast unit there were no indications for BCT, since the dominant tumors were pT2 and pT3. Therefore, sentinel node biopsy was not used in PABC until some years ago, and all patients underwent axillary dissection.
Pregnancy affects all of the body. Physiological changes particularly associated with pregnancy include increased cardiac output, decreased peripheral vascular resistance, increased blood volume, physiological dilutional anemia, increased oxygen consumption, increased renal plasma flow, increased coagulability, decreased lung capacity, supine positional hypotension, and slow gastric emptying [15, 16]. They require special care from anesthesiologists and the surgical team (Table 39.1). So there are limits to consider in the extension of surgery in pregnancy.
Table 39.1
Physiological changes in pregnancy that can potentially affect breast reconstruction decisions and outcome
Physiological change | |
|---|---|
Blood volume | Increases by 30–50 % |
Hematocrit | 30–35 % of normal |
Heart rate | Increases by 10–15 bpm |
Clotting factors | Increase in the levels of fibrinogen, prothrombin, and factors VII, VIII, IX, and X |
White blood cells | 10,000–14,000 |
Platelet level | Low to normal |
With regard to breast reconstruction, pregnancy affects particularly the breasts, resulting in glandular hyperplasia and hypertrophy (mean breast weight normally doubles in pregnancy), increasing ptosis, areolar enlargement, nipple hypertrophy, and increasing pigmentation of the nipple and areola. At the end, breast anatomy is completely altered (Fig. 39.4). Unfortunately no data exist about the changes in breast structure, as well as volume and shape, and how they can affect the decisions regarding the best technique to use to reconstruct the breast in PABC. For that reason, some authors propose that breast reconstruction should be delayed until after delivery, when all reconstructive options are available (especially autologous tissue flaps), and when symmetry could be easier to achieve.
Fig. 39.4
a, b Aesthetic modifications in the breasts and body during pregnancy
However, nowadays, immediate breast reconstruction is widely preferred and does not have a negative influence on breast cancer survival rates or recurrences. It has innate advantages in terms of quality of life and aesthetic outcomes when compared with delayed reconstruction, especially for young women [20]. So our reconstructive approach to these patients in this series was to divide them into three different categories according to the phase of their pregnancy and body and breast modifications:
1.
First trimester. The breasts and body are modified little by pregnancy. The result of the reconstructed breast is more predictable than in the other two phases. Immediate reconstruction can be performed in one-step surgery with breast implants and contralateral symmetrization by breast reduction or mastopexy, or in two-step surgery with temporary breast expanders (Fig. 39.2). Autologous tissue flaps, especially those involving abdominal wall techniques (pedicled or free transverse rectus abdominis myocutaneous flaps), are contraindicated. A latissimus dorsi flap could be indicated in well-selected cases, but it increases both the surgical time and the clinical complications. In this series there were two patients who underwent immediate breast reconstruction through one-step surgery with a definitive implant and contralateral symmetrization, resulting in a good aesthetic result. There were no significant modifications in their breasts over time.









