Is This Technology Still Relevant?
In 2012, the author reviewed a series of patients who had undergone plasma skin resurfacing (PSR) with the Portrait PSR3 device,1 and concluded that plasma skin resurfacing was a relevant and worthwhile procedure for patients with Fitzpatrick skin types I through IV whose major complaints were hyperpigmentation and mild-to-moderate wrinkles everywhere on the face except the upper lip. Since that time, this author continues to use the technology; but its popularity has definitely waned. Fewer patients are willing to accept a week or so of downtime; and with the demise of the original manufacturer (Rhytec, Inc., Waltham, Massachusetts), the procedure has much less Internet presence. Hence, prospective patients are not as familiar with the technology. The new manufacturer of the technology (Energist Medical Group, Swansea, United Kingdom) can supply the necessary parts and service, but it has not reestablished the type of Internet and media presence seen with Rhytec. Downtime, the length of time from the day of the procedure to when a patient may return to relatively normal activity, is comparable to that for nonablative, fractionated carbon dioxide laser resurfacing. In the author’s practice, patients with wrinkles or scars deep enough to require a full ablative carbon dioxide laser resurfacing seem more willing to accept the necessary downtime than patients with lesser rhytids and hyperpigmentation. It is important, therefore, to ask if plasma technology is still relevant compared to chemical and laser technologies that have similar effects.
22.2 Historical Perspective
The Portrait PSR3 device is a class II nonlaser device that was designed to provide a quicker healing alternative to ablative laser treatments for patients with facial rhytids and hyperpigmentation. It was also considerably less expensive than many ablative lasers. Introduced into the U.S. market for cosmetic use by Rhytec in 2005, its launch preceded the launch of a number of fractionated laser devices by 1 or 2 years but was almost simultaneous with others. Its clinical relevance is most commonly compared to that of a fractionated carbon dioxide laser.
The device produces nitrogen plasma in its handpiece. Plasma is an ionized gas that is considered the fourth state of matter. Examples of where plasma is commonly observed in nature include some flat-screen television monitors, electrical storms, and the Aurora Borealis. In this device, an ultrahigh-frequency radio pulse vibrates a tungsten element in the handpiece that excites nitrogen molecules in a stream of nitrogen gas passing through the handpiece. It converts the stable nitrogen gas to unstable ionized nitrogen plasma. Nitrogen plasma is delivered to the skin in one or more passes in a technique similar to that of laser resurfacing (▶ Fig. 22.1).
Fig. 22.1 (a) The Portrait plasma skin resurfacing (PSR) device, and (b) a close-up of the delivery end of the handpiece system. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
The original Food and Drug Administration (FDA) approval for the device was for treating facial and nonfacial rhytids, acne scars, and superficial benign skin lesions such as seborrheic keratoses, viral papillomata, and actinic keratoses in Fitzpatrick skin types I through IV. The device is contraindicated in patients prone to keloid formation.
22.3 Comparable Technologies
Ablative and nonablative facial resurfacing techniques are designed primarily to remove wrinkles or scars and rejuvenate skin. Rejuvenate is a difficult-to-define term that can include the removal of wrinkles and scars and changes in color and texture of the skin. Some techniques are more efficacious for wrinkles and some are more efficacious for uniformity of skin color. Rejuvenation may also include improvements in overall brightness and luminescence of the skin that may be apparent in photos and in person but are very hard to measure. The various machines and chemical techniques available have varying depths of epidermal and dermal penetration. Virtually all these technologies claim to stimulate neocollagenesis. With the advent of aesthetic carbon dioxide and erbium laser technology in the mid-1990s, mechanical dermabrasion became less commonly used. Superficial, medium, and deep chemical peels are still common.
The principle by which medical lasers achieve their results is called photothermolysis. Each laser generates a collimated light of a single frequency that can selectively target a specific complimentary color or group of colors, target chromophores. For the carbon dioxide laser (10,600 nm) the primary target of the laser is water.2 The laser vaporizes skin cells in a very controlled and precise manner.
Lasers commonly used for skin rejuvenation are the 10,600-nm carbon dioxide laser, the 2,940-nm erbium:yttrium aluminum garnet (Er:YAG) laser,3 and the fractionated erbium 1,550- and 1,410-nm lasers.4 The depth of penetration for each laser depends on the wavelength of the target chromophore, the number of passes, and the amount of laser energy delivered. Typical depths of penetration for the carbon dioxide laser (10,600 nm) are 450 µm to 1 to 2 mm (although rarely used beyond 1 mm),2 for the Er:YAG (2,940 nm) laser 3 to 120 µm,3 and for the erbium fiber, diode (1,550 nm) 250 to 800 µm.4 By sparing specifically and uniformly spaced areas of untreated skin between targeted skin, fractional technology often provides the ability to treat skin with local or topical anesthesia and shorter postoperative downtime. Fully ablative laser treatments may require a few more days of downtime and may require more intraoperative analgesia or anesthesia. It is important to match the correct technology with the needs and desires of the patient. In skin resurfacing, the patient’s very specific goals, the genetic makeup of the patient’s skin, the depth and location of the wrinkles or scars, the amount of dyschromia, and tolerance for downtime are important factors in choosing the right technology. The amount of heat delivered to the skin and the depth of that heat penetration are major determinants of the amount of collagen neogenesis. In practice, it seems that around 40 to 44°C is needed for collagen neogenesis. This can also be accomplished to a lesser extent for mild wrinkles and loss of volume with a bipolar radiofrequency device and no downtime.
22.4 Histological Changes in Plasma Skin Resurfacing
The effect on collagen neogenesis and the mechanisms of healing with plasma skin resurfacing are directly related to the amount of energy delivered to the tissue.5,6 The histological changes with this device have been most thoroughly studied with delivered energy over 2 joules (J) (the PSR2, PSR3, and PSR2/3 protocols for the device).5,6,7,8 With energies less than 2 J, slough of the epidermis and treated dermis actually takes longer.
The distribution of heat in the tissue dissipates, according to a predictable Gaussian distribution. Typically, it penetrates to 500 to 600 µm in normally hydrated skin at energies over 3.0 J.7 This leads to two distinct, histologically visible areas in the skin, a so-called inner zone of thermal damage and an outer zone of thermal modification (▶ Fig. 22.2). Of particular note is that the epidermis (including the stratum corneum) remains largely intact.5,6 Over time, a line of cleavage forms between these two zones, along which the epidermis and dermis will separate as the skin regenerates. Higher energy leads to a deeper line of cleavage. There is none of the vaporization of tissue seen with a carbon dioxide laser. Protection of this epidermis postoperatively leads to a very predictable slough along the line of cleavage, usually beginning 4 to 5 days after the treatment in energies above 2 J. With energies below 2 J, this process can take 10 days or so.
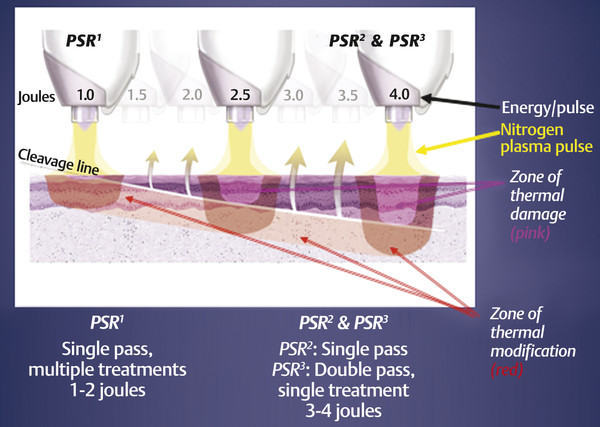
Fig. 22.2 Higher energy delivery leads to more depth of penetration in the zones of thermal damage and thermal modification, lowering the line of cleavage between the two zones deeper into the dermis. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
The preserved epidermis and stratum corneum act as a biological dressing. Heat distribution in the zone of thermal modification is sufficient to stimulate significant collagen neogenesis. ▶ Fig. 22.3 shows the early histological changes that occur in the epidermis and dermis with plasma energy applied at a typical treatment level of 3.5 J.
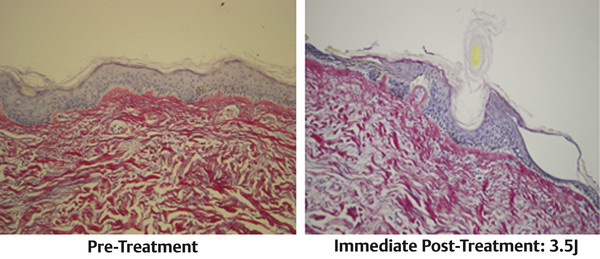
Fig. 22.3 The immediate effect of application of the nitrogen plasma is heating of the dermis and epidermis, leaving the stratum corneum intact. In clinical practice, the only smoke seen is from heating the hairs. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, MA, USA.)
Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.
At energies above 2 J, vacuole formation is a prominent feature in the histology.5,6,7 It is seen in some of the basal epidermal cells at the dermal-epidermal junction. The vacuoles appear to be air-filled spaces that insulate the dermis enough to permit a second pass of plasma without overheating the dermis to the point of irreparable damage. They seem to block deeper penetration of heat with the second pass.5,6,7 With increasing energy, the depth of the zones of thermal damage and thermal modification increases, but the second pass at energies over 2 J only fills in the gaps between previously treated spots. It gives a more uniform treatment but not a deeper treatment (▶ Fig. 22.4). A line of skin cleavage forms between a newly regenerated epidermis and old epidermis around day 4 or 5 (▶ Fig. 22.5). The beginning of skin slough on days 4 and 5 is very predictable, and we tell all our patients when to expect this phenomenon. By days 7 to 10 there has been complete remodeling of the epidermis, and collagen neogenesis has begun. There is intense fibroblast activity and neovascularization in the zone of thermal modification in the deep dermis that corresponds with the regeneration of the reticular architecture of the dermis. The zone of thermal modification in the upper papillary dermis is reactive. ▶ Fig. 22.6 is a polarized image that shows new collagen in the zone of thermal modification. These new collagen fibers assume their normal orientation perpendicular to the skin. Generally, this orientation is not seen with an ablative carbon dioxide laser treatment. By around 90 days, there is a very significant zone of collagen neogenesis at the dermal-epidermal junction (▶ Fig. 22.7).5,6,7,8 Collagen neogenesis can continue for up to 1 year.
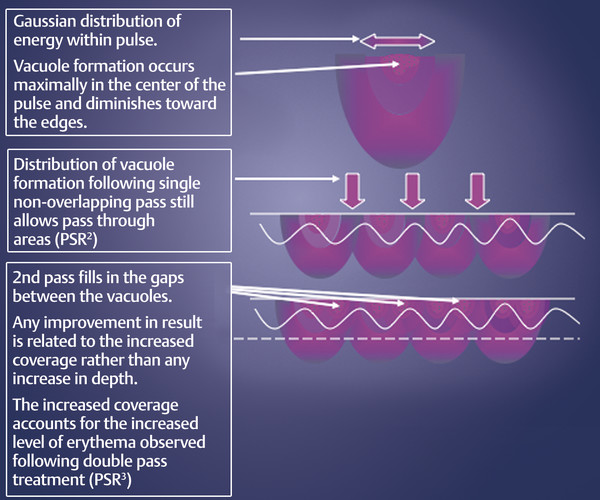
Fig. 22.4 Effect of a double pass with energies greater than 2 J (PSR3). (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
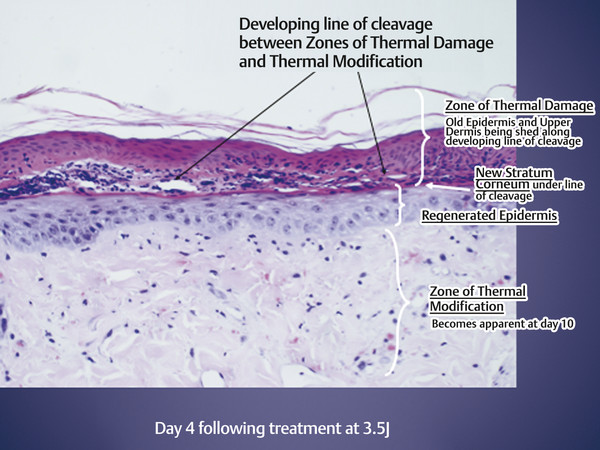
Fig. 22.5 Day 4 after a Portrait nitrogen plasma treatment with 3.5 J. Separation of old epidermis from the new epidermis along the line of cleavage that forms between the zones of thermal damage and thermal modification begins. Usually lasts until day 6 or 7. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
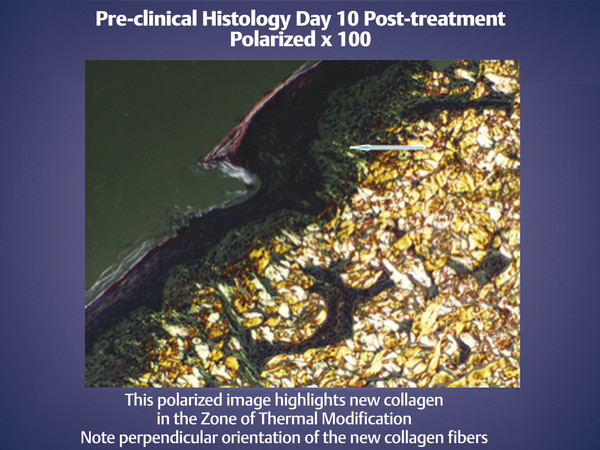
Fig. 22.6 Here a polarized image shows the collagen neogenesis. Much of the new collagen in the dermis is oriented perpendicular to the epidermis. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
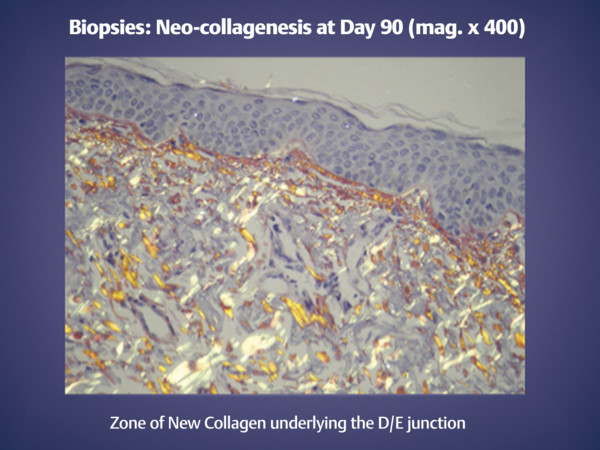
Fig. 22.7 Plentiful collagen neogenesis at 90 days, much of it perpendicularly oriented. D/E, dermal/epidermal. (Courtesy of NeoGen by Energist Medical Group, Swansea, United Kingdom; formerly Portrait, Rhytec, Inc., Waltham, Massachusetts.)
22.5 Plasma Resurfacing Technique
We have used this technology since 2006. Whether in a single treatment over 2 J (so-called high-energy treatment) or a multiple treatment approach at energies of or below 2 J (so-called low-energy treatment), there is well-documented collagen neogenesis; significant decreases in facial rhytids; and overall improvement in the general appearance of facial, neck, chest, and dorsal hand skin.5,7,8,9,10,11,12,13,14 Although it is claimed that plasma resurfacing can improve some acne scarring by as much as 34%,10 we have never been able to duplicate this result. We have also not found it useful for deep upper lip wrinkles.
Holcomb et al13 clearly demonstrated that plasma resurfacing, like carbon dioxide laser resurfacing, can be used simultaneously with facelift and cosmetic eyelid surgery in the properly chosen patient. They had specific recommendations for technique and energy levels.13 The technique recommendations of Lam and Tzikas14 published in 2008 are similar to ours.
22.6 Our Current Algorithm for Hyperpigmentation and Facial Rhytids
Whereas our objective is generally long-term efficacy, we also treat rhytids, dyschromia, and minimally depressed scars daily with temporary measures like botulinum toxin, superficial peels, and facial fillers. We treat dyschromia and facial rhytids with long-term measures that may include long-term skin-lightening regimens, Q-switched laser treatments, bipolar radiofrequency procedures, plasma skin resurfacing, fractionated carbon dioxide laser resurfacing, and ablative carbon dioxide laser resurfacing. ▶ Table 22.1 is our current algorithm for skin rejuvenation.
Rejuvenation needed | Skin type | Treatment |
Hyperpigmentation | Fitzpatrick skin types I–VI | Superficial skin peels (Fitzpatrick skin types I–III only), hydroquinone and tretinoin-based skin care products, Q-switched laser at 532 nm, or plasma skin resurfacing |
Mild rhytids around the eyes | Fitzpatrick skin types I–VI, wrinkle severity rating scale (WSRS) 1 and 215 | Bipolar radiofrequency |
Mild-to-moderate facial rhytids | Fitzpatrick skin types I–IV, WSRS 1 through 3 | Plasma skin resurfacing |
Fractionated carbon dioxide laser resurfacing may be recommended for the lower eyelids and crow’s-feet in conjunction with a transconjunctival lower eyelid blepharoplasty with fat transposition or as an isolated treatment. | ||
Mild-to-moderate facial rhytids + hyperpigmentation | Fitzpatrick skin types I–IV, WSRS 1 through 3 | Plasma skin resurfacing |
Moderate-to-severe facial rhytids | Fitzpatrick skin types I–III, WSRS 3 through 5 | Carbon dioxide laser resurfacing, fractionated and fully ablative |
Moderate-to-severe facial rhytids + hyperpigmentation | Fitzpatrick skin types I–III, WSRS 3 through 5 | Carbon dioxide laser resurfacing for deeper rhytids is sometimes combined with plasma skin resurfacing to areas with less deep rhytids for a more even, concomitant treatment of hyperpigmentation. |
Long-term follow-up therapy | We recommend long-term follow-up with tretinoin-based products and intermittent use of hydroquinone to maintain uniform skin color. About 50% of the patients adhere to these recommendations. |
22.7 Our Protocol for Plasma Skin Resurfacing
22.7.1 Skin Preparation
In accordance with the original manufacturer’s protocols, tretinoin or retinols are discontinued for 4 to 6 weeks before the treatment. We have not verified that this is actually necessary. Before recommending any resurfacing technique, a thorough family history and personal history of how a patient’s skin reacts to the sun, injury, and heat are important. Specifically, it is essential to determine the patient’s propensity for postinflammatory hyperpigmentation. In New England, we see many patients who appear to have Fitzpatrick skin type III with a significant propensity for hyperpigmentation. Patients of European lineage mixed with Native American ancestry and French Canadian lineage mixed with Native American ancestry are commonplace in New England. Although they may appear to have Fitzpatrick skin type III, we often treat these patients as we would patients with Fitzpatrick skin type IV (see specific treatment protocols in a subsequent section). Whereas we routinely pretreat our carbon dioxide laser resurfacing patients with tretinoin and hydroquinone, we typically treat our plasma resurfacing patients with just hydroquinone. We do not want to thin the stratum corneum. Patients are pretreated with 4% hydroquinone for 4 to 6 weeks before the procedure. Hydroquinone is restarted 7 to 10 days after the treatment. We typically restart tretinoin at 3 months postoperative.
22.7.2 Infection Prophylaxis
Viral and bacterial prophylaxis is similar to what we use for the carbon dioxide laser. All patients receiving perioral treatments are started on valacyclovir hydrochloride 1 gm daily for 7 days, starting the day of treatment for herpes simplex prophylaxis. All patients are placed on bacterial prophylaxis for 7 days starting the day of treatment. The incidence of methicillin-resistant Staphylococcus aureus in our community has led to a change from cephalexin prophylaxis to doxycycline or clindamycin in the last 2 years.
22.7.3 Anesthesia
We treat the majority of our patients using topical anesthesia or topical plus subcutaneous local anesthesia in our office procedure room. We also offer the patient 5 to 10 mg of oral diazepam and oxycodone 5 mg, 1 hour prior to the procedure. Our music or the patient’s choice of music plays the entire time the patient is in the treatment room. If a patient requests more sedation or general anesthesia, we do the procedure in the same-day surgery unit of our hospital. Our office is located in the same building.
22.7.4 Skin Preparation Day of Surgery
▶ Fig. 22.8 illustrates the application of topical anesthetic before the procedure and the grid used to ensure uniform treatment. Consistent with the original investigations, we hydrate the skin for 1 hour before the treatment with a topical anesthetic cream. If the patient is under general anesthesia, an occlusive ointment like Aquaphor (Beiersdorf Inc., Wilton, Connecticut) is just as good. Our current topical anesthetic cream of benzocaine, tetracaine, and lidocaine comes from a local compounding pharmacy and is a ratio of 20:10:10%. If treating without this period of hydration, the energy applied should be decreased about 30%, again consistent with the original Rhytec protocol.
For treatments of 2 J or less, topical anesthetic alone is usually sufficient.
For higher energy treatments over 2 J, we use regional blocks and direct infiltration with a total of 15 to 20 mL of 0.5% lidocaine, 1:200,000 epinephrine about 10 minutes before the end of the hydration period. The author blocks all three branches of the trigeminal nerve plus the entire length of the brows, an area of about 4 cm2 in front of the tragus, the entire lower eyelid, and about a 1.5-cm wide area along the mandible from the angle of the jaw to the mentum. For the upper lip, an upper dental block is placed, usually after a topical oral anesthetic gel like HurriCaine® (Beutlich Pharmaceuticals, Waukegan, Illinois).
After removing the topical anesthetic cream with a moist sponge, we draw the grid on the skin with a temporary marker to help ensure that the energy is delivered uniformly. Since this treatment is not chromophore-dependent, the marker can be any color.
< div class='tao-gold-member'>
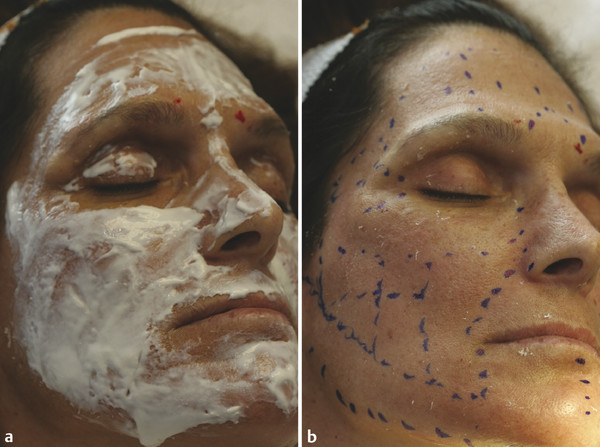
Fig. 22.8 (a) Topical anesthetic cream, and (b) grid to guide the treatment.
Only gold members can continue reading. Log In or Register to continue









