6 Nail and fingertip reconstruction
Synopsis
 Fingertip and nail bed injuries are the most common injuries of the hand.
Fingertip and nail bed injuries are the most common injuries of the hand.
 Common primary injuries include subungual hematomas, nail bed lacerations and fractures of the distal phalanx.
Common primary injuries include subungual hematomas, nail bed lacerations and fractures of the distal phalanx.
 Common secondary nail deformities seen after nail bed injury include nail ridging, splitting, nonadherence, absence, cornified nail bed, hook and spikes, or cysts.
Common secondary nail deformities seen after nail bed injury include nail ridging, splitting, nonadherence, absence, cornified nail bed, hook and spikes, or cysts.
 It is important to have a thorough understanding of the anatomy of the fingertip in order to adequately manage common injuries and deformities of the fingertip and nail.
It is important to have a thorough understanding of the anatomy of the fingertip in order to adequately manage common injuries and deformities of the fingertip and nail.
 The purpose of the current chapter is to provide the reader with a comprehensive review of the pathophysiology, diagnosis, and treatment of nail and fingertip injuries and their management.
The purpose of the current chapter is to provide the reader with a comprehensive review of the pathophysiology, diagnosis, and treatment of nail and fingertip injuries and their management.
Introduction
The perionychium develops near the end of the 1st trimester.1 A thickened area of epidermis on the dorsal distal phalanx of each finger and toe proximally invades the underlying dermis to form the nail groove. The deep layer of epidermal cells proliferates to form the nail matrix. Cells within the superficial layer of the nail matrix differentiate into hard keratin, forming the nail. At approximately 14 weeks, proliferation of the deeper layers of the nail matrix pushes the nail distally across the nail bed while firm attachment is maintained between the nail and nail bed.2 Folds of epidermis lateral and proximal to the developing nail form the nail folds. Nails reach the tips of the fingers and toes at about 32 and 36 weeks of intrauterine life, respectively.3
Basic science/disease process
Anatomy
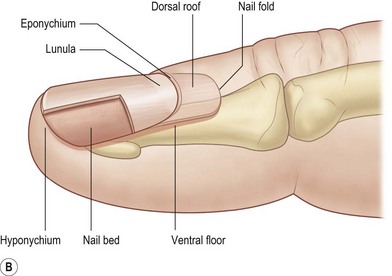
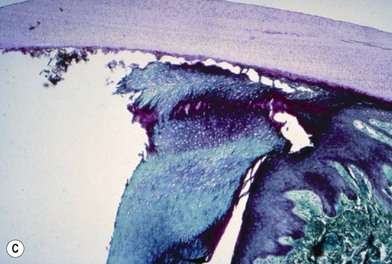
Topography of the nail was first described by Zaias.4 A standardized nomenclature for the anatomy of the nail was proposed by Zook et al.5 to improve communication between physicians regarding nail pathology, injury, and treatment (Fig. 6.1A,B). The entire nail structure, including the nail fold, paronychium, hyponychium, nail bed (germinal and sterile matrices), and nail, is referred to as the perionychium. The paronychium refers to the lateral skin surrounding the nail bed and nail. The skin over the dorsum of the nail fold is referred to as the nail wall. Extension of the nail wall distally onto the dorsum of the nail forms the eponychium. The eponychium is attached to the nail by a cornified material known as the nail vest, or cuticle. The white, convex opacity extending distally from beneath the eponychium is the lunula, which is the distal visible extent of the germinal matrix. The white color remains after removal of the nail and is thought to be secondary to retention of nuclei of the germinal cells to this level in the nail. The mass of keratin beneath the distal aspect of the nail and at the distal edge of the nail bed is the hyponychium (Fig. 6.1C).
Vascularity
The nail unit is supplied by branches of the common volar digital arteries. According to Flint,6 the digital arteries form three arterial anastomoses over the dorsal surface of the distal phalanx. A superficial arcade supplies the nail fold, and proximal and distal arcades wrap around the waist of the distal phalanx to supply the sterile matrix as well as the pulp space. On dissection of 10 amputated digits, Zook et al.5 found two consistent dorsal arterial branches of the digital arteries. The first branch was seen at the base of the nail fold and the second branch at the level of the lunula. Venous drainage of the perionychium coalesces laterally and dorsally, proximal to the nail fold, drains in a random fashion over the dorsum of the digit, and becomes large enough for vessel anastomosis at the level of the distal interphalangeal joint.7
Lymphatics roughly parallel the veins and are most numerous at the free edge of the nail (hyponychium). The density of hyponychial lymphatics is greater than in any other dermal area of the body.8 This explains the low subungual infection rate, considering the heavy exposure of the hyponychial region to pathogenic organisms with use of the nails and fingertips to scratch frequently contaminated areas.
Nerve supply
The common volar digital nerves branch dorsally, just distal to the distal interphalangeal joint, to supply the perionychium. Zook et al.5 reported the most common distribution of branching (70%) to be a proximal fascicle into the deep nail bed at the level of the lunula and a distal branch to the hyponychial area. Wilgis and Maxwell9 reported innervation by three nerve branches including two dorsal branches, as well as a branch to the pulp.
Physiology
Nail growth averages about 0.1 mm a day,4,10 and fingernails grow faster than toenails at a rate of 4 : 1.11 The rate of growth changes by season (growth is increased in the summer) as well as by age (growth is twice as rapid before the age of 30 years than after 80 years).11 Nail growth is also affected by comorbid conditions of the individual, including endocrine, vascular, infectious, and nutritional disorders.12 The rate of complete nail progression from the nail fold to the free margin has been reported to be between 70 and 140 days.4 Baden10 described a 21-day delay in growth after injury, during which time the nail thickens proximally but does not grow distally. Distal growth of a thicker than normal nail proceeds for the next 50 days; followed by growth of a thinner than normal nail for 30 days. Therefore, it is normal for an injury-induced lump to be present on the growing nail. Nail growth is not normal for approximately 100 days after injury. The nail is not fixed to underlying tissues by some mysterious glue but is fixed by virtue of its being a continuous chain of cells from the germinal layer into the nail, each cell attached to the one in front, behind, and beside it.
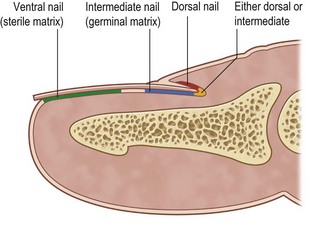
The nail is produced by cells from three areas of the perionychium: the germinal matrix, the sterile matrix, and the dorsal roof of the nail fold (Fig. 6.2). The germinal matrix produces the majority of the nail volume (90%) by gradient parakeratosis.4 The sterile matrix and the dorsal roof of the proximal nail fold produce the remaining nail cells. The sterile matrix adds cells to the volar surface of the nail, accounting for the attachment of the nail to the matrix. The addition of ventral nail during distal growth usually results in a thicker nail distally and compensates for the dorsal wear.13,14 There are longitudinal ridges in the sterile matrix that increase the surface for attachment. The dorsal roof of the nail fold adds flattened cells to the dorsal surface of the nail, producing the shine of the nail.15 Loss of the dorsal roof causes a dull-appearing nail.
Function
The function of nails was described in 1724 as “weapons to defend us from trouble … from small creatures, that often make their habitation upon our bodies and to allay the uneasy titillation by scratching.”13 Accordingly, fingernails are used for scratching as well as in defense. The nail protects the fingertip and contributes to tactile sensation.16 Counterpressure between the nail and the volar skin and pulp aids in delicate and precise touch. Picking up small objects is difficult if the nail is absent. Two-point discrimination will frequently double when the nail is lost. Incompletely attached or split nails are often painful, especially in individuals who work with their hands.
Acute injury
Epidemiology
Injury to the fingertip and nail bed is the most common injury of the hand because of their prominent position.17 The long finger is the most commonly injured, followed by the ring, index, and small fingers and the thumb with equal frequency bilaterally. The majority of injuries occur between the ages of 4 and 30 years; 75% occur in males.17 Fractures of the distal phalanx are present in 50% of nail bed injuries, and most injuries occur to the middle or distal third of the nail bed.
Injury is caused by a deforming force, which compresses the nail bed between the nail and the distal phalanx. A subungual hematoma results from injury to the nail bed, causing bleeding beneath the nail. The most common injury to the nail bed is the simple laceration (Fig. 6.3A).17 A simple laceration is common when the object causing the injury is small or sharp. The stellate laceration (Fig. 6.3B) is seen after compression with larger objects causing a bursting injury. Severe crush of the nail bed (Fig. 6.3C) is commonly caused by a wider, greater force of compression. Avulsion injuries (Fig. 6.3D) are the least common.17
Subungual hematoma
Treatment/surgical technique
Therefore, whether a subungual hematoma should be drained with the nail left intact or the nail removed and the nail bed repaired is debatable. In the past, removal of the nail for inspection of the nail bed with repair as needed was advocated for hematomas undermining more than 25% of the nail. Simon and Wolgin18 examined the nail beds of 47 patients presenting to the emergency department with a subungual hematoma and found that a hematoma >50% had a 60% incidence of laceration requiring repair. Repair of the nail bed was advocated with a hematoma >50% and an associated distal phalanx fracture. At the University of Pittsburgh, a 2-year prospective, observational study was designed to examine the outcome of 48 patients with subungual hematomas treated with drainage alone. No complications of nail deformity were found with this treatment, regardless of the size of hematoma or presence of fracture.19 Roser and Gellman20 compared three treatment groups in a prospective study of 52 children with subungual hematomas. A total of 26 fingers were treated with nail removal and repair of the nail bed. Drainage only was performed in 11 fingers, and 16 of 27 fingers were observed. No notable difference in outcome was found between the groups, regardless of hematoma size. It was concluded that nail removal and nail bed exploration are not justified in children with subungual hematoma with an intact nail and nail margin. Leaving the nail in place is recommended for most subungual hematomas with an intact nail. Exceptions may include children or patients with concern for an optimally aesthetic nail. If the nail is broken or the edge disrupted, removal of the nail and exploration of the nail bed are advised.
Lacerations
Treatment/surgical technique
Meticulous repair of the more complex stellate laceration and crush injury is more difficult. The severe crush injury may appear to be missing fragments. However, these fragments are often present, attached to the undersurface of the nail. Small fragments should be gently removed with a periosteal elevator and used as a nail bed graft. A split- or full-thickness nail bed graft up to 1 cm in diameter will usually survive, even when it is placed directly on the distal phalanx cortex.6 Blood supply to the graft is established by inosculation and vascular ingrowth from the periphery.
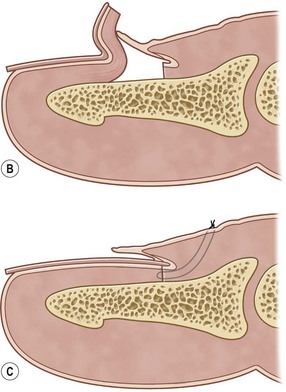
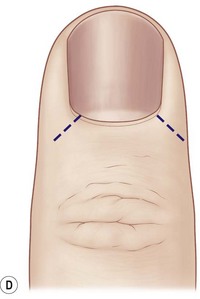
Avulsion of the bed often occurs at the level of the germinal matrix and proximal nail fold, leaving a distally based nail bed flap of germinal or sterile matrix (Fig. 6.4A). The nail bed remains attached to the nail, avulsing the germinal matrix off the bone and out of the nail fold (Fig. 6.4B). The nail and germinal matrix must be separated and the germinal matrix replaced and sutured back into the nail fold (Fig. 6.4C). The nail fold is exposed with unilateral or bilateral incisions perpendicular to the lateral corners of the eponychium. The incisions should be made at a 90° angle to the eponychium to prevent a notch deformity (Fig. 6.4D). If the laceration occurs at the junction of the ventral and dorsal roof of the nail fold, suture approximation may not be possible. In this case, a horizontal mattress stitch is placed through the proximal end of the avulsed nail bed and brought out through the nail wall. This will secure the nail bed within the nail fold. The eponychial incisions are then reapproximated with 5–0 or 6–0 nylon after nail bed repair.
Loss of small areas of nail bed may be replaced with split-thickness nail bed grafts from adjacent uninjured nail bed, harvested carefully with a No. 15 scalpel blade (Fig. 6.5A,B). A split-thickness nail bed graft may be harvested from an adjacent noninjured finger (risky) or an amputated finger. A split toenail bed graft may also be used acutely and avoids the possible deformity of an adjacent nail (Fig. 6.5C–H).21
On completion of the nail bed repair, the nail is removed from the povidone-iodine solution and a hole made in the nail away from the site of injury. The hole allows drainage of the subungual space after reinsertion of the nail into the nail fold. The nail is placed within the nail fold to mold the edges of the repair, to act as a splint for tuft or phalangeal fractures, to prevent formation of synechiae between the nail fold and the injured nail bed, and to protect the tender fingertip. The nail is held in place with a 5–0 nylon suture placed distally through the nail and hyponychial region. On rare occasions with severe injury to the fingertip, a mattress suture may be placed proximally through the nail fold. If the nail is not available or is in small fragments, a piece of silicone sheeting (reinforced 0.020-inch-thickness Silastic) may be shaped to fit beneath the nail fold and secured proximally through the nail fold (Fig. 6.6). Unlike the nail, the Silastic sheet is soft and easily slips from beneath the nail fold if it is secured only distally. Non-adherent gauze may also be placed within the nail fold if no nail or silicone sheet is available.

Fig. 6.6 An example of a stitch in the silicone sheeting to hold it in place.
(© Southern Illinois University School of Medicine.)
Distal phalanx fractures
Diagnosis/patient presentation
Distal phalanx fractures are found in approximately 50% of nail bed injuries and result in a higher incidence of secondary nail deformities.17 Therefore, radiographs of the distal phalanx are recommended.
Treatment/surgical technique
Treatment of nondisplaced distal fractures consists of nail bed repair and replacement of the nail. The nail acts as an excellent splint for the fracture. Small, displaced tuft fractures and most stable distal fractures can be reduced with reapproximation of the nail bed and replacement of the nail. Larger displaced fractures or unstable fractures require longitudinal or cross K-wire fixation. Care must be taken to put the pin in the medullary cavity of the bone (see Fig. 6.9).
Nail ridge
Introduction
Nail ridges are secondary to an irregularly healed distal phalanx fracture or scar within the nail bed. Nail ridges may also be secondary to a K-wire placed between the sterile matrix and the periosteum on reduction of a phalanx fracture (Fig. 6.7). Longitudinal irregularities result in longitudinal ridges or grooves. Transverse irregularities beneath the nail bed result in corresponding transverse grooves or ridges or distal nonadherence. Correction of this deformity requires excision of the scar or irregular bone edge to form a flat, smooth nail bed surface.6,16 A defect that cannot be reapproximated primarily requires use of a nail bed graft.
Split nail
Introduction
A split nail is often secondary to longitudinal scarring of the germinal or sterile matrix. Unlike the germinal and sterile matrices, the scar does not produce nail cells, resulting in splitting of the nail. Scar within the germinal matrix can split the nail from its most proximal aspect. Scar within the sterile matrix disrupts the progressive addition of nail cells to the volar nail, leading to detachment of the nail plate (Fig. 6.8). Other causes of split nails include bone spurs beneath the nail bed, eponychial pterygium resulting from failure of the dorsal roof matrix to detach from the nail, and scar formation between the dorsal roof and ventral floor of the nail fold. Although longitudinal splits are most common, a horizontal split has been reported; it caused a diagonal scar in the matrix and formation of a portion of the nail on each side (Fig. 6.9). The nail was produced within both folds, forming a horizontally split nail.
Treatment/surgical technique
Scar must be minimized to allow normal nail production. Scar within the sterile matrix can occasionally be treated with excision and primary closure. The excised defect is frequently too wide to be approximated without tension and requires repair with a split-thickness sterile nail bed graft from the same digit or a toe. In germinal matrix injuries, Johnson22 recommended releasing incisions in the lateral paronychial folds with bilateral central advancement of the germinal matrix, but the authors’ experience with this technique has been disappointing in traumatic deformities. Replacement of germinal matrix with sterile matrix will not be successful because sterile matrix grafts do not produce a nail. Split-thickness germinal matrix grafts also do not produce hard nail growth. The germinal matrix defect requires repair with a full-thickness germinal matrix nail bed graft.21,23 The second-toe germinal matrix is a good option with its similar shape and size; the large toe is a second choice (Fig. 6.10). The patient is warned that use of the toenail germinal matrix will eliminate hard nail growth on the toe. This second-toe nail defect is frequently more acceptable to patients than a defect of the great toenail. In the case of an existing bone spur, the nail bed is lifted free and the spur is removed with rongeurs to produce a flat surface, and the nail bed is replaced.
Pterygium
Splitting of the nail may also be caused by a pterygium. A pterygium of the eponychium results from adherence of the eponychium or dorsal roof of the nail fold to the nail plate or nail bed during healing. A web between the eponychium and nail bed will result in splitting of the nail as it grows distally from the nail fold (Fig. 6.11).
Nonadherence (onycholysis)
Introduction
Nonadherence of the nail is the most common nail deformity after trauma and is often found distal to transverse or diagonally oriented nail bed scars or bone irregularities. The most common cause of nonadherence is nail bed scarring. The scar interrupts the progressive addition of nail cells from the sterile matrix to the volar nail plate, causing detachment of the nail. The nail is unable to reattach to the nail bed distally.24
Treatment/surgical technique
Nonadherence secondary to a nail bed scar is corrected with scar excision and primary closure or closure with a split-thickness sterile matrix graft from the adjacent nail bed or toenail bed.24–
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree