Fig. 38.1
(a, b) Preoperative 32-year-old patient who underwent a secondary aesthetic surgery for bilateral capsular contractures after retroglandular silicone gel prosthetic mammoplasty (McGhan Anatomic, 270 mL). (c, d) Six months postoperative after capsulotomy was performed to eliminate the thick capsule and to replace a second implant (Mentor, CPG Plus Tall, 270 mL)
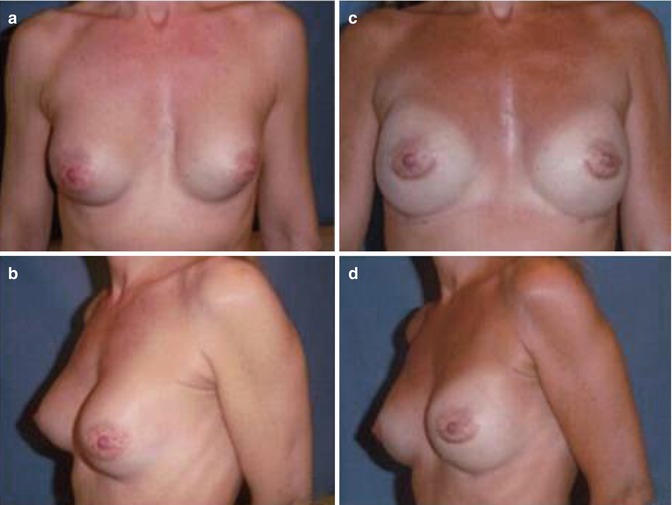
Fig. 38.2
(a, b) Unnatural aspect of a capsular contracture in a 35-year-old woman, 10 years after the insertion of subglandular implants (Trilucent, 210 mL). (c, d) One year postoperative after revision augmentation (Mentor, CPG 312, 245 mL) showing greater mammary symmetry and an overall improvement of the breast shape
38.6 Breast Expanders
The technique of tissue expansion, introduced by Radovan in 1982 [37] and later developed by Argenta, paved the way for the use of implants for breast reconstruction and is still considered the standard procedure in breast reconstructive surgery. Breast expanders are temporary implants consisting of an expandable casing of silicone which encloses an empty chamber that is filled, by a valve (easily available through the skin with a system of magnets), of saline at the time of surgery and during the postoperative period according to a predetermined protocol time [38]. The final volume of the “expanding” breast must be 30 % greater than the healthy one. It is common to maintain the excess of volume for at least 3 or 4 months in order to counteract the elasticity of tissues (including the periprosthetic capsule) that inevitably tends to bring the breast to the original volume. Expanders are placed under the pectoralis major muscle and under the medial border of the serratus muscle. They allow modulating the size, shape, and projection of the reconstructed breast through a progressive expansion over time.
These principles can be used both in the immediate reconstruction after mastectomy, that is, in deferred ones, in order to gradually stretch the skin-muscle tissue to insert implants of larger volumes. This procedure, of course, requires a secondary surgery, but results are satisfactory: it not only allows a more precise choice of the size but, through a progressive expansion, prevents the abnormal tension of muscles and skin covering the implant. The technique consists of two stages: the first one is the positioning of the expander a second time; after the expansion of soft tissues, the expander is replaced with the permanent implant; in the same operative session, the simultaneous adjustment of the contralateral breast is often performed.
Today, textured surface expanders (developed by Maxwell in the 1990s) are the most used; the valve is contained within the casing. The volume ranges from 300 to 1,000 mL.
The texturing of the surface tends to reduce the capsular periprosthetic reaction and allows a more rapid adhesion to the surrounding tissue, preventing its displacement (the presence of pores induces fibroblasts of surrounding tissues to grow above, preventing harmful displacements). This procedure is indicated for all those patients undergoing mastectomy presenting superficial soft tissues of good but insufficient quantity [39].
The aims of the mammary skin expansion are:
1.
Functional: progressive expansion of the skin (“skin recovering”) to make possible the positioning of a definitive prosthesis
2.
Aesthetic: restore a more natural morphology after mastectomy
Nowadays industries commercialize prosthesis expanders of Becker (introduced by Becker in 1987 [40]) that, once the desired expansion is achieved, are permanently left on-site, in order to avoid the replacement of a secondary implant. These implants consist of a double room: the outer one contains a non-expandable silicone gel, while the inner chamber can be inflated with saline, gradually expanding to the final desired volume.
38.7 Breast Implants
All breast implants are composed of a silicone casing containing a soft and flexible gel, such as silicone, or liquid (saline), or both:
38.7.1 Prosthesis with Salt Solution
Inside the silicone casing, there is a sterile saline solution. There are different types of implants in saline, which differ primarily in prosthesis prefilled with a determined volume, prosthesis that can be filled during surgery, or finally prosthesis with filling volume that can be modulated over time.
These implants appear to be associated with a lower incidence of capsular contracture, and because they are filled after the insertion, they can be implanted through smaller incisions.
38.7.2 Prosthesis with Silicone Gel
These have a shell of silicone elastomer filled with a silicone gel that corresponds to different degrees of cohesiveness to make them more or less soft. The most widespread are filled with high-cohesive silicone of IV generation that, even in case of breakage, does not expand and soak up at a systemic level (as it happened with old implants) and also minimizes the risk of deformation and displacement. In fact the silicone gel has a very similar viscosity to human fat, the largest component of the female breast tissue. They are distinguished by filling mode, and some can be retouched in volume after a few months since surgery, but it is usual to choose a type of prefilled and sealed system. In April 2006, they received from the American FDA (Food and Drug Administration) the approval to be marketed in the United States but only for two companies that have passed several steps required by the Board of Supervisors [41]. They are currently used in about 90 % of interventions.
38.7.3 Form of Prosthesis
In addition to the structures and features of materials, breast implants can be divided according to the form:
38.7.3.1 Round
These have been used for almost half a century, and they have a symmetrical shape with a rounded base on the chest and a dome-shaped appearance. There are several volumes, diameters, and different projections (low, medium, and high profile). There are no preformed implants and their shape, once implanted, is affected by the force of gravity and by the pressure of surrounding tissues.
38.7.3.2 Anatomical
They have been introduced since about 20 years to be used in post-mastectomy reconstructions, when it is useful to restore the anatomical shape of the mammary gland, previously removed. They have an asymmetric shape with a basic oval of different possible widths and heights and a predefined shape with a greater projection of the lower poles than the upper ones. This preformed “drop” aspect is made possible by using an internal highly cohesive silicone gel, more rigid, which enables the prosthesis to maintain its original shape and to be less affected by the force of gravity and the pressure of surrounding tissues.
38.7.4 Prosthesis History
The first prosthesis produced in the 1960s had a smooth surface; during the mid-1970s, breast implants covered with a micropolyurethane foam were introduced, particularly suitable for the use after radiation treatments that have not left clinical signs of tissue damage and the prevention of recurrence of periprosthetic capsule contracture [42]. Unfortunately the polyurethane tends to dissolve in a few years in microparticles; it is phagocytosed by macrophages, and this results in an intense inflammatory reaction.
At the end of the 1980s, a new generation of textured surface breast implants appeared.
Their wrinkled consistency allows for greater adhesion to tissues and promotes the formation of a more favorable, less thick, and less contracted periprosthetic fibrous capsule. In fact the frequency of the capsular contracture also depends on the type of surface coating the implant. Numerous scientific studies have shown that textured breast implants have a lower risk of capsular contracture than those with smooth surface (Fig. 38.3) [43].


Fig. 38.3
Old breast implants removed after radial and tangential capsulotomy in a woman presenting an evident capsular contracture
38.8 Periprosthetic Fibrous Capsule
Our body reacts against breast implants with the formation of a fibrous capsule which surrounds them completely. It is a real chronic inflammatory reaction to a foreign body with the production of a fibrous tissue rich in collagen fibers and cells of chronic inflammation, in the interface between the implant and the host [44]. It is a kind of internal scarring, which consists in the production of a species of endothelium in contact with the prosthesis; this “natural casing” plays a protective role because it insulates implants from the rest of the body and stabilizes them in the correct position.
In fact, in case of rupture, the dense barrier constituted by it prevents the rapid gel spread to neighboring tissues (Fig. 38.4).
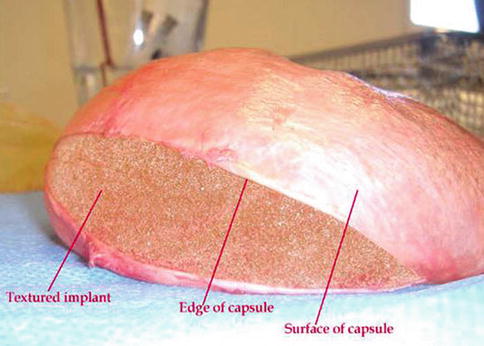
Fig. 38.4
Periprosthetic fibrous capsule surrounding a textured surface breast implant
From a histological point of view, the capsule is composed of many types of cells, including fibroblasts, which shall form the collagen matrix, but also macrophages, various inflammatory cells, and vascular cells; if there are irritative factors, consequent chronic inflammation tends to make fibroblasts contractile, stimulating the production of growth factors, which provide them with a trophic support. They are thus transformed into myofibroblasts, whose contraction, together with the production of abnormal collagen, contributes significantly to the narrowing of the capsule [45].
In fact, over time the capsular tissue tends to increase in thickness and contract to fit around the implant with a speed that depends in part on the type of prosthesis and in part on the individual reactivity and effectiveness of the host immune system. The origin of this complication has not yet been fully clarified, although it is believed that it is multifactorial.
A study published in 2010 [46] shows that the severity of capsular contracture is closely associated with a significant increase in gene expression of TNF-α, highlighting its key role in the periprosthetic inflammation. Therefore, periprosthetic capsular fibrosis represents one of the most common adverse reactions in the medium and long term in aesthetic and reconstructive surgery.
Causing displacement, visibility of the implant, sense of tension, pain, and hardness on palpation, it accounts more than 30 % of all surgical revisions after the first surgery. Nevertheless the evolution of materials and techniques used for breast surgery has significantly decreased this phenomenon.
Other principals, frequently used in reducing capsular fibrosis, are anti-inflammatory drugs, especially derivatives of cortisone, used both intraoperatively and in the postoperative period in the short and medium term [47]. Finally, starting in the early 2000s, a lot of excitement has been created around the use of anti-asthma leukotriene antagonists (Zafirlukast, Accolate), which showed promising preventive effects of capsulitis [48] and are routinely used mainly in aesthetics.
38.9 Experimental Procedure: MSCs and MCF-7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








