■ If done correctly, there is minimal risk associated with this technique. The main risk of this procedure occurs if the injection is done too deep. If injected too deep into the neck, branches of the brachial plexus can be anesthetized, and the patient may have a temporary paralysis of the ipsilateral upper extremity. A deep injection can also anesthetize the phrenic nerve and lead to temporary diaphragmatic paralysis. For this reason, if the injection is being done without general anesthetic while the patient is awake, it is important that bilateral blockade is not performed simultaneously on both sides of the neck. Finally, if the injection infiltrates superiorly, the greater auricular branch of the plexus will be blocked, and the patient will have numbness of the skin overlying the parotid and the earlobe. This is a common side effect that the patient should be told to be aware of in the immediate postoperative period.
TECHNIQUES
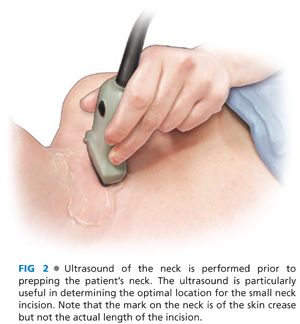
■ Optimal positioning for parathyroidectomy is with the patient’s neck gently extended but well supported. Prior to prepping the skin, we routinely perform an intraoperative ultrasound of the neck to ensure the choice of the optimal location for the skin incision (FIG 2). In addition, intraoperative ultrasound often allows the surgeon to confirm the location of the adenoma and focuses the subsequent surgical exploration.
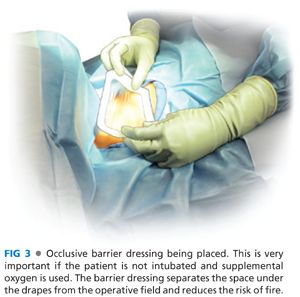
■ After prepping the skin, it is critical that if the patient has not received a general anesthetic, care must be taken when placing drapes to ensure that the operative field is fully separated from the space below the drapes. Patients who are receiving sedation and local anesthesia usually are also given supplemental oxygen by the anesthesiologist during the operation. This is commonly done with nasal cannula and results in relatively high oxygen concentrations below the drapes. If that oxygen comes in contact with a spark from electrocautery used during the performance of the parathyroidectomy, the risk of fire is increased. For this reason, when draping the patient, an occlusive dressing or adherent drapes are important to separate the operative field from the space below the drapes (FIG 3).
■ A small (2 to 3 cm) incision in the midline is made in a skin crease. Although some surgeons prefer an incision shifted toward the side of the parathyroid adenoma, we prefer using a midline incision so that if it becomes necessary to explore both sides, the same incision can often be used. If it is necessary to lengthen the incision, this is usually only a minimal increase in incision size.
■ Small subplatysmal flaps are created with electrocautery to allow the skin incision to be moved up or down depending on where the abnormal gland is located. The midline strap muscles are then separated in the midline so that the thyroid lobe on the involved side can be rotated medially (FIG 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








