Minimal Access Le Fort III Osteotomy for Midface Hypolasia
Scott J. Rapp
Christopher B. Gordon
DEFINITION
Midface hypoplasia can lead to significant aesthetic and functional airway compromise.
Le Fort III distraction osteogenesis is a useful surgical approach to address hypoplasia and facial dysmorphism at skeletal maturity or when severity of symptoms warrants earlier intervention.
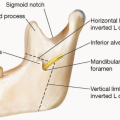
A Le Fort III approach involves osteotomies to the floor/lateral/medial wall of orbit, nasal bones, zygomaticofrontal suture, pterygoid plates of sphenoid, ethmoid, zygomatic arch, and posterior wall of maxillary sinus.
ANATOMY
Midface hypoplasia (FIG 1) is characterized by:
Facial disharmony
Malar deficiency and concavity to profile
Exorbitism, lack of globe protection
Class III occlusion
Posterior airway space (PAS) narrowing
Dental crowding
PATHOGENESIS
Events leading to severe craniofacial skeletal dysplasia are likely multifactorial but are believed to be associated with abnormalities in neural crest cell development and migration.1
Most are associated with genetic syndromes, but occasionally they may be sporadic.2
Midface sutures such as the spheno-occipital suture may prematurely fuse leading to growth disturbances.3
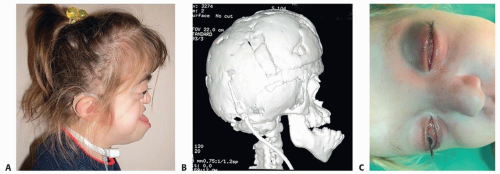
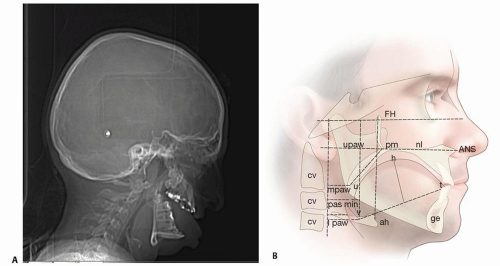
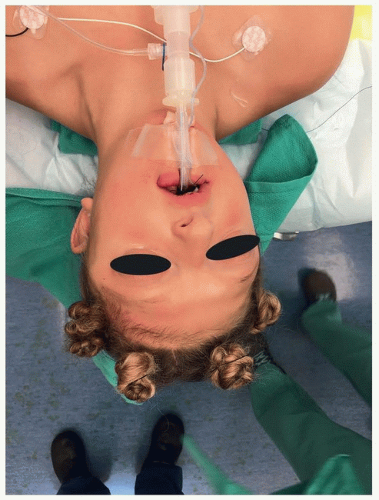
FIG 1 • Midface hypoplasia can have profound effects on projection (A), occlusion and airway (B), and eye protection (C).
Genes associated with midface hypoplasia are the fibroblast growth factor receptor genes (FGFR2, FGFR3), twist-related protein gene (TWIST), and treacle ribosome biogenesis factor 1 gene (TCOF1).1
Midface hypoplasia is often observed with concomitant craniosynostosis, most often with bicoronal synostosis seen in syndromic patients:
Apert (FGFR2)
Crouzon (FGFR2)
Saethre-Chotzen (TWIST)
Meunke (FGFR3)
Other syndromes leading to maxillary hypoplasia include Treacher Collins syndrome and craniofacial microsomia (hemifacial microsomia, Goldenhar syndrome).
Neurologic dysfunction may be present including:
Hydrocephalus/ventriculomegaly
Gyral abnormalities
Hypoplastic/heterotopic white and gray matter
Corpus callosal agenesis
Kleeblattschadel/megalocephaly
NATURAL HISTORY
Surgical approaches to the midface in syndromic patients were first reported by Gilles in the 1950s and then advanced through Paul Tessier’s work in the 1960s.4
Midface osteotomies have been historically performed at skeletal maturity to prevent undergrowth or reduce relapse rates.
However, distraction techniques provide greater bony movements and more structural stability at an earlier age to address life-threatening airway compromise and ocular exposure.
PATIENT HISTORY AND PHYSICAL FINDINGS
Clinical exam findings may include
Midface retrusion
Craniosynostosis
Exorbitism/shallow orbit
Keratitis/corneal ulcers
Lagophthalmos/scleral show
Orbital hypertelorism
Class III occlusion
Anterior open bite
Narrow arch/dental crowding
IMAGING
Cephalometric consideration for PAS (FIG 2A)
Nasopharynx
Pterygomaxillare (pm) to posterior pharyngeal wall (upaw)
Oropharynx
Tip of uvula (U) to posterior pharyngeal wall (mpaw)
Hypopharynx
Tongue base (V) to posterior pharyngeal wall (lpaw)
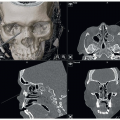
Plain film/CT exam findings (FIG 2B)
Shallow orbits
Hypertelorism
Exotropia
Bicoronal synostosis—brachycephaly
Choanal stenosis/atresia
DIFFERENTIAL DIAGNOSIS
NONOPERATIVE MANAGEMENT
Severe midface hypoplasia observed in syndromic newborn may require early nonsurgical management.
Airway compromise may be managed with:
Prone positioning
Positive pressure ventilation or assistance
Mandibular distraction for concomitant tongue-based obstruction
Globe protection
Taping
Eye lubrication
SURGICAL MANAGEMENT
A multidisciplinary team is required for optimal surgical intervention, including:
Plastic surgery/oral surgery
Orthodontics
Genetics
Dentistry
Ophthalmology
Speech pathology
Otolaryngology and audiology
Social work and psychology
Preoperative Planning
Planning between surgeon and orthodontist is critical to optimize the desired end point of centric occlusion.
Virtual surgical planning (VSP) or model surgery assists in anticipated distance and vectors for distraction.
Stereolithic models can assist with identification of permanent teeth and root location.
Patient may require palatal expansion prior to Le Fort III osteotomy.
Maxillary third molars may be removed prior to intervention; secondary Le Fort I osteotomy is anticipated to obtain class I occlusion.
An ophthalmologic evaluation is required to assess for corneal ulceration and abrasion and to identify preoperative visual dysfunction (ie, strabismus, exotropia, V-pattern esotropia/exotropia).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree