CHAPTER 19 Midface lift
History
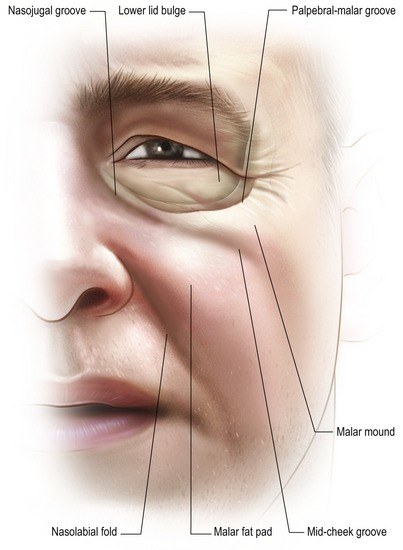
Surgical rejuvenation of the midface remains a challenging concept in facial aesthetic surgery. An appreciation of age-related changes that occur in this region allow the surgeon to develop a comprehensive operative plan in an effort to restore a youthful, well-contoured midface. The hallmarks of midface aging, which include descent of the lid–cheek junction, formation of the nasojugal groove and deepening of nasolabial folds, are caused by a myriad of factors (Fig. 19.1). Most notably, these include structural ligamentous laxity, soft tissue descent, malar fat pad ptosis and facial volume loss. As these anatomical changes became elucidated, surgeons have evolved various techniques to address release of the soft tissues of the central face with subsequent resuspension.
Physical evaluation
• Lower eyelid shape. Evaluation includes assessment of medial to lateral canthal tilt as well as the relationship of the lid to the lower corneal sclera limbus.
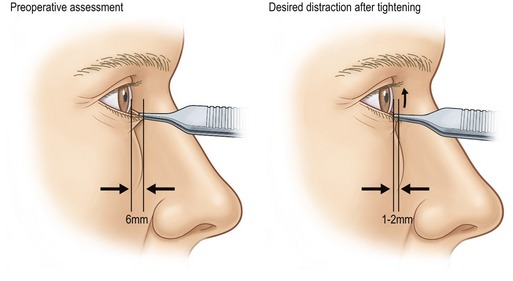
• Lower lid tone. As aging occurs, tarsoligamentous laxity will lead to loss of lid tone. Lid snap back and distraction tests are helpful in this assessment (Fig. 19.2).
• Volumetric analysis. Assessment of excess orbital fat, skin or muscle as well as its relationship to the lid–cheek junction will provide a guide for treatment of the orbital retaining ligament as well as fat excision and/or repositioning.
• Tear trough deformity. Assessment of the ligamentous attachments medially and the nasojugal groove are important in planning the extent of medial dissection and/or fat repositioning.
• Midface descent and/or deflation. Analysis of descent of the SOOF (suborbicularis oculi fat), malar fat pad, and/or the development of malar bags or festoons determine the extent of supra- or sub-periosteal dissection.
• Nasolabial or midface fold. The nasolabial fold deepens as cheek soft tissues descend over the nasolabial retaining ligament. The lateral oral commissure may also migrate inferiorly with increased laxity of the upper lip elevators.
• Skin analysis. Evaluation of photoaging, including skin elasticity, rhytids, and hyperpigmentation will guide the extent of skin resection as well as the utility of adjunctive therapies such as peels or laser.
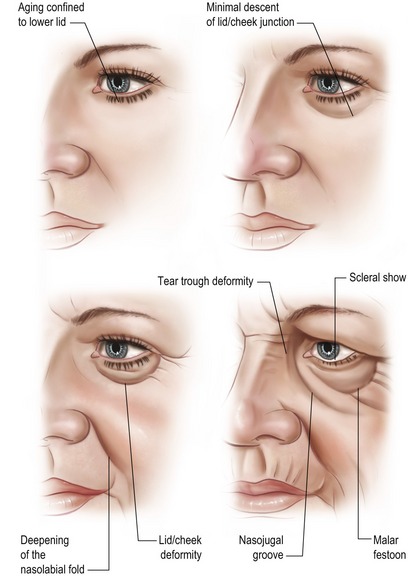
• Classification of morphological changes. Classification of changes according to the extent of midface aging provides a surgical guideline for the extent of dissection of the tear trough, and supra- or sub-periosteal dissection. A description of this classification is found in Fig. 19.3. In general, patients with lesser degrees of descent (type I or II) may necessitate only a lower lid blepharoplasty. Patients with more defined changes, such as lid–cheek deformity or nasolabial folds (type III) respond more effectively to a midface/cheeklift procedure. Patients with more advanced changes such as those with malar festoons and pronounced grooving (type IV) respond more completely to subperiosteal dissection and soft tissue redraping. In our surgical description below, we will concentrate on treatment of type III and IV deformities.
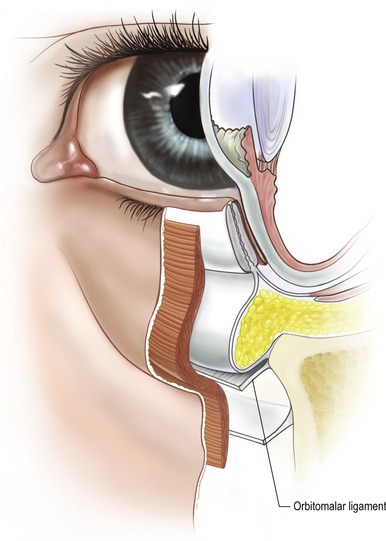
Anatomy
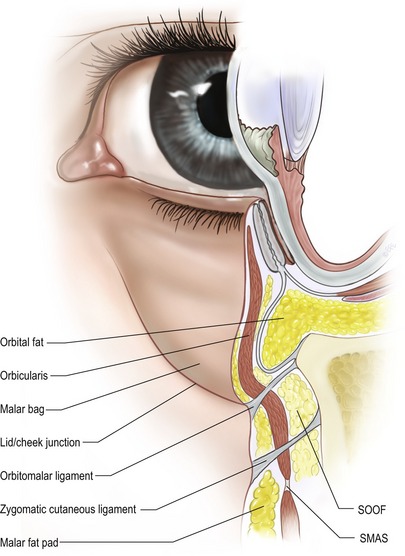
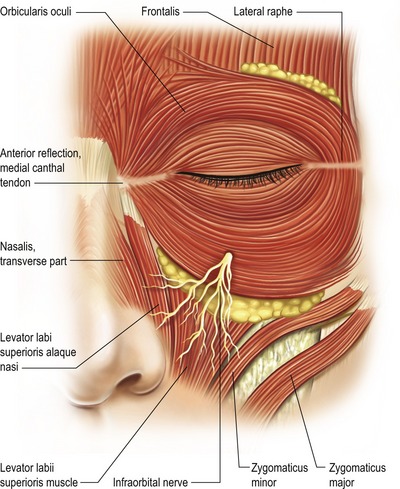
A major support structure of the midface is the orbitomalar ligament which is the primary retaining ligament of this region (Fig. 19.4). The orbitomalar ligament is an osseocutaneous ligament which originates at the inferior orbital rim just below the arcus marginalis and histologically has been shown to anteriorly penetrate the orbicularis oculi muscle inserting into the dermis (Fig. 19.5). Laxity of the orbitomalar ligament contributes to formation of the malar crescent and malar festoons, which are common findings with mid-facial aging. In addition, the orbitomalar ligament contributes to the formation of lid–cheek junction. The ligament, along with the origin of the levator labii superioris and levator alaeque nasi muscles contribute to formation of the tear trough and can be released subperiosteally to treat this deformity.
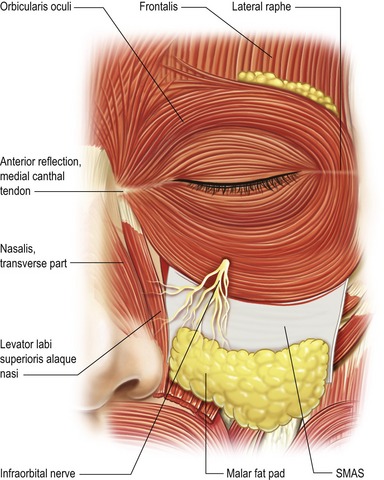
The origins of the deep facial mimetic muscles lie in the periosteal plane and provide an anchor for facial movement (Fig. 19.6). In addition to orbital fat compartments, two additional fatty layers exist in the midface. Analogous to the ROOF in the upper lid, the suborbicularis oculi fat (SOOF) lies deep to the orbicularis oculi in the lower lid and midface. This layer is readily visible following suborbicularis dissection below the infraorbital rim. As the inferior portion of the arcus marginalis is identified and released through its attachment anterior to the orbital rim at the orbitomalar ligament, the SOOF is defined between the overlying orbital portion of the orbicularis and the underlying soft tissue structures of the midface, often enveloping the zygomaticus major and minor muscles. With aging changes, descent of the SOOF contributes to overlying soft tissue attenuation thereby unmasking the nasojugal groove. Release of the origin of the alaeque nasi as well as repositioning of orbital fat anterior is a common maneuver to flattening out the nasojugal groove. Division of the orbital retaining ligament as well as the zygomaticocutaneous ligament provides mobilization of the SOOF, separating the prezygomatic space from the preseptal space. This maneuver is important in performing a lateral midface lift in an effort to treat malar descent.
The superficial musculoaponeurotic system (SMAS), which envelopes the orbicularis, also provides major support to the midface. Laxity of the SMAS is often a contributing cause of midface descent (Fig. 19.7). The malar fat pad is a triangular shaped fat pad in the midface which is located in the subcutaneous plane superficial to the SMAS. Aging changes caused by descent of the malar fat pad often unmasks the orbital fat pads from inferior migration and thinning of overlying tissue.