CHAPTER 48 Mastopexy with and without augmentation
Physical evaluation
• Measure breast width and upper pole pinch thickness.
• Assess for nipple ptosis by noting nipple position relative to inframammary fold.
• Assess for glandular ptosis by measuring centimeters of breast hanging below the inframammary fold.
• Assess for presence of unpigmented skin below the areola with the patient upright on frontal view.
• Assess overall breast skin quality, skin stretch, masses, and previous scars.
• Assess for any chest wall abnormalities such as pectus excavatum, pectus carinatum, thoracic hypoplasia, etc.
• Assess for any evidence of a tuberous breast deformity including constriction of the breast in the horizontal or vertical dimensions and herniation of the areola.
• Take note of asymmetries preoperatively including inframammary folds, breast volume, nipple position, ptosis, and chest wall.
Technical steps
Mastopexy without augmentation and mastopexy with augmentation are really two different procedures and we will address them separately, although some principles do overlap. Both procedures aim to raise the breast gland and the nipple in relation to the chest wall. Mastopexy with augmentation is more complicated since there are more variables related to implant selection and position. In addition, mastopexy with augmentation is more likely to disrupt the blood supply to the nipple due to more extensive undermining and it is more likely to require revision.
Preoperative assessment
Marking
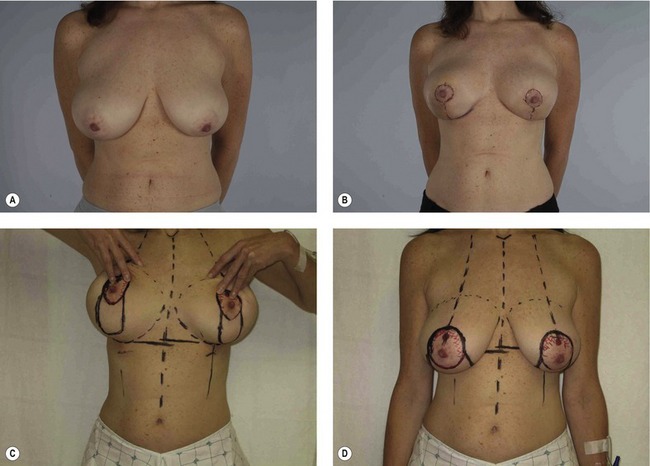
The patient is marked while standing, often on the day prior to surgery. Midline, bilateral breast meridians, and inframammary folds are marked (Fig. 48.1). Nipple height is usually set at or just above the level of the inframammary fold in mastopexy patients, but up to 4 cm higher than the fold in mastopexy with augmentation patients in order to center the nipple and breast over the implant. Based around the selected nipple position, a circumareolar pattern is drawn either free hand or using the circular portion of a Wise pattern ring. The superior aspect of the circumareolar marking should be 2 cm above the new nipple position. The lateral, medial, and inferior markings should skirt the areola creating an oval that includes the existing areola.