The nose and the nasal airway is highly complex with intricate 3-dimensional anatomy, with multiple functions in respiration and filtration of the respired air. Nasal airway obstruction (NAO) is a complex problem with no clearly defined “gold-standard” in measurement. There are 3 tools for the measurement of NAO: patient-derived measurements, physician-observed measurements, and objective measurements. We continue to work towards finding a link between subjective and objective nasal obstruction. The field of evaluation and surgical treatment for NAO has grown tremendously in the past 4-5 decades and will continue to grow as we learn more about the pathophysiology and treatment of nasal obstruction.
Key points
- •
The nose/nasal airway is a complex structure with intricate 3-dimensional anatomy; portions of the structure are composed of skin that has no supporting cartilage or bone.
- •
The nose functions as a heat and moisture exchanger. The nose also acts as a filter for particles.
- •
The measurement of nasal obstruction (NAO) can be broken into 3 tools for measurement: patient-derived measurements, physician-observed measurements, and objective measurements.
- •
The concept of a nasal valve has been key to our understanding of NAO.
- •
The field of evaluation and surgical treatment for NAO has grown tremendously in the past 4 to 5 decades and will likely continue to grow.
The nose is a complex structure
The nose and the nasal airway is a highly complex structure with intricate 3-dimensional anatomy resulting in one of the few areas of the body where portions of the structure are composed of skin that has no supporting cartilage or bone. Despite this incomplete substructure, it functions in respiration and filtration in a highly advanced way. This presents difficulty for both patients and clinicians in determining where within the nasal airway perceived obstruction lies.
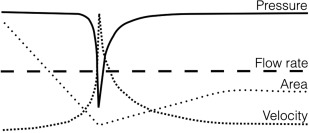
Nasal obstruction (NAO) is a common complaint in primary care and otolaryngologists’ offices. Evaluation of NAO goes back just as far as the published record. The study of obstruction is the study of flow and resistance. The complex intranasal anatomy contains areas of substantial variability in flow ( Fig. 1 ). The first published studies on these were using molds of the upper airway and smoke trails in the early 1950s. These studies demonstrated rapid air flow through the areas of the inferior and middle meatus. Further studies in the 1980s, 1990s, and today, using more advanced modeling techniques, demonstrated similar findings. However, we are no closer today to finding the single answer to the cause of NAO than we were decades ago.
The nose is a complex structure
The nose and the nasal airway is a highly complex structure with intricate 3-dimensional anatomy resulting in one of the few areas of the body where portions of the structure are composed of skin that has no supporting cartilage or bone. Despite this incomplete substructure, it functions in respiration and filtration in a highly advanced way. This presents difficulty for both patients and clinicians in determining where within the nasal airway perceived obstruction lies.
Nasal obstruction (NAO) is a common complaint in primary care and otolaryngologists’ offices. Evaluation of NAO goes back just as far as the published record. The study of obstruction is the study of flow and resistance. The complex intranasal anatomy contains areas of substantial variability in flow ( Fig. 1 ). The first published studies on these were using molds of the upper airway and smoke trails in the early 1950s. These studies demonstrated rapid air flow through the areas of the inferior and middle meatus. Further studies in the 1980s, 1990s, and today, using more advanced modeling techniques, demonstrated similar findings. However, we are no closer today to finding the single answer to the cause of NAO than we were decades ago.
Function and physiology
Humans are unique among hominids with increased nasal projection, anterior nasal convexity, expansion of the nasal bone breadth, exaggerated nasal angles, prominence of the anterior nasal spine, and substantial cartilage framework at the nasal tip. These traits began with the Homo erectus and continued in our lineage. All of these adaptations are felt to increase the ability of the nose to warm and moisturize the inspired air. These changes afforded the nose the ability to pull increased volumes through a more limited space and increase the contact with mucosa. This evolution is thought to be brought on by migration of early humans to more arid climates. This migration may be the underlying drive towards improving NAO as Homo erectus strived to have the air he breathed remain as moist, warm, and pure as it had been in tropical climates.
Studies supporting this hypothesis were hard to generate and were based much on earlier research of the nasal physiology. Heat and moisture exchange was determined experimentally through evaluation of patients with and without tracheotomies. The nasal physiology is complex, but data from these studies demonstrate air presented to the nostrils at 20°C attains 32°C at the back of the nasopharynx and changes from 45% relative humidity to 98%. The same temperature air only reaches 30°C and 80% humidity if inspired orally. Thus, the ability of the nasal mucosa to moisten air would be key in a more arid climate to prevent dehydration.
Heat and moisture exchanges represents only a small portion of the physiologic purpose for the nose and nasal cavity. The nose also acts as a filter for particles. The earliest studies began in the 1950s and continue currently to evaluate the filtration function of the nose. Through multiple study methods, particles larger than approximately 25 to 30 microns are deposited at near 100% within the nasal cavity. This filtration and subsequent chemoreception is sensed in both the olfactory cleft and portions of the anterior nasal cavity.
The loss of thermoreception and chemoreception may represent some of the feelings of NAO when a patient’s airway is made overly patent by turbinate surgery. Thermoreceptor TRPM8 function has been implicated in the sensation of NAO with loss of adequate thermal change in the mucosa of the nose resulting in feelings of NAO. The turbinates create nonlaminar flow resulting in the warming of the air by contact with mucosal surfaces. This presents cooling to TRPM8, which is postulated as one of the mechanisms of sensation of nasal patency.
Nasal obstruction poorly characterized
Some of the earliest attempts to measure NAO began with attempts to establish the diagnosis. Early surgeons struggled in patients with persistent symptoms of NAO, but an absence of definitive pathologic findings. The Cottle maneuver was developed by Heinberg and Kern in the 1970s and named for Dr M.H. Cottle to evaluate patients with NAO. The maneuver is performed by pulling the cheek laterally and is positive when this improves the patient’s sensation of nasal airflow.
The Cottle maneuver is a well-known and highly sensitive test with poor specificity. As such, multiple revisions of the technique have been performed to improve specificity with some encouraging results. The use of a small item (ear curette or cotton swab) to support the lateral nasal wall during inspiration was shown to correlate significantly with postoperative results from placement of spreader grafts to improve the nasal airflow.
In our practice, we perform what we call the passive Cottle maneuver. With this maneuver, the examiner’s fingers are placed on each side of the nasal sidewall on the skin of the medial maxillary buttress. The examiners fingers are used to simply ‘tense’ the skin of the lateral nasal wall rather than expand the nasal airway. The patient is then asked to breathe in. If the patient gets relief from this maneuver, it is likely they have dynamic lateral wall insufficiency and would benefit from strengthening the lateral nasal wall.
Measuring nasal obstruction
The measurement of NAO can be broken into 3 different tools for measurement: patient-derived measurements, physician-observed measurements, and objective measurements. The first is highly important, but a well-known, inexact form of measurement. The second is key in establishing a diagnosis and, although intrarater recognition of findings is fairly consistent, interrater assessment can be variable and is not necessarily correlated with patient symptoms. The third can be very standardized, but also does not necessarily correlate with patient symptoms or patient findings on examination.
Patient-derived measurements
Multiple patient reported outcome measures have been used previously for evaluating the symptoms of NAO. Before the current century, no single test was validated, widely accepted, and used. Visual analog scales (VAS) were some of the first to be used. These scales represent patients’ overall perception of a problem or group of problems placed on a linear scale from absent to severe. Although this is a useful gauge to determine problem severity, based on its intrarater and interrater variability, its usefulness as a standalone measure is minimal.
In an era where health-related quality-of-life measures are at the forefront of medicine, the most prominent and frequently used in the evaluation of NAO is the Nasal Obstruction Symptom Evaluation (NOSE) score. This quality-of-life scale was created in 2004 out of a need for a reproducible, valid scale to measure a difficult clinical problem. It consists of 5 questions on a scale of 0 to 4 that is multiplied by 5 resulting in a score from 0 to 100 with 100 as the most severe NAO ( Fig. 2 ).
Since its inception, the NOSE scale has been validated multiple times for both preoperative and postoperative evaluation of patient symptoms. The system has become the gold standard for patient-derived measurements with 64 articles indexed in the English literature featuring this scale at the time of this writing. Unfortunately, the scale correlated poorly with objective measures. In 1 well-performed study of 290 patients with NAO, without sinus disease, were evaluated by acoustic rhinometry (AR), peak nasal flow (PNF), and NOSE score with VAS and no correlations were found of the 16 evaluated. Despite this poor correlation with objective measurement, the NOSE score has an exceedingly useful preoperative and postoperative quality-of-life/patient-reported outcome measure evaluation tool.
Using this system, a severity classification has been created for NAO with cutoff points at 5, 30, 50 and 75 representing patients with mild (5–25), moderate (30–50), severe (55–75), and extreme (>80) obstruction. This classification system was found to have a greater than 90% sensitivity and specificity for evaluating patients with NAO.
Sinus evaluation has several validated measures, including the Sino-Nasal Outcomes Test. This test was originally designed as a 20-item questionnaire with a score between 0 and 100. In 2009, 2 questions were added to address smell and NAO to create the Sino-Nasal Outcomes Test-22. The scores were validated using other methods such as the NOSE scores and are very useful in patients with chronic sinusitis and concomitant NAO.
Physician-derived measurements
Physician-derived measurements for evaluation of NAO began in earnest with Guy de Cehauliac when he referred in his writing to the nasal speculum in the 13th century. The field has changed by leaps and bounds owing to the diligent work of innumerable clinician–scientists; however, we continue to struggle with the physician-derived measurement techniques for NAO.
The concept of a nasal valve has been key to our understanding of NAO. Starting with Bridger in 1970, the nasal valve as a primary site of obstruction was codified. In his work, Bridger illuminated the physics of fluid passing through the nose and the creation of a “flow-limiting segment,” which he called the nasal valve at the junction of the caudal edge of the upper lateral cartilage and the nasal septum. Goode continued this work in 1985, describing diagnosis and surgery within this location. Goode went into great detail about the various causes, including septal deviations, iatrogenic causes from cartilage resection or inappropriate osteotomies, weak or recurved cartilage, facial nerve weakness, or vestibular soft tissue insufficiencies.
This structure remains so vitally important in the nasal airway that papers continue to be published on the surgical evaluation and treatment of the nasal valve. In 2010 a clinical consensus statement was released by the American Academy of Otolaryngology—Head and Neck Surgery. This group defined nasal valve compromise as a distinct entity resulting in NAO with a variety of causes. The statement included that history and examination, including anterior rhinoscopy, Cottle maneuver or modified Cottle maneuver, and visualization of the nasal wall during inspiration were sufficient to diagnose nasal valve compromise.
Both Bridger and Goode cited a second area prone to dynamic collapse, which was initially termed alar collapse and later termed external nasal valve collapse. The area is caudal to the internal nasal valve and is composed of the septum, nasal ala, and caudal portion of the lower lateral cartilage. This is a zone defined by the American Academy of Otolaryngology—Head and Neck Surgery group subject to valve compromise. More recently, this terminology has been modified to be the less ambiguous “lateral wall insufficiency or collapse.” The lateral nasal wall and its dynamic collapse or lateral wall insufficiency can be broken into 2 zones, with zone 1 superior to the scroll region of the upper and lower lateral cartilages and zone 2 inferior to that. Zone 2 collapse represents classical alar collapse or external valve collapse. This method of classification allows for previously poorly characterized collapse superior to the region of the external nasal valve, or zone 1, to be evaluated and more adequately treated. Most important, a validated, physician-derived grading scale has been developed to quantify the amount of dynamic collapse of the airway in these cases ( Table 1 ).







