Introduction
The mandible provides support for the teeth and attachment of the maxillofacial muscles and with the temporal bone, forms the temporomandibular joint (TMJ). Tributaries of the inferior alveolar neurovascular bundle, passing through the mandibular canals, are distributed to the skin of the chin and mandibular teeth. An impingement of the mandibular canal can result in sensory disorders of the mandibular teeth and skin of the chin.
The masticatory muscles consist of the masseter, temporalis, and medial and lateral pterygoids, and these are innervated by the mandibular nerve. The masticatory muscles and their associated neurovascular and fascial systems are important in various surgical approaches.
Mandible
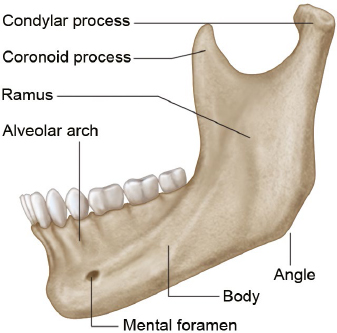
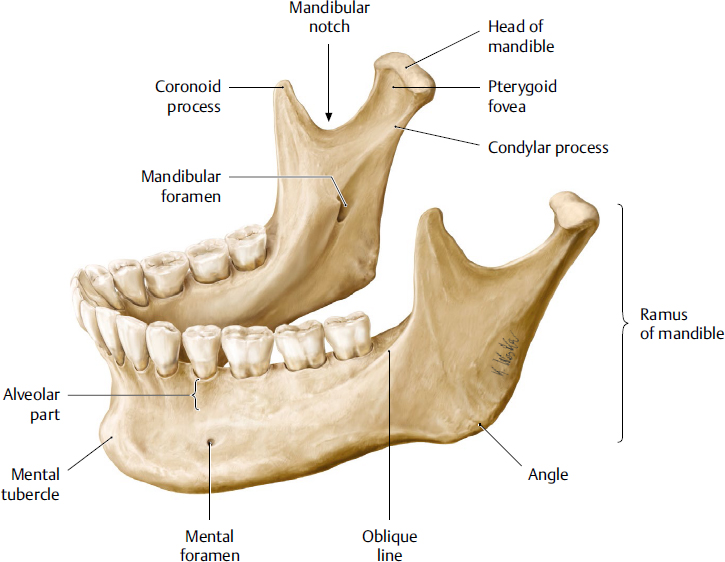
The mandible is the only bone of the lower jaw. It consists of an arch-shaped body and two quadrilateral rami (Fig. 19.1). The mandible provides support for the mandibular teeth; provides for attachment of muscles, including facial, masticatory, and infrahyoid muscles; and is the lower component for the TMJ. The bone also provides passage for the inferior alveolar nerve and vessels supplying the mandibular teeth and lower face.
Body
The body of the mandible is U-shaped and convex anteriorly. It has external and internal surfaces and an alveolar part (tooth-bearing portion). The inferior border of the body continues with the ramus, and together they form the mandibular base.
External Surface of the Body of the Mandible
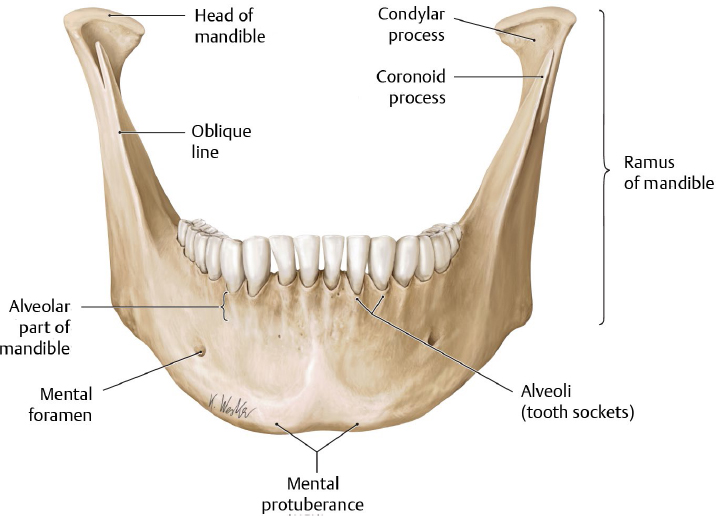
During development, half-sides of the mandible are fused by a mandibular symphysis in the midline (Fig. 19.2). A vague median ridge at the upper external surface in an adult mandible can indicate the fused site. The ridge bifurcates at the lower external surface, and the mental protuberance lies between them and is triangular-shaped. Two mental tubercles and the small central depression between them lie on the base of the mental protuberance.
The mental protuberance and tubercles constitute the chin (i.e., the mentum). The mental foramen is usually located below the interval between the premolar teeth or second premolar, approximately on the midpoint between upper and lower border of the mandible. The mental neurovascular bundle emerges from the mental foramen after passing through a canal inside the mandible (mandibular canal). The bundle emerges backward, and thus the posterior rim of the foramen is smooth, whereas the anterior rim is more distinct. The exact position of the mental foramen and the course of the neurovascular bundle within it are important during dental implant procedures.
The external oblique line is faint and ascends posteriorly from the mental tubercle to the anterior border of the ramus of the mandible. The line is distinct farther backward and continuous with the sharp anterior border of the ramus.
Surgical Annotation. Harvesting Bone from the Chin
Alveolar bone resorption resulting from tooth loss reduces supporting bone for the dental implant placement. To enhance vertical bone dimensions, the mandibular symphysis area is recommended as the donor site for the autogenous bone graft. An osteotomy should be made away from the apex of the root of the incisors. It is suggested that the surgical site of the osteotomy be located 5 mm from the dental roots.1
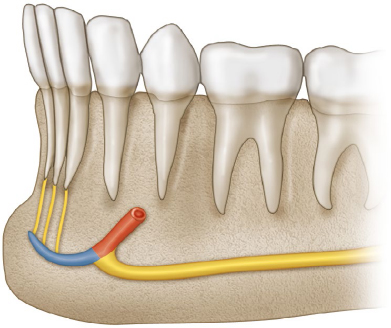
Additionally, encroachment of the mental foramen by the osteotomy results in insensitivity on the chin. According to dentition, the mental foramen lies below the premolar area, especially in the interval between these teeth. Superficially, the mental foramen lies about 2 cm below the corner of the mouth and slightly lateral to it. The distance between the bilateral mental nerves is about 45 mm.2 Regarding the anterior loop (mandibular canal anterior to mental foramen (Fig. 19.3), the safe area might be narrower than the interval between the mental foramina.
The cortical plate on the chin is thick further downward. Anatomical research in Asians has demonstrated that the maximum volume of graft block can be harvested from the rectangular site from the mandibular symphysis with a height of 1 to 1.5 cm and a width of 4.0 cm centered at the midline.1
Internal Surface of the Body of the Mandible
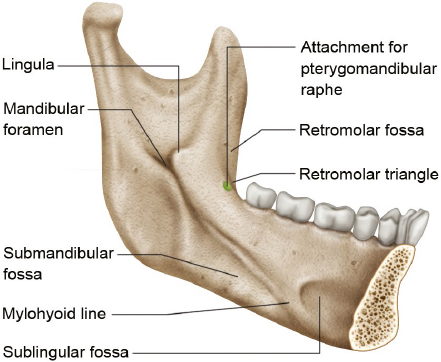
An oblique mylohyoid line extends from the area below the mandibular third molar as far forward as the midline and gives attachment to the mylohyoid (Fig. 19.4). The concave area below the line is a submandibular fossa providing space for the submandibular gland. The line is faint further forward and ends by widening into a concave sublingual fossa for the sublingual gland. The mylohyoid groove from the ramus lies below the mylohyoid line at the posterior end of the mylohyoid line. The digastric fossa lies near the midline on each side on the internal surface of the mandible and gives attachment to the anterior belly of digastric.
Mental spines lie near the internal aspect of the mandibular symphysis on both sides. Although it sometimes merges into a single tubercle or is absent, the spine usually divides into two parts: an upper part for attachment to genioglossus and a lower part for attachment to geniohyoid.
Alveolar Part
The upper border between the internal and external surfaces of the mandible forms the alveolar part, giving support for the mandibular teeth. It contains the alveoli (alveolar sockets) for seven to eight mandibular teeth on one side. The alveolar part consists of the buccal and lingual plates, which are located on the external and internal aspects of the bone, and interdental and interradicular septa, which separate each tooth and root, respectively.
Fig. 19.2 External surface of mandible. (From THIEME Atlas of Anatomy, Head and Neuroanatomy. © Thieme 2010, Illustration by Karl Wesker.)
Fig. 19.3 Anterior loop of the mandibular canal. The yellow portion of thick canal represents the mandibular canal, and the red represents the anterior loop of the mandibular canal proceeding toward the mental foramen. The blue portion presents the incisive canal. The yellow small lines in the anterior region indicate the incisive nerves innervating the incisive teeth.
Ramus
The ramus of the mandible is a broad square-shaped part extending backward and upward from behind the body (Fig. 19.5). It consists of lateral and medial surfaces, four borders (superior, inferior, anterior, and posterior), condylar, and coronoid processes. The ramus provides entrance and passage for the inferior alveolar bundle (mandibular foramen and canal), attachment for masticatory muscles, and the condylar process for articulation at the TMJ.
Surfaces and Borders
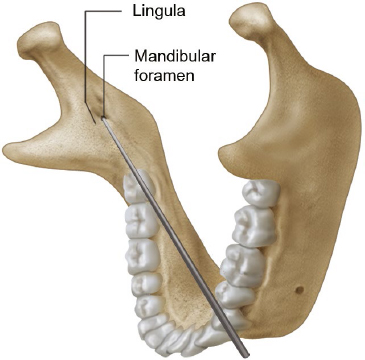
The lateral surface is smooth except where the masseter attaches to its lower part. The medial surface of the ramus is more complicated. The mandibular foramen, the opening of the mandibular canal, is located at the point just above a center of the ramus. The anterior portion of the foramen is partially covered by a sharp triangular spine, the lingula. The tip of the needle should be placed at the vicinity of the lingula during an inferior alveolar nerve block (Fig. 19.6). The ligula lies about 1 cm above the occlusal plane.
The mylohyoid groove extends forward and downward from the lowermost part of the mandibular foramen. The anterior end of the groove lies below the mylohyoid line. Nerve and vessels proceed on the groove and distribute to the mylohyoid, which is the main muscle forming the floor of the mouth. The medial pterygoid muscle attaches to a rough surface behind and below the mylohyoid groove.
The external oblique ridge continues along the anterior border of the ramus on its lateral surface. From the tip of the anterior border (coronoid process), a ridge descends on the medial side of the process to the area posterior to the third molar region. This ridge, the temporal crest, constitutes a small triangular depression (retromolar fossa) with the external oblique line.
The joining of the mandibular base and the posterior border of the ramus forms the angle of mandible. A portion of the mandibular base anterior to the angle is slightly curved superiorly and is called the premasseteric notch. The facial artery passes beneath the premasseteric notch; thus, the pulsation of the artery can be palpated here.
The superior border bears a sharp, triangular coronoid process and a round and claviform condylar process. The mandibular notch is an incisure with a sharp superior edge between two distinct processes. Nerve and vessels to the masseter on the lateral surface of the ramus pass though the mandibular notch.
Surgical Annotation: Identifying the Mandibular Foramen
With a thumb on the anterior border of the ramus fits on the concave line of the border, the line through the distal end of the thumbnail and the interproximal point of the two premolars on the opposite side passes through the vicinity of the mandibular foramen. This line is usually used for an inferior alveolar nerve block.
Coronoid Process
The coronoid process is thin, triangular shaped, and protects upward. Its anterior border is a continuum of the external oblique ridge, and the mandibular notch limits its posterior border. The temporalis is attached to the anterior, posterior, and medial borders of the coronoid process.
Fig. 19.5 Internal surface of ramus of mandible. (From THIEME Atlas of Anatomy, Head and Neuroanatomy. © Thieme 2010, Illustration by Karl Wesker.)
Fig. 19.7 Arrangement of inferior alveolar neurovascular bundle. Yellow represents the inferior alveolar nerve, mental nerve, and incisive nerve. Red and blue represent the inferior alveolar artery and vein, respectively.
Condylar Process
The condylar process consists of the articular head and the neck. The articular head participates in articulation with the mandibular fossa of the temporal bone. The pterygoid fovea is a small fossa on the anterior surface of the neck and gives attachment to the upper head of the lateral pterygoid. Since the head of the condylar process is larger than its neck and the condylar process acts as an axis of jaw joint, the condylar process is frequently fractured with trauma.
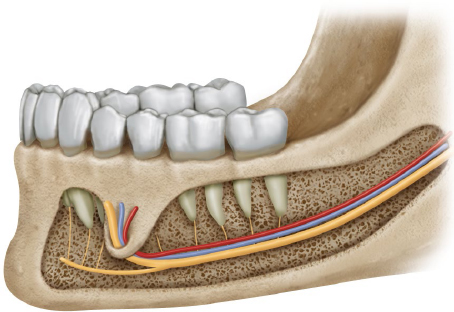
Mandibular Canal
The mandibular canal is the bony canal extending from the mandibular foramen to the mental foramen. The canal runs downward and forward within the ramus then runs horizontally within the body under the tooth-bearing portion. The canal is closer to the external surface (labial cortical plate) farther forward. In the anterior end of the canal, it extends anterior to the mental foramen and curves back to the foramen, forming the anterior loop.
The inferior alveolar nerve and vessels enter the mandibular canal through the mandibular foramen. The trunk of the inferior alveolar nerve divides into mental and incisive nerves. The former exits through the mental foramen and innervates the skin of the chin. The latter passes medially within the mandible and innervates the incisors. The bony passage of the incisive nerve is called the incisive canal.
The neurovascular bundle from the inferior alveolar nerve and vessels to the teeth is within numerous tiny canaliculi between the canal and the alveolar part. Radiographically, the mandibular canal’s upper border is less distinct compared with its lower border.
Damage to the Mandibular Canal
The inferior alveolar nerve innervates all mandibular teeth, and the mental nerve supplies sensation of the skin and mucosa of the chin. Intrusion of an instrument or dental implant can result in a sensory disorder of the teeth distal to the injury site.1 Therefore, an injury of the inferior alveolar nerve within the mandibular canal causes partial or complete numbness of the chin area.
Additionally, the mental nerve is a branch from the inferior alveolar nerve, and its sensory component is conveyed through the buccal portion of the inferior alveolar nerve. The foramen is located below the premolars in about half the cases.2 The position of the mental foramen varies among races and individuals. Therefore, its position on radiography should be performed before surgical intervention on the premolar area.
The inferior alveolar nerve lies below the inferior alveolar vessels, and the artery is located lingual to the vein in most cases (Fig. 19.7).1 Therefore, transient numbness can result indirectly from the compression of, for example, a hematoma.
Some surgeons try to overcome limitation of a fixture placement because of the mandibular canal by altering angulation or position of the fixture; however, some difficult situations (more than 10%) occur in which the mandibular canal follows midway or a lingual one-third passage within the mandible.1 The buccolingual position should be evaluated radiographically before intervention.
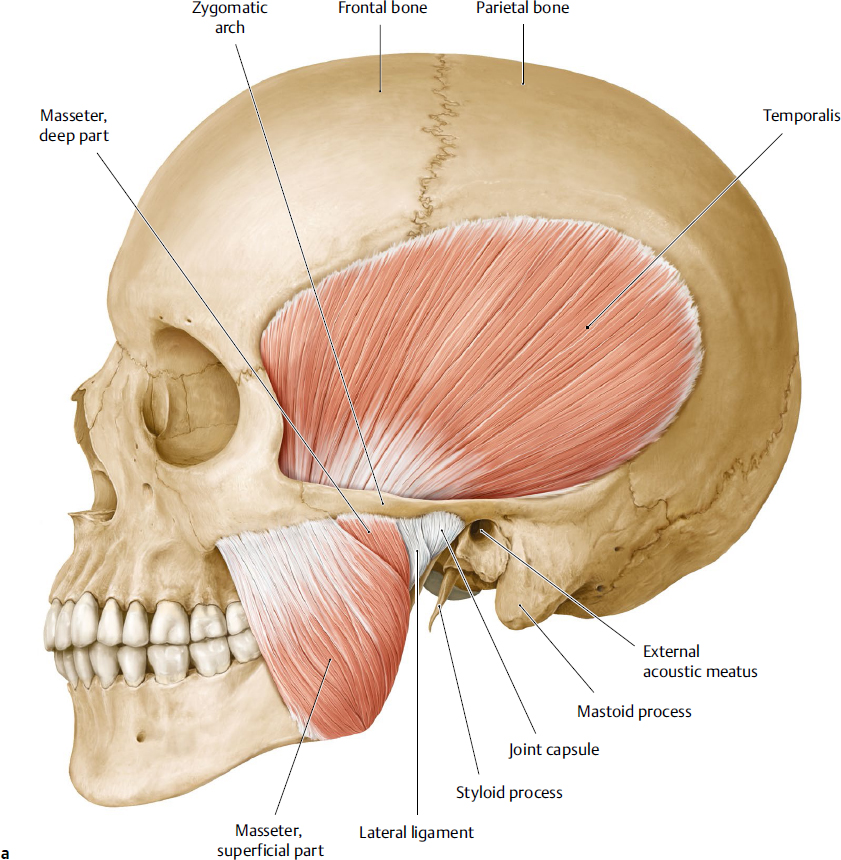
Masticatory Muscles
The main masticatory muscles consist of the masseter, temporalis, and medial and lateral pterygoids. The masseter lies on the external surface of the ramus of the mandible and the temporalis is located in the temporal fossa. The two pterygoid muscles and the tendon of temporalis are located in the infratemporal fossa (Fig. 19.8a–c).
The four muscles are derived from the first pharyngeal arch and are innervated by the mandibular division of the trigeminal nerve. The maxillary artery from the external carotid artery and supplementary branches from the facial or superficial temporal arteries supply blood to the masticatory muscles. The masticatory muscles produce movements of the mandible at the TMJ; elevate the mandible (masseter, temporalis, medial pterygoid); pull down (lateral pterygoid), protrude (lateral pterygoid) and retract it (temporalis). They also act together to provide complicated side-to-side movements. Functionally, the infrahyoid muscles, including the digastric, stylohyoid, geniohyoid, and myohyoid muscles, participate in accessory mastication functions such as opening the mandible. The four masticatory muscles innervated by the mandibular nerve are commonly regarded as principal movers of the jaw.
Masseter
The masseter has been commonly described as a muscle arising from the maxillary process of the zygomatic bone and the zygomatic arch and inserting into the angle and the lower part of the lateral surface of the ramus of the mandible. The main action of the masseter is to occlude the teeth by elevating the mandible.
Actually, the masseter consists of three layers; superficial, middle, and deep layers. Although the fibers of the three layers mostly pass downward and backward, detailed directions of the muscle fibers are slightly different according to the layer. The superficial layer arises from the maxillary process of the zygomatic bone and the anterior two-thirds of the zygomatic arch and inserts into the angle and its neighboring portion of the external surface of the ramus. The origin of the middle layer lies posterior to the superficial layer. The middle layer arises from the medial aspect of the anterior two-thirds of the zygomatic arch and the lower border of the posterior one-third of the arch and inserts into the central part of the ramus. The direction of the superficial layer is anterior to the middle one, and thus the superficial layer participates more in protraction of the mandible. The deep layer arises from the deep surface of the zygomatic arch and inserts into the upper part of the ramus and the coronoid process. Some parts of the middle and deep layers are involved in retraction of the mandible. The temporalis and buccinator muscles lie deep to the masseter. Most of the buccal branches, some zygomatic branches of the facial nerve, and facial vein cross over the masseter. The parotid gland overlaps the posterior part of masseter.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree