Liver Transplantation Using a Cavocavostomy
Christopher J. Sonnenday
DEFINITION
Liver transplantation is the only definitive therapy for end-stage liver disease. Deceased donor liver transplantation is typically done in an orthotopic manner, traditionally with replacement of the retrohepatic inferior vena cava (IVC) en bloc with the donor liver (“bicaval liver transplantation”). Over the past two decades, more transplant centers have migrated to a technique preserving the recipient native IVC, which potentially mitigates the need for venovenous bypass and may be associated with fewer physiologic derangements from temporary caval disruption. One technique for implantation of the donor allograft with caval preservation is the cavocavostomy in which a side-to-side anastomosis is created between the donor and recipient IVC.
PATIENT HISTORY AND PHYSICAL FINDINGS
Common indications for liver transplantation and details of the evaluation process are detailed in other chapters.
Although transplant programs and centers typically adopt a preferred method of outflow reconstruction in liver transplantation, certain patient characteristics and diagnoses may lead to consideration of alternative techniques.
Caval preservation, and therefore cavocavostomy, may not be possible in all patients. In patients with caudate lobe tumors, for example, caval preservation could risk violation of the tumor during hepatectomy and should be used selectively.
Other patients in whom caval preservation could be more difficult include patients with a large hypertrophied caudate lobe and/or a caudate lobe that is completely circumferential to the retrohepatic IVC. Patients with cholestatic liver disease, such as primary sclerosing cholangitis, often have particularly large caudate lobes.
Although unusual, patients with caval stenosis or thrombosis or who have indwelling retrohepatic IVC metallic stents are not good candidates for cavocavostomy.
Morbidly obese transplant recipients may be thought to be difficult candidates for caval preservation due to difficulties of exposure and a deep anteroposterior (AP) diameter. However, these are also recipients in whom the bicaval anastomoses may be quite difficult for similar reasons. Therefore, caval preservation should be strongly considered in obese or deep recipients.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The transplant evaluation includes a comprehensive evaluation of general health and organ function, including a standard battery of laboratory studies, cardiopulmonary testing, and assessment of viral serologies.
Required pretransplant imaging varies by center practice and recipient diagnosis. At a minimum, liver ultrasound with Doppler to demonstrate patency of the hepatic inflow (hepatic artery and portal vein) and outflow (hepatic veins and IVC) is performed.
Most patients will also undergo cross-sectional imaging (liver computed tomography [CT] or magnetic resonance imaging [MRI]) at some point in their evaluation or in the management of an associated hepatocellular cancer.
When considering the technique of outflow reconstruction during liver transplantation, attention should be paid to the available preoperative imaging. Patency and caliber of the IVC and the orientation and size of the caudate lobe relative to the retrohepatic IVC should be assessed to anticipate ease of hepatectomy and the feasibility of caval preservation.
SURGICAL MANAGEMENT
Preoperative Planning
Decision making regarding the hepatectomy and method of outflow preservation should be made prior to transplant based on recipient characteristics, preoperative imaging, and surgeon preference. This plan may change during the operation based on the intraoperative events.
A standard liver transplant set should include a variety of large vascular clamps that provide options for control of the IVC regardless of the preferred technique of outflow reconstruction. Cavocavostomy is typically performed with partial clamping of the recipient IVC in a side-biting manner, typically with a large Satinsky clamp.
In some circumstances, bicaval clamping may be necessary to facilitate safe hepatectomy, allow repair of caval injuries sustained at hepatectomy, and/or to facilitate the cavocavostomy anastomosis in select circumstances. Control of the infrahepatic IVC may be done with a variety of large angled vascular clamps such as a Glover or Wylie hypogastric clamp. The suprahepatic IVC is typically controlled with a sturdy clamp with appropriate profile to fit under the diaphragm. The Calne or Klintmalm clamp is commonly used.
Caval preservation is facilitated by low central venous pressure, which allows dissection and division of retrohepatic veins without excessive blood loss. Seamless communication with the liver anesthesia team prior to the operation and throughout the procedure is essential to optimal patient outcomes.
Long, fine-tipped needle drivers are necessary to perform the cavocavostomy, as the anastomosis may be deep and at a steep angle from the operating surgeon.
Positioning
Liver transplantation is performed with the patient in the supine position, with arms out nearly perpendicular to the torso.
Central venous and arterial access are established. Pulmonary artery catheterization may be performed routinely or selectively according to center practice, although more routine use of intraoperative transesophageal echocardiography may eliminate the necessity of pulmonary artery catheters for monitoring cardiac performance. A Foley catheter is placed. Core temperature monitoring is a necessity with either a temperature-sensing bladder catheter or esophageal probe.
TECHNIQUES
BACKBENCH PREPARATION OF THE DONOR LIVER
A standard back-table preparation of the donor liver is performed when considering cavocavostomy.
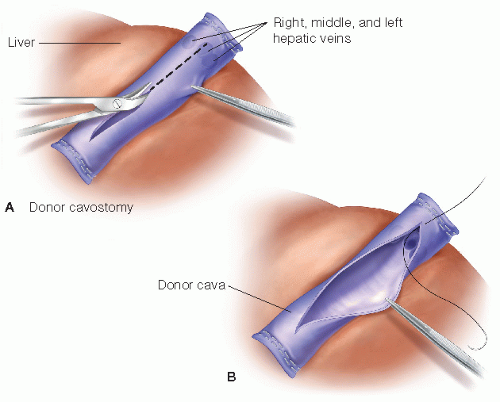
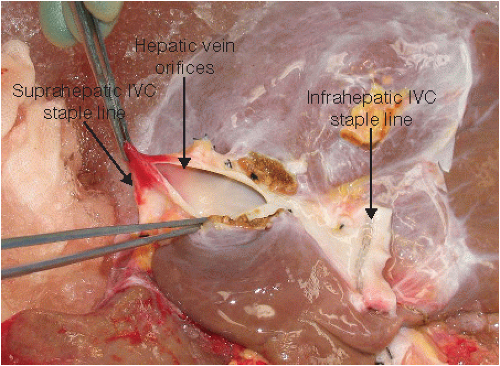
Pay attention to the length of the infrahepatic and suprahepatic IVC to assure easy closure prior to cavocavostomy (FIG 1). If additional length of the infrahepatic IVC is necessary to allow closure, small retrohepatic accessory veins may be doubly ligated and divided.
In cases where the donor liver has a circumferential caudate lobe, divide the caudate lobe along the posterior midline to facilitate the donor cavotomy.
Adequate length of the suprahepatic cava is essential to allow safe closure without compromise of the hepatic venous drainage. Given the desire for extra length of the suprahepatic cava, the temptation may exist to leave some right atrial tissue attached to the IVC. This atrial tissue is friable and does not hold staples or sutures well. Furthermore, if atrial tissue is present, there is likely more than adequate length of the suprahepatic cava to trim back to healthy cava and allow safe closure.
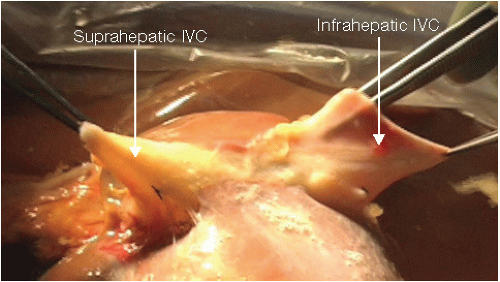
FIG 1 • Length of the donor infrahepatic and suprahepatic IVC to assure easy closure on the back table prior to cavocavostomy.
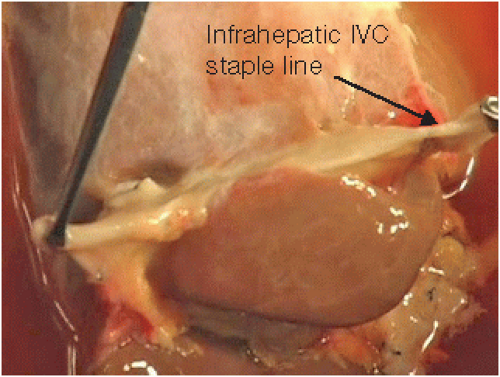
FIG 2 • Closure of the infrahepatic IVC in preparation for the cavocavostomy. Either oversew or staple the suprahepatic IVC.
In the rare circumstance that during procurement the suprahepatic cava is divided at or just above the level of the donor hepatic veins, create a caval extension using a piece of infrahepatic or infrarenal donor cava or donor iliac vein. An alternative technique in this situation is to perform a true cavoplasty reconstruction, as detailed below.
Once the native liver is removed and the decision to proceed with cavocavostomy is confirmed, final preparations are made to the donor liver for implantation.
Close the infrahepatic and suprahepatic IVC with an Endo GIA stapler (FIG 2). Suture closure of the suprahepatic cava may be more appropriate if there is concern about compromising the hepatic vein orifices with a short suprahepatic cava.
Once the ends of the donor cava are closed, make a cavotomy (6 to 8 cm) on the dorsal aspect of the donor cava in the midline (FIG 3A). Create the cavotomy so that it crosses the hepatic vein orifices, opening the venous drainage broadly (FIG 3B). Position the cavotomy toward the suprahepatic IVC, with its superior extent just inferior to the suprahepatic closure (FIG 4).
INCISION AND EXPOSURE
The liver transplant incision may vary by patient body habitus and surgeon preference, but a right subcostal incision with midline extension provides excellent exposure for almost all liver transplant operations. This incision allows midline extension up to the xiphoid process, which can be essential for exposure of the suprahepatic IVC, particularly in patients with a narrow costal angle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree