Introduction
Liposuction and liposculpture represent the evolution of minimally invasive plastic surgery techniques developed in an attempt at restoring shape and form. Liposuction was first described in the 1920s but it was not until the 1970s that the technique was popularized in Europe by Illouz, Fournier, and Otteni whereby fat was harvested using a blunt cannula and aspirated using negative pressure. Prior to liposuction, fat was directly excised leaving unsightly scars and increased morbidity. The effect of liposuction on the body has been extensively studied and it has been shown to be safe and effective. Other than producing improved contour cosmesis, liposuction was shown to reduce body weight, BMI, waist circumference, body fat, plasma leptin, and insulin levels. Although fat grafting was first described back in 1893 by Neuber, it was Coleman who popularized free fat transfer in a minimally traumatic fashion leading to a consistently higher graft retention compared to prior techniques. As research in the field increased, the indications and quoted graft retention rates also increased (20%–90%). Part of the reason for the wide variation in the results is the sheer amount of factors involved in graft survival. Though the Coleman technique is often accepted as the standard, in the nascent field of fat grafting, multiple strategies for liposuction, fat processing, and grafting have evolved, which makes standardization and optimization challenging. This chapter critically appraises each step in the process of liposuction and fat grafting, from harvesting to processing to injecting, to provide a detailed overview for the plastic surgeon of the 21st century.
Harvest Site
Liposuction for body sculpting or for fat harvesting purposes can be performed anywhere around the body as long as there is sufficient adiposity. The most common sites include the abdomen, flanks, and thighs. However, both animal and human studies have shown that donor site does not influence the quality of the lipoaspirate and the graft survival. In fact, in a murine model Ullmann et al found no significant differences based on thigh, abdomen, and breast donor sites in graft retention or histology after 16 weeks. Li et al repeated and expanded upon these animal findings, finding no difference in retention from five separate donor sites (flank, upper and lower abdomen, and lateral and inner thigh) after 12 weeks. Human studies have also found no difference based on comparative symmetry scores of craniofacial patients grafted with fat from the abdomen versus other areas (medial thigh, suprapubic). Similarly, in breast reconstruction Small et al found no significant difference in graft retention after 140 days in fat harvested from the abdomen versus the thighs. There is currently no evidence to support that harvest site independently influences graft survival. However, this parity has not been proven with higher-level prospective cohorts or randomized control trials, and further research is needed.
Donor Site Preparation
Liposuction can be performed dry (no wetting solution), wet (200 mL/area), superwet (1 mL infiltrate per 1 mL of aspirate), or tumescent (2–3 mL infiltrate per 1 mL of aspirate). The wetting solution may contain lidocaine, epinephrine, and/or sodium bicarbonate depending on surgeon’s preference. The benefit of using a superwet or tumescent solution is the significant decrease in blood loss down to 1%. Other benefits of using a wetting solution is the analgesic effect provided by lidocaine, volume replacement, and enhanced cavitation and heat dissipation in ultrasound-assisted liposuction. The concern of the use of wetting solutions in the setting of fat grafting is the potential effect on adipocyte viability and blood flow reduction to grafts. However, as early as 2005 Shoshani et al demonstrated no significant difference in weight and volume retention at 15 weeks between xenografts harvested with lidocaine and epinephrine versus a control of saline. Livaoğlu et al further proved the safety of local anesthesia showing no significant difference in retention at 180 days between control, lidocaine plus epinephrine, or prilocaine groups in an autologous murine model. Lastly, Rohrich et al found no significant differences in adipocyte viability among four donor sites (abdomen, flank, thigh, knee) determined on an in vitro colorimetric assay of cell proliferation. Overall, despite theoretical concerns for the use of local anesthesia, graft survival does not seem to be greatly affected by its use in animal models. This finding should be further investigated in human studies.
Harvest Technique
Depth of Liposuction
Fat can be aspirated at different depths of the subcutaneous layer but one has to be aware of potential risks and variation in quality of the fat (relevant if used for fat grafting). The superficial subcutaneous layer contains dense fat, which is adherent to overlying skin. The intermediate subcutaneous layer is the safest and most commonly aspirated layer. The deep subcutaneous layer contains looser and less compact fat, and can be safely aspirated in most areas except the buttocks. Ideally, the surgeon should avoid violating the superficial plane above the superficial fascia to ensure preservation of subdermal structures, and prevent surface irregularities. A variety of zones of adherence have been described, which should not be violated during liposuction because of the risk of contour deformity. These zones include the gluteal crease, middle medial thigh, lateral gluteal depression, distal posterior thigh, and distal iliotibial tract.
Cannula Size
The use of single-bore blunt-tip harvesting cannula has been standard practice since the description of the technique by Coleman. There are very few studies examining the impact of different parameter in cannula such as bore size and single versus multiple perforation.
To determine the impact of bore size, Erdim et al compared fatty aspirate obtained from 2-mm, 4-mm, and 6-mm blunt cannulas and found significantly higher in vitro adipocyte survival in the 6-mm group compared to both the 2-mm and 4-mm groups. However, this viability assessment was only based on brilliant cresyl blue supravital stained adipocyte counts after collagenase digestion and centrifuging. A similar in vitro study by Alharbi et al comparing 3-mm single-bore and 2-mm multiperforated St’rim cannulas (Thiebaud Biomedical Devices), found no significant difference in cell viability between the groups when measured by alamarBlue (ThermoFischer) reagent. Lastly, Kirkham et al compared 3-mm and 5-mm Coleman cannulas in a murine model using a dry technique, and found significantly higher graft retention and histologically healthier grafts in the larger cannula group at 6 weeks. These findings suggest that, generally, larger bore cannulas produce more viable cells leading to better graft retention. However, we must balance these results with data on parcel size discussed below. Given the limited data on graft survival, further longer-term, in vivo research with more modern viability assays is justified.
Parcel Size
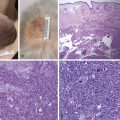
The importance of parcel size in fat graft survival is based on the same general theories of imbibition and neovascularization that are vital to survival of all tissue grafts. Early research theorized on how graft shape could affect percentage of graft that was more than 1.5 mm from the edge and how this would impact survival. This theory was expanded upon by Eto et al, who identified three distinct zones of adipocyte survival. Outer surviving zone with cells located within 300 μm of the graft edge; middle regenerating zone with cells undergo necrosis but are replaced by adipose-derived stem cells (ASCs); and central necrotic zone where no viable fat survives. The same group published further evidence of the behavior of grafts based on distance from the edge, showing adipogenesis via CD34 + /Ki67 + ASCs in the regenerating zone (600–1200 μm thick) peaked at 4 weeks and concluded by 12 weeks, while stabilization via MAC2 + /CD206 − M1 macrophages MAC2 + /CD206 + M2 macrophages in the central necrotic zone persisted through 12 weeks. The importance of the relation between graft and surrounding tissue has been further demonstrated in injected fat. Our group demonstrated that as the total fat volume transferred increases, grafted deposits coalesce to form larger globules (especially at ratios beyond 1:4). Therefore, increasing the likelihood of central necrosis and subsequent graft loss. Our group also showed that larger grafts contain central cores that could not be cleared appropriately by macrophages, allowing for persistent necrosis that skew retention as a measure of survival. The architecture of fat grafts is clearly important, with the principles of different survival zones based on distance to the vascularized edge providing insight into how parcel size may affect graft survival. The research using cannula size surrogates has not been conclusive and no research exists to date directly examining lobule size in vivo. Further research must be performed to determine the relationship between parcel size and graft survival in vivo.
Aspiration Technique
The amount of liposuction performed depends on the level of lipodystrophy, desired result, and amount of fat needed for grafting. Large-volume liposuction is usually considered to be anything above 5 liters of fat aspiration. These cases should be performed in an acute care hospital or an accredited facility because of the increased complication rates associated with larger volume liposuction. To ensure safety, vital signs, urine output, overnight monitoring, and appropriate fluid replacement are required.
Various aspiration techniques have been developed over the years, including suction-assisted, ultrasound-assisted, water-assisted, and laser-assisted liposuction. Use of either hand aspiration or machine-assisted liposuction is a compromise between efficiency and the risk of adipocyte damage. Early studies in aspiration pressure were based on cell viability with varying pressures. Pu et al found that there was a significantly greater number of viable adipocytes harvested via hand aspiration compared to machine aspiration at no greater than 20 cmH 2 O. In contrary, Lee et al found that there was no difference in graft weight retention or histology between −15 mmHg handheld aspirate and −25 mmHg machine-harvested fat.
Ultrasound-assisted liposuction (UAL) was first described by Zocchi, and it is a result of alternating currents that cause piezoelectric crystals to expand and contract, releasing ultrasonic waves that emulsify fat by micromechanical, thermal, and cavitation action. Our group showed no difference in graft retention in a murine model between UAL and traditional suction-assisted liposuction at 430 mmHg in graft retention or histology. Yin et al compared graft survival between xenografts harvested via water-jet assisted liposuction and traditional liposuction set to −0.5 bar and found significantly improved graft retention and adipocyte viability in the water-jet assisted liposuction group. Laser-assisted liposuction (LAL) uses a laser fiber to disrupt fat cell membranes and emulsifying fat. The most common wavelengths in LAL include 924/975 nm, 1064 nm, 1319/1320 nm, and 1450 nm. Prado et al showed no major differences between SAL and LAL, other than higher concentrations of free-fatty acids after LAL. However, limited conclusions can be drawn given the small sample size.
In the current literature, increased pressure from machine-assisted liposuction does not appear to impact actual graft survival though it may affect cell viability. While many of these studies discuss graft survival, none compares techniques based on esthetic outcomes. Thus the assertion of superiority of nonvacuum techniques on esthetic outcomes is not yet defined. With limited studies, more research should be pursued comparing graft retention based on aspiration method potential comparing hand, machine, ultrasound, water-jet, and laser-assisted liposuction.
Processing Technique
Centrifugation, Filtration, Decanting, and Rolling Techniques
Four primary processing methods have been used clinically to process fat graft: centrifugation, filtration, decanting, and rolling techniques.
Centrifuging has been a mainstay in fat processing as a method of separating viable adipocytes from additional, undesirable lipoaspirate. As a commonly utilized technique, it has been more highly researched with investigation into ideal centrifuge speeds and how the method compares to other processing techniques. , , , Early research into the utility of centrifuging for improving fat graft survival in humans by Butterwick showed that, when compared to noncentrifuged fat, centrifuged grafts to the hand were rated by both patients and physicians as having better retention and more visual improvement as long as months after the procedure. Ferraro et al also utilized digital photography to compare resorption rates in patients grafted with fat centrifuged at 3000 rpm (1500 g ) for 3 minutes, 1300 rpm (250 g ) for 5 minutes, or uncentrifuged and decanted fat injected in the gluteal region and found the lowest resorption rates in the slow centrifuge group and highest in decantation after 12 months. Quantitative research to evaluate the effect of centrifuging speeds on graft survival has been completed in murine models. Using percent oil extracted after centrifuging as a surrogate for adipocyte damage, Hoareau et al determined speeds up to 400 g had little effect on harvested fat whereas a speed of 900 g had significantly damaged adipocytes. On the other hand, higher centrifuge speeds produced more concentrated adipocyte fractions with maximal concentration being achieved at 5000 g . Thus, in determining the ideal speed, concentrating power and cell damage must be balanced to produce optimal graft survival. Kurita et al compared grafts either not centrifuged or centrifuged at 400 g , 700 g , 1200 g , 3000 g , or 4200 g for 3 minutes and found significantly improved retention up to 3000 g , but when balanced with ASC concentration and volume compaction, suggested 1200 g was the ideal speed. Additionally, the group suggested that increased oil isolated above 400 g was due to separation of existing oil rather than cell damage as grafts up to 4200 g were histologically intact. Other studies have suggested the ideal speed to be as low as 698.75 g or as high as 5000 g . , Centrifuging at any speed creates multiple layers of density, which Allen et al compared to determine if the density of the processed fat affected survival. They found that the highest density fraction had significantly higher retention and improved architecture at 2 and 10 weeks.
Centrifuging has also been compared to other methods of processing such as sieves and gauze rolling. When comparing these three methods in a murine model, Minn et al found no significant differences in graft retention or necrosis at 12 weeks, but did find significantly lower in vitro cell viability in the metal sieve group based on XTT metabolization. These results were echoed by Salinas et al when they found centrifuging at 1200 g and mesh/gauze processing produced equivalent graft retention and histology scores in mice at 4 weeks, noting the result was expecting as the two methods achieved the same level of adipocyte concentration. However, Canizares et al found that when compared to centrifuging at 1200 g , telfa rolling produced superior graft retention at 2 and 10 weeks in a murine model as well as adipocyte functionality as determined by glycerol-3-phosphate dehydrogenase assay. Fisher et al similarly found that xenograft retention at 6 weeks for the telfa roll method was superior to both centrifuging via the Coleman method and Tissu-Trans Filtron filtration.
The current evidence suggests that fat should be processed using centrifugation or rolling techniques. However, one must consider the practical aspect of fat processing technique, which must allow feasible workflow in the operating room. For this reason, a surgeon might need to tailor the processing technique based on the volume of fat that needs to be grafted. For instance, smaller volumes can be processed with either centrifugation or rolling techniques; whereas, larger volumes may be more efficiently processed with filtering or decantation.
Washing
Washing serves as another method of processing and purifying lipoaspirate, which is performed often in isolation rather than as an adjunct, by adding and removing solutions. , Girard et al showed improved fat graft retention in immunodeficient mice at 4 weeks, by combining centrifugation with Ringer’s lactate washing. Khater et al found better esthetic results when lipoaspirate was washed 1:1 with physiological serum instead of centrifugation, which they attributed to the noncentrifuged graft’s higher leptin expression and number of preadipocytes as identified by morphology. In a similar study, Botti et al found no difference between centrifuging and washing with normal saline. Condé-Green et al showed that while washing lipoaspirate with normal saline three times in a 1:1 ratio leads to high histological fat graft viability, cell assisted lipotransfer and centrifuged fat graft had significantly more consistent volume retention of 0.3 mL grafts at 12 weeks in immunodeficient mice.
Taken as a whole, current data seems to suggest washing provides comparable retention to other methods of processing but may provide benefits to cell viability. However, further research is needed to determine its superiority.
Pharmacological Additives
A multitude of individual additives have been tested to improve graft retention including IL-8, PDGF, VEGF-loaded microspheres, botulinum toxin-A, M2 macrophages, N-acetylcysteine, phosphodiesterase inhibitors, insulin, EGF, anti-TNF-α improved autograft, bone marrow aspirate or concentrate. These pharmacological additives show promising results. However, the majority of these studies utilize non-ideal methods in their processing and assessment of viability of their grafts. Whereas among those studies that do, the heterogeneity in methodology makes comparison of additives impossible. To determine the true benefits and superiority of additives in the clinical setting, further standardized studies using methods that reduce spurious retention and demonstrate viability must first be pursued.
Injection Technique
The technique employed to inject fat is crucial to optimize the esthetics and retention of the graft. Injection of the processed fat into the recipient site requires significant care to produce long-lasting desirable outcomes. The original technique described by Dr. Coleman uses Luer lock syringes connected to a 17G blunt cannula to inject the processed lipoaspirate. The cannula is withdrawn as the lipoaspirate is injected, in order to allow the grafted fat to fall into the natural tissue planes as the cannula is removed. A fan injection pattern is also recommended because as described by our group the distribution of the injected fat is of utmost importance to survival. , Given the impact of injection pattern on survival, other aspects of injection method have also been researched. ,
Much as with harvesting, a focus on injection technique has been needle size. Erdim et al found no difference in in vitro adipocyte count between 14G, 16G, and 20G injection needle gauges. Their findings were reinforced by Nguyen et al, who found no significant differences in graft retention or histology when comparing injections of 0.7 mL of fat with 17G, 20G, 23G, or 25G needles. Contrarily, Luan et al suggest injection cannula does impact survival, finding that injection of 0.2 mL xenograft through a 14G 8-cm cannula led to significantly better histology than fat injected through longer or narrower cannulas, and that volume retention was significantly better than a 18G 8-cm cannula. Possible differences in outcomes with different injection cannulas have been attributed to shear stress during injection. Lee et al proposed that the increase in shear stress with fast injection rate (3–5 mL/second) over slow injection rate (0.5–1 mL/second) was the cause of decreased retention and histology scores in their – mL xenografts at 4 weeks. Chung et al investigated how a low shear, automated adipose tissue injector device affected grafts, finding a significant increase in in vitro viability and proliferation, and improved in vivo retention and histology at 12 weeks.
While early studies suggested no effect, later investigation using more ideal models demonstrated clear preference toward low-shear stress injection methods. Further research pursuing these methods should be completed in clinical trials to confirm their success.
Recipient Site
Researchers have suggested differences in retention due to recipient site may be due to factors such as site mobility, existing vascularity, and injection effect on architecture. Fat graft retention depends on revascularization among many factors, which means that lipoaspirate injection into a vascularized bed is essential. Karacaoglu et al tested optimal recipient bed by comparing fat grafting in the subcutaneous, supramuscular, and submuscular layer of the buccomandibular area of rabbits, and found that grafting into the supramuscular layer had significantly improved retention and histopathological scores. Shi et al showed that 0.1-mL allografts to the fat pad had the highest weight retention compared to the intramuscular and subcutaneous layers. However, angiogenesis and vascularized connective tissue were more prominent in fat injected in the intramuscular layer, likely being the reason for the highest survival rates among the three recipient sites.
A potential factor impacting graft retention is the degree of mobility of the underlying tissue. The face is a prime example with areas like the glabella and lips that are less amenable to correction, compared to less mobile areas like the malar and lateral cheek.
Denadai et al demonstrated radiologically that fat graft retention was better in the cheek unit at 12 months compared to the forehead or the chin units. Furthermore, Mojallal et al showed in their clinical trial that fat injected to the malar region had significantly better esthetic result than grafts to the temporal and lip areas.
The manipulation of recipient site offers the chance to enhance graft survival and predictability. Much of the research in the area has been dedicated to preexpansion, where the mechanotransduction properties of preexpansion lead to conversion of mechanical tension into growth-promoting signals creating a vascularized scaffold that allows for larger graft volumes and better retention rates. The BRAVA (Brava, LLC, Miami, FL) preexpansion device is a prime example and the benefit of this technology was demonstrated in a prospective multicenter study highlighting the significant improvement in weighted mean graft retention rate and the ability to inject much larger volumes of fat graft. Lee et al used posttransplant negative external pressure on 1-g en bloc autografts, finding a significant improvement at 3 months in the experimental group’s weight retention and viability. Sezgin et al examined the effect of microneedling prior to fat grafting and found that it had significantly better retention and histopathological scores at 15 weeks of 100-mg grafts, but did not find a significant difference in the grafts triglyceride content. By housing posttransplant mice in oxygen-enriched environments, Kato et al investigated the effect of normobaric hyperoxygenation on a perilipin staining and weight retention calculated engraftment score for 0.2-mg murine autografts, proving that this pretreatment significantly increased survival at 12 weeks by increasing the surviving and regeneration zones over the central necrotic zone of grafts.
These techniques are promising strategies to support the recipient bed and should be further explored in human trials.
Intrinsic Patient Variability in Adipose Tissue
The unpredictability of fat graft retention remains a major issue and intrinsic patient factors are likely to play a role. Much of the research into the efficacy of fat grafting has focused on how technique affects graft survival, and only few papers have directly examined the effect of different patient characteristics on the grafts they receive. , , , , Commonly, patient factors will be reported in studies to show standardization between study groups but will not be subject to analysis for potential significance. Furthermore, while some studies have performed patient factor analysis, this is rarely the primary focus of the paper, rather being a secondary finding. Geissler et al examined the fat of 24 female patients harvested from the flanks, lower abdomen, and inner thigh and showed that younger patients had greater adipocyte viability in the lower abdomen than in the flank, whereas older patients did not show any differences. Younger lower abdominal fat showed superior adipocyte viability compared to older patients. However, flank fat had higher adipocyte viability in older patients. Patient weight did not appear to affect adipocyte viability. In the only prospective study found specifically designed to examine the effect of patient factors on graft survival, Dendai et al identified several factors which impacted fat graft survival in patients with unilateral craniofacial contour deformities. The authors identified Parry–Romberg syndrome, previous craniofacial bone surgery, forehead unit, grafted volume, and older age as independently negative predictors of fat graft retention, whereas injection in the cheek unit was an independently positive predictor. It therefore appears that age and underlying pathology of the recipient play a role in adipocyte viability and retention. Another factor that has been studied is exposure to radiation. Choi et al and Small et al found that prior radiation exposure did not significantly affect graft retention over time in breast reconstruction. , However, when radiation exposure was examined in a murine case–control trial by Garza et al, they found radiation to be significantly detrimental to graft survival. Due to this discrepancy, further clinical trials specifically examining radiation exposure are warranted. The role of other factors like gender, smoking, obesity, diabetes, and hypertension on the impact of graft retention and adipocyte viability remains uncertain. Özalp and Çakmakoğlu looked into the impact of smoking on facial fat grafting in their 18-patient retrospective cohort study, and highlighted a low fat graft survival rate and reduced skin quality improvement; however, no controls were included. Jung et al demonstrated in their murine model the negative impact of diabetes on graft retention and histological quality. Whereas Herly et al showed in their long-term retention study that the only factor having a significant positive impact on graft retention was male gender. Among the current literature, there is discrepancy of the impact of variables such as radiation exposure, age, and gender. Larger-scale, prospective human studies specifically examining multiple patient factors are required for the different applications of fat grafting.
Volume Retention Over Time
Animal studies have shown that active remodeling, resorption, and adipogenesis stabilize around the 12-week mark. , How this process of stabilization effects long-term volume retention has been observed in various clinical trials. , , , ,
Early photographic assessment supports the later observed laboratory kinetics, with facial grafting generally stabilizing around 3–4 months and breast grafting around 4–6 months, though there may be subtle volume decreases out to a year. , Denadai et al confirmed these findings in their study, showing with ultrasound measurements a steady decrease of soft tissue thickness over 3 months with no significant decrease after that point out to a year.
Counter to these studies, Herly et al reached steady state point much later, as demonstrated by MRI analysis that loss of <5% original volume per year was not reached until 806 days after grafting. However, this study was performed with en bloc fat grafted to the postauricular region, making it less applicable to routine clinical practice. On the other hand, Choi et al’s fat grafting results reached steady state sooner with larger volume breast grafts nearing stability closer to 49 days while small volumes continued to rapidly shrink out to 140 days. All of the studies that qualified long-term retention found optimal results ranging from 51% to 68%. , These discrepancies in results require clarification with larger-scale prospective trials using lipofilling techniques.
Impact of Serial Fat Grafting
With the uncertainty of graft retention, varying use of multiple injections have been implemented. ,
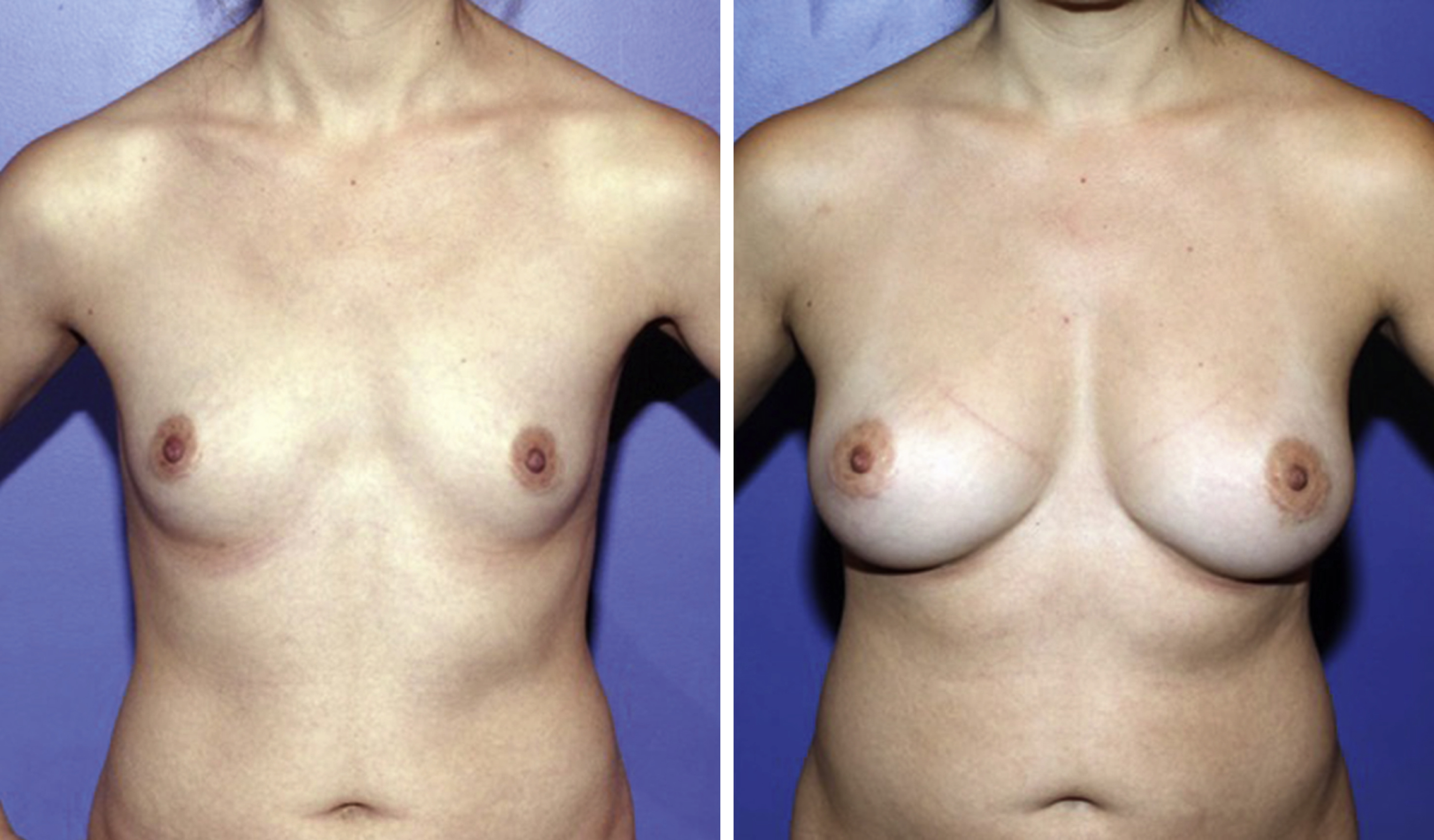
Serial fat grafting is often needed to correct deformities. A prime example is fat grafting for breast augmentation or reconstruction either with or without the use of a preexpansion device ( Fig. 70.1 ). Khouri et al report using between 1 and 10 rounds of fat grafting at a minimum of 8-week intervals to achieve satisfactory results, noting needing more injections in delayed reconstruction and post-radiation patients, and higher volumes injected in later procedures. Kim et al used fat grafting for secondary breast reconstruction, reporting about a quarter of their patients required reinjection due to inadequate volume.