Chapter 38 Liposuction and circumferential lower truncal dermatolipectomy
• The procedure of circumferential lower truncal dermatolipectomy is described and compared to alternative techniques.
• Main technical aspects and refinements are highlighted and described in the clinical context.
• The prevention, reduction and management of complications is demonstrated for this specific procedure.
• The different intraoperative steps are explained and how these enable procedure enhancement.
• The combination of liposuction and lower body contouring procedures has to be performed cautiously and restricted. Therefore, limitations are emphasized.
Introduction
The worldwide population of obese and morbidly obese individuals is growing faster than any other group. Consequently, we have a rapid increase in patients after weight loss, some of them through diet and exercise, and others who undergo a bariatric procedure with more or less irreversible gastrointestinal changes. Therefore, this new subfield of plastic surgery is gaining worldwide acceptance and there are many participating surgeons around the world. Following the establishment of modern body lift procedures by Ted Lockwood in the early 1990s1–5 and the progress in this surgical field, we nowadays benefit from different innovative approaches, which are all based on Lockwood’s philosophy. The main technical aspect, similar to modern face-lifting procedures, is the reconstruction of the superficial and deep connective tissue layers comparable to the superficial musculoaponeurotic system (SMAS) of the face. Nevertheless, it is essential to perform large-area tissue undermining and separation to allow a sufficient tissue mobilization and tightening of the affected areas with respect to an optimal result.
Preoperative Preparation
A precise physical examination and assessment of the medical history is mandatory in every patient. The examination of the lower body should include the upper and lower abdomen, the umbilical region, the midline region in standing and supine position, the flank and hip region with lateral thigh, the inner thigh, and additionally, the entire lower back region. For grading we recommend the Pittsburgh Rating Scale, published by Song et al.6
The ideal patient for circumferential reconstructive surgery meets the following criteria:
• Non-smoker or to quit smoking 6 weeks prior to surgery
• Weight stabilized for at least 6 months prior to surgery
• Highly motivated, athletically and socially stable
• Weight loss through diet and exercise
• Physically and mentally stable
• Circumferential tissue excess
• Maximal deflation of adipose tissue
• Adequate reduction of intraabdominal fat
The first consultation should further include a thorough and detailed explanation of the entire procedure, preferably on PowerPoint® presentations. It is essential to demonstrate complications on images to visualize and emphasize possibilities such as wound separation and impaired scarring. The translation-test by Aly has proven to be worthwhile in clinical practice. The patient is instructed to grasp his tissue surplus at the height of his waist and pull the excess tissue firmly upwards. The visible skin lift and body contour improvement obtained in this way reliably forecasts the outcome of the thigh appearance after lower body lift operations. Optimal results can be achieved with a normal BMI < 25. With a higher preoperative BMI the patient must be informed about an exponentially limited postoperative result. The upper limit for massive weight loss surgery should not exceed a current BMI of 32.7
Further, we endeavor to enhance the patient’s understanding of impaired skin quality due to weight loss and bariatric surgery. In this context, we cite the latest article on this issue and inform every patient about secondary skin relaxation in this specific patient group. Therefore it is not uncommon to perform a secondary tightening procedure in particular cases.8
Markings
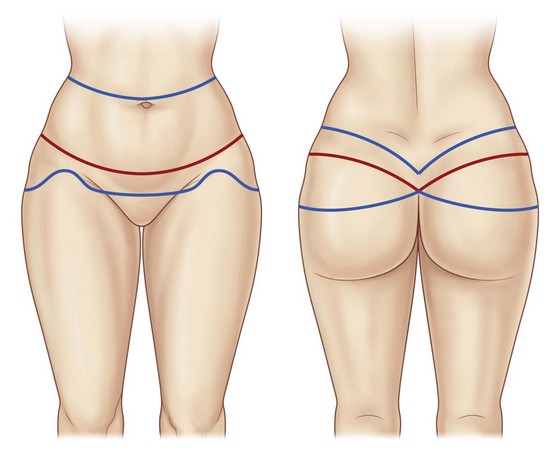
Initially, the boundaries of the patient’s preferred undergarment are marked in the standing position. The desired scar course is marked in red and double-checked by the patient. Dorsal markings are performed first. The posterior upper incision line runs about two to three finger breadths above the desired scar line and is marked in blue. The blue line, along its entire length, is then pulled caudally using the surgeon’s palm and is checked to make sure that it will reach the proposed red line of closure. In general, it should be at the lateral height of the umbilicus. The inferior proposed line of excision is estimated by strongly pinching the skin cranially, ensuring that approximately a quarter of the total resection height lies superior to the red scar line while the lower three quarters are inferior to it. The proposed inferior line of excision is an estimate that may need to be adjusted at the time of surgery. If avoidable, the anal cleft should not be elevated, since an elongation may result in patient dissatisfaction. It has been worthwhile to allow the upper incision line to run at a sharper angle into the anal cleft, in order to achieve an optical accentuation of the buttock form (Fig. 38.1).
Next, the anterior markings are performed based on the frontal red line previously marked (Fig. 38.2). We routinely instruct the patient to firmly and symmetrically pull up the entire abdominal tissue, while we initially mark the midline, a minimal distance of 6 cm from the vulvar commissure (or base of the penis), and next the lower incision line from the midline point laterally, where they are connected to the lower dorsal line. Often the resulting scar line is placed too far cranially due to a lower incision line marked in the abdominal skinfold. Consequently, the mons pubis, which is often sagged and slackened, is not lifted. In more severe cases the lower incision line can be extended caudally in an elliptical or triangle shape into the mons pubis region for an effective local skin tightening. Nevertheless, it is essential to leave a distance of 6 cm to the upper vulvar commissure (or base of the penis) (Fig. 38.3). The upper incision line is then continued from the lateral aspect of the dorsal upper line medially to the height of the umbilicus. In cases of distinct tissue surplus in the upper abdomen we routinely inform the patient about the option of a fleur-de-lis incision pattern during the first consultation. If the patient agrees to this additional scar line, we draw the midline cranially to the xiphoid. The vertical incision line is then evaluated by pinching and marked in an elliptical shape, starting two finger breadths below the xiphoid. This is mandatory to avoid a further cranial scar ending. Also, it is advisable to mark the vertical incision lines in standing position, since the tissue tends to drop laterally and backwards in supine position. The upper horizontal incision line is then marked approximately one finger breadth below the height of the umbilicus.
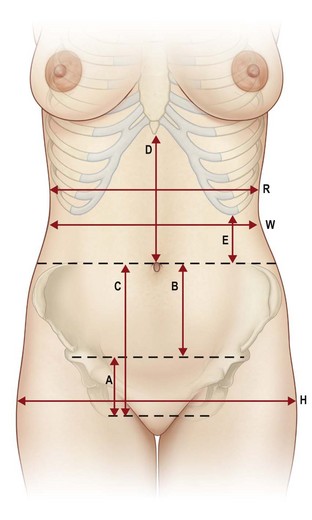
FIG. 38.2 Anatomical landmarks.
(from Richter DF, Stoff A. Abdominoplasty procedures. In: Plastic Surgery 3rd edition (Neligan P ed.) Elsevier, Saunders, St. Louis, 2012, with permission from Elsevier).
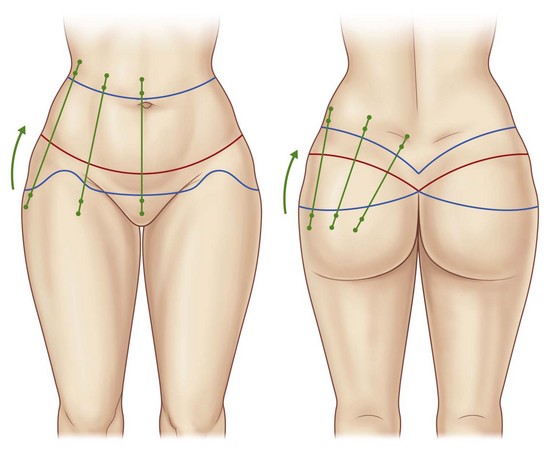
Importantly, dorsal vector lines are marked to allow a mediocranial rotation of the gluteal and thigh region and a consequent sculpturing of the waist (Figs 38.3 and 38.4). A final check of the markings should be performed in the patient’s supine and prone positions.

FIG. 38.4 Intraoperative marking of vectors and intraoperative positioning in prone position (with permission from Elsevier).9
For additional liposculpturing of the flank, back or lateral thigh regions, the markings are made in the typical manner. We advise refraining from excessive liposuction in the undermined gluteal area, since any additional impairment of microcirculation in this area may result in skin necrosis. Patients after massive weight loss frequently present with significant adipose tissue redundancy in the area of the circumferential thighs, we routinely perform widespread tissue reduction by vibration-assisted liposuction in this area during the initial circumferential lower truncal dermatolipectomy.9
General Considerations
Accurate patient positioning is essential for avoidance of scar asymmetry and impairment of tissue perfusion in the areas of maximal pressure. The entire team, including anesthesiologists, surgical nurses and surgeons must constantly and conscientiously check the patient’s positioning. Pressure necrosis can arise around the periorbital regions and at the breasts, particularly in the prone position.10
We routinely install a urinary catheter and wrap the lower legs with compression bandages for deep vein thrombosis (DVT) prevention. Further, we administer a single-shot antibiotic to every patient. In specific cases the postoperative continuation of antibiotic prophylaxis may be considered.11
Surgical Technique
Dorsal Preparation
The initial skin incision (utilizing the cold blade or alternatively the Colorado® Microdissection needle) is made along the superior marking line and is carried out down to the level of the underlying superficial fascia, which is exposed using the Colorado® Microdissection needle or alternatively the Harmonic™ ultrasound scalpel, both of which easily separate the superficial lamellar from the subfascial lobular fat. Next, the dissection is continued inferiorly just above the robust white superficial fascia. The dissection level above the superficial fascia differs considerably from the original technique by Lockwood, who dissected subfascially. The preservation of fascia to the deep gluteal fat as the “gluteal SMAS” is conceptionally similar to the “facial SMAS” used in face-lifts. The superficial fascia is dissected at the height of the inferior resection line, before flap mobilization is continued caudally. Further, this allows a reconstruction of superficial fascia upon wound closure. Lateral gluteal adhesions are released caudally up to the gluteal fold height, before dissection is continued to the lateral thigh, where the preparation level is above the aponeurosis of the tensor fascia lata muscle. Further distal mobilization of the lateral thigh can be carried out bluntly using the Lockwood underminer. With completion of dissection, the waist and gluteal fatty tissue is widely mobilized and covered with robust superficial fascia. This is particularly suited for autologous gluteal augmentations, since patients after massive weight loss frequently suffer from flattened buttocks. For this purpose, two to three 1×0 Ethibond threads (Ethicon, USA) are sutured from lateral to medial, grasping the stable fascia and consequently displacing the gluteal fatty tissue to the middle of the buttock. For cranial repositioning, three to four 1×0 Ethibond threads (Ethicon, USA) are sutured from caudal to cranial at the medial aspect of the buttocks. By reconstruction and tightening of the gluteal adipose tissue, the gluteal flaps are lifted cranially with a consequent final skin closure under less tension. Further, this maneuver is able to improve the shape of the waist (Fig. 38.5).
The detachment in the zones of adherence combined with an extended mobilization allow an enormous tightening of the skin. The stage of resection should always be supervised by the “leading” surgeon in terms of symmetrical resection. We advise to utilize bullet forceps for determination of the amount of resection. The marked vector lines (Fig. 38.4) are incised from medial to lateral and adjusted for maximum tension. The redundant medial, central and lateral gluteal flaps arising in this way are measured precisely in tensed condition for symmetrical resection, which is subsequently carried out between the clamps (Figs 38.6 and 38.7).

FIG. 38.6 Intraoperative demonstration of flap dissection to ensure symmetrical resection (with permission from Elsevier).9

FIG. 38.7 Each flap should be measured in comparison to the contralateral side (with permission from Elsevier).9
Before patients are turned into the supine position we perform a temporary closure of the lateral skin surplus utilizing a stapler and occlusive Opsite® foil.9
Anterior Preparation
Standard Technique
With all techniques the dissection level is performed above Scarpa’s fascia (Figs 38.8–38.10), entailing a number of key advantages: long-lasting swellings can be prevented because the underlying lymphatic vessels are preserved, and the stretching of the SFS craniomedially provides an additional “inner traction” on the deep penetrating fascia system of the thigh. The SFS may then be fixated with 1/0 Ethibond sutures (Ethicon, USA) to the anterior rectus fascia (Fig. 38.11). Approximately three finger breadths below the umbilicus, Scarpa’s fascia is dissected and further mobilization of the abdominal flap is performed cranially on the anterior rectus fascia (Fig. 38.12). The central supraumbilical adhesion zone is sharply dissected between both rectus muscles, preserving the laterally incoming perforator vessels (Fig. 38.13).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree