Legs
OVERVIEW
There are few cutaneous conditions limited to, or particularly characteristic of the thighs; however, eczema and psoriasis commonly appear in this location. The intertriginous inner surfaces of the thighs are subject to heat, moisture, and the friction of undergarments; consequently, many of the resultant dermatoses of this region are considered in Axillary and Inguinal Creases.
The knees and flexor creases of the leg demonstrate localized plaques analogous to those that are found on the elbows and flexor creases of the arms i.e., psoriasis, lichen simplex chronicus, and atopic dermatitis (see Arms).
In contrast, the lower legs have a unique variety of dermatoses that are influenced by such factors as vascular abnormalities that may result in edema, stasis dermatitis, purpura, vasculitis, and ulcerations. Purpuric lesions can be a sign or symptom of other vascular disorders such as a coagulopathy or vasculopathy and may serve as clues to a systemic disease such as systemic lupus erythematosus. Purpuric skin is purple, violaceous, or dark red in color and it does not blanch because blood is present outside the vessel walls. In contrast, erythema that is red in color blanches on compression because blood remains within the vessels.
Red, pinpoint macules (petechiae) or bruises (ecchymoses) are seen most often on dependent areas (i.e., lower legs and ankles and the buttocks in bedridden patients).
Older lesions generally become purple and then turn brown as hemosiderin forms.
Older lesions generally become purple and then turn brown as hemosiderin forms.
Atrophic and ulcerative conditions such as necrobiosis lipoidica, diabetic dermopathy, and pyoderma gangrenosum, as well as various panniculitides such as erythema nodosum, tend to target the thighs and lower legs.
Both upper and lower legs are prone to certain benign neoplasms, namely, dermatofibromas, various melanocytic nevi, and seborrheic keratoses, whereas the more sun-exposed lower legs also tend to develop actinic keratoses, squamous cell carcinomas, as well as melanomas, in susceptible individuals.
THIGHS, KNEES, AND LOWER LEGS
Nummular Eczema
Nummular eczema is commonly noted in adults, many of whom also have an atopic predisposition. It may also be seen in children as a clinical variant of atopic dermatitis. The word nummular comes from the same root as numismatic, meaning “coin-shaped” because lesions are round and have the shape of coins.
Distinguishing Features
Itchy, coin-shaped, scaly, eczematous plaques that tend to occur in clusters (Fig. 18-1)
Appear mainly on the legs; less commonly, they occur on the arms and trunk, particularly in children
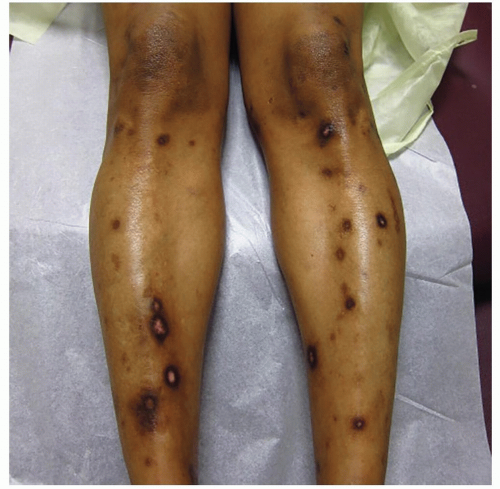
Healing or resolving lesions often display postinflammatory hyperpigmentation, particularly in people of color (Fig. 18-2)
Diagnosis
Based on clinical appearance
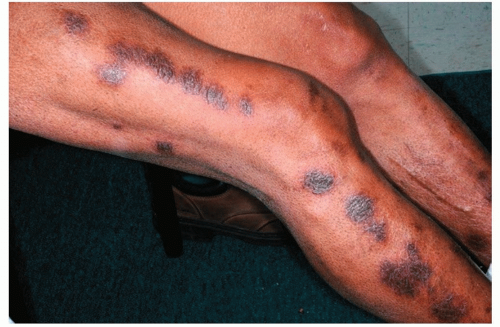 Figure 18-2 Nummular eczema. Coin-shaped, very itchy, scaly lesions with prominent postinflammatory hyperpigmentation. These lesions show lichenification. |
Management
Often can be controlled by an intermediate-strength (class 3 or 4) topical corticosteroid, such as triamcinolone acetonide cream 0.1%, applied two times daily.
If necessary, a high-potency (class 1) topical corticosteroid, such as clobetasol 0.05% cream or ointment applied once or twice daily
Recalcitrant cases may require occlusion—provided by a polyethylene wrap or flurandrenolide tape (Cordran Tape)—or intralesional corticosteroid injections
Prurigo Nodularis
Prurigo nodularis appears most often on the shins and is seen mainly in adults 20 to 60 years of age. The cause is unknown; however, most patients, but not all, have a personal or family history of atopic dermatitis, asthma, or hay fever. It also may appear in patients with systemic conditions causing persistent itching, such as renal failure. It is seen in the same clinical context as lichen simplex chronicus and may be considered a nodular form of it. Prurigo nodularis tends to be one of the more resistant skin conditions to treat.
Distinguishing Features
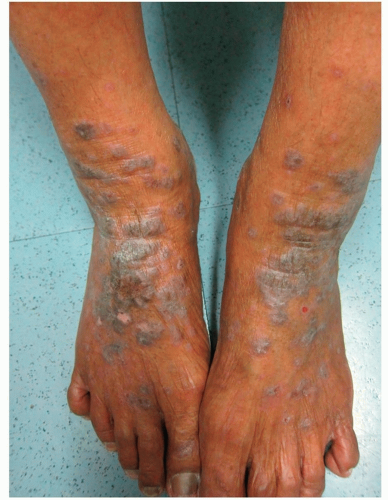
Lesions are reddish, brown, or very darkly hyperpigmented, dome-shaped papules or nodules 1 to 3 cm in diameter (Figs. 18-3 and 18-4)
Symmetrically distributed, most commonly appear on the pretibial shafts, less commonly on the extensor areas of the arms
They are often crusted or excoriated—pruritus may be intense and lead to vigorous scratching and sometimes secondary infection and can also lead to significant emotional stress and depression
Healing results in significant postinflammatory hyperpigmentation
Diagnosis
Clinical
Skin biopsy if the diagnosis is in doubt
Management
Local Treatments
Superpotent (class 1) topical steroid ointments or creams, applied under occlusion (covered with a plastic dressing) to enhance their effect
Cordran Tape
Intralesional corticosteroids
Systemic Treatments
Oral corticosteroids
Phototherapy
Systemic retinoids, such as acitretin, which may shrink the nodules and reduce the severity of the itch
Antidepressants are sometimes necessary
Naltrexone, an opiate antagonist, has been reported to reduce itching in some patients
Thalidomide has been reported as effective in recalcitrant cases
Xerosis
Xerosis, or dry skin, is a common occurrence in winter climates, particularly in conditions of cold air, low relative humidity, and indoor heating. In Western societies, where people tend to overbathe and live in overheated spaces, dry skin is a common complaint. The plethora of moisturizing skin care products are testimony to the prevalence of this condition. Xerosis is believed to be caused by diminished production of sebum (asteatosis), as well as by reduced eccrine sweat activity.
Xerosis becomes especially common in the elderly and tends to be most apparent on the hands and lower legs. The word “dry” is sometimes misapplied. Skin that appears to be dry (i.e., showing a buildup of scale) may not always be suffering from a lack of water but from an overadherence or hyperproliferation of scale, which also occurs in patients with ichthyosis (see below).
Distinguishing Features
Whitish scale
Diagnosis
Clinical
Management
Less frequent showers and baths
Soap avoidance (on affected areas) or mild soaps (e.g., Dove, Basis) or a nonsoap cleanser (e.g., Cetaphil Gentle Skin Cleanser) may be used
Moisturizers help to retain or “lock in” water that is absorbed while bathing; for that reason they should be applied while the skin is still damp
Ammonium lactate 12% lotion or cream (Lac-Hydrin or AmLactin) is an α-hydroxy acid preparation available OTC and via prescription and can be applied after bathing. It is very effective and used for more severe cases of xerosis
Asteatotic Eczema
Asteatotic eczema, also referred to as winter eczema, appears exclusively in adults and most commonly arises on the thighs and shins. This form of eczema is a common, sometimes pruritic, low-grade dermatitis. It is caused by a relative loss of water from the skin through evaporation, a lack of normal desquamation, and, possibly, a decline in the production of sebum.
Distinguishing Features
Scaly, erythematous eruption
Early on, the affected skin feels and looks dry; subsequently, an inflammatory dermatitis may evolve
Seasonal recurrences during dry winter months
Because the skin often resembles the surface of a cracked porcelain vase, it is often referred to as erythema craquelé. It is also likened to the appearance of a dry riverbed (Fig. 18-5)
Diagnosis
Clinical
Management
As with xerosis (see previous discussion), asteatosis is managed with moisturizers
For itching, low-potency to medium-potency (class 4 to 6) topical corticosteroids are helpful for brief periods, when necessary
Ichthyosis Vulgaris
Ichthyosis vulgaris, the most common form of ichthyosis, first evident in early childhood, is a common disorder that is associated with atopy. Inheritance is autosomal dominant. The term ichthyosis is derived from the Greek root ichthys, meaning fish, because of the resemblance to fish scales.
Typically, shedding of skin occurs unnoticed; however, individuals with ichthyosis produce new skin cells at a rate faster than they can shed them or produce them at a normal rate but shed them too slowly. In either case, there is a buildup of dry, scaly skin. Many patients with hereditary ichthyosis vulgaris have associated atopic manifestations (e.g., asthma, eczema, hay fever). Such atopic conditions can be found in family members, with or without signs of ichthyosis.
Distinguishing Features
Symmetric scaling of the skin, which varies from barely visible roughness and dryness to thick horny plates
Lesions are most apparent on the shins, resembling fine fish scales (Fig. 18-6)
Sparing of the flexural folds (e.g., antecubital and popliteal fossae) is an important diagnostic feature (Fig. 18-7)
Scales are small, fine, irregular, and polygonal in shape, often curling up at the edges to give the skin a rough feel
Usually starts in the first year of life, progresses until puberty, then usually improves with age and sun exposure
Diagnosis
Clinical
Skin biopsy is rarely necessary
Management
Hydration of the skin and application of an ointment to prevent evaporation
Ammonium lactate 12% (Lac-Hydrin) or OTC AmLactin is very effective
Tinea Corporis
Tinea corporis (“ringworm”) is most often acquired by contact with an infected animal or human. It may also be autoinoculated from other areas of the body that are infected by tinea. Majocchi granuloma, a variant of tinea corporis, is defined as a granulomatous folliculitis due to a cutaneous dermatophyte infection. Majocchi granuloma is most commonly due to Trichophyton rubrum infection and less commonly to Trichophyton mentagrophytes and Epidermophyton floccosum. Majocchi granuloma tends to occur in women who frequently shave their legs and it also may appear as a result of the use of potent topical steroids on unsuspected tinea, so-called “tinea incognito.”
Distinguishing Features
Lesions may be characteristically annular, with peripheral enlargement and central clearing; however, less well-defined patches, papules, or scaly plaques tend to occur on the legs (Fig. 18-8)
Lesions are single or multiple
If multiple lesions are present, their distribution is typically asymmetric
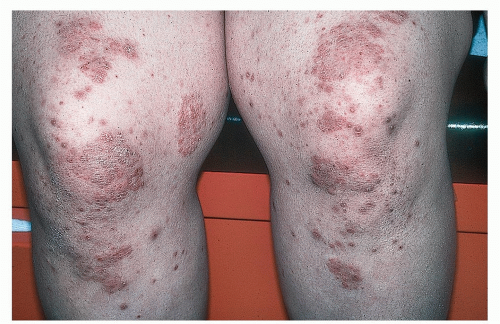
Figure 18-8 Tinea corporis (“incognito”), KOH positive.
This patient was initially treated with topical steroids for what was initially thought to be an eczematous eruption.
May be pruritic or asymptomatic
Majocchi granuloma may result when inappropriate therapy, such as topical steroids, or shaving drives the fungi deeper into hair follicles
Diagnosis
Diagnosis is confirmed by a positive KOH examination or fungal culture
Management
Topical antifungal creams applied once or twice daily are often effective in controlling, and sometimes curing, uncomplicated, localized infections. Preparations such as miconazole (Micatin), terbinafine (Lamisil), and clotrimazole (Lotrimin) are available over the counter
Systemic antifungal agents such as terbinafine (Lamisil), itraconazole (Sporanox), or griseofulvin are sometimes necessary when multiple lesions are present, or in areas that are repeatedly shaved, especially women’s legs
Psoriasis
Localized plaques of psoriasis on the knees (Fig. 18-9) are similar to those on the elbows where they can be quite hypertrophic (see also Figs. 13-5 and 13-6).
Folliculitis
Folliculitis of the legs is seen most often in young adults (see also Mandibular Area and Neck). Causes include actions such as shaving, as well as irritants such as waxing, depilatories, and electrolysis.
Distinguishing Features
Superficial, small, red, relatively asymptomatic papules and/or pustules (Fig. 18-10), often in a grid-like pattern
Diagnosis
Bacterial culture and sensitivity, if necessary
Management
Nonbacterial
Discontinuance or removal of external causes and irritants (e.g., waxing, shaving)
Bacterial
Mild cases of bacterial folliculitis can sometimes be prevented or controlled with antibacterial soaps (e.g., Hibiclens)
Topical antibiotics, such as clindamycin 1% solution, lotion, foam, or gel (Cleocin), may be applied once or twice daily
If staphylococcal colonization is present, mupirocin 2% ointment (Bactroban) may be applied
If necessary, a systemic antibiotic for coverage of Staphylococcus aureus. Dicloxacillin or a cephalosporin is generally the first choice
Lichen Planus
 Figure 18-10 Folliculitis. Note superficial, small red papules with emerging hairs in this young woman who shaves her legs. |
Distinguishing Features
Lesions are pruritic, planar, purple, polygonal, pleomorphic, papules, or plaques that heal with postinflammatory hyperpigmentation.
The presence of Wickham striae, characteristic white streaks on the surface of lesions, and/or the Köebner phenomenon in which new LP lesions appear at sites of scratching (see also Figs. 13-23 and 13-24)
Clinical Variants: Hypertrophic Lichen Planus
Often pruritic, papules or plaques and nodules
Chronic, and tend to heal with residual very dark hyperpigmentation (Fig. 18-11)
Diagnosis
Clinical
Characteristic oral lesions are helpful in making the diagnosis
Skin biopsy is performed, if the diagnosis is in doubt
 Alert: Underlying diseases such as hepatitis C or drugs associated with a LP-like reaction should be ruled out.
Alert: Underlying diseases such as hepatitis C or drugs associated with a LP-like reaction should be ruled out.Management
High-potency (class 2) or superpotent (class 1) topical steroids may be used alone or with polyethylene occlusion, or with Cordran Tape
Intralesional corticosteroids
Systemic steroids
Oral acitretin (Soriatane), cyclosporine, psoralen with ultraviolet A (PUVA) therapy, and griseofulvin have been reported to be occasionally helpful
Erythema Nodosum
Erythema nodosum (EN) is a type of panniculitis, an acute inflammatory reaction of the subcutaneous fat. It is considered a delayed hypersensitivity reaction to various antigenic stimuli. EN is three times more common in females than in males and has a peak incidence between 20 and 30 years of age.
The most common causes of EN in the United States are sarcoidosis, streptococcal infections, pregnancy, and the use of oral contraceptives. In children, streptococcal pharyngitis is the most likely underlying cause. Approximately 40% of cases are idiopathic. EN also is associated with a variety of other conditions: deep fungal infections in endemic areas, including coccidioidomycosis, histoplasmosis, and blastomycosis; tuberculosis; Yersinia enterocolitica infection; inflammatory bowel disease, including ulcerative colitis and Crohn disease; malignant disease, including lymphoma and leukemia; post-radiation therapy; and Behçet syndrome. In addition, drugs such as sulfonamides, penicillin, gold, amiodarone, and opiates have been implicated as causes of EN.
Distinguishing Features
Lesions begin as bright red, deep, extremely tender nodules (Fig. 18-12)
Tends to occur in a bilateral distribution on the anterior shins, thighs, knees, and arms
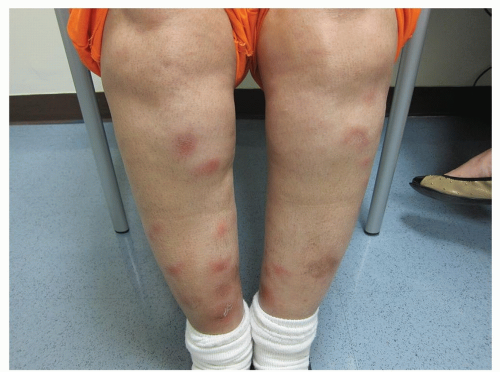
Figure 18-12 Erythema nodosum, acute.
These tender, red nodules appeared after this patient began taking an oral contraceptive.

Figure 18-13 Erythema nodosum, healing.
Resolving “contusiform” lesions are present in this patient.
(Image courtesy of Robert I. Rudolph, MD.)
During resolution, lesions become dark brown, violaceous, or bruise-like macules (“contusiform”) (Fig. 18-13)
Malaise, fever, arthralgias, and periarticular swelling of the knees and ankles may accompany the panniculitis
Other symptoms may also be present, depending on the cause of EN
Spontaneous resolution of lesions occurs in 3 to 6 weeks, regardless of the underlying cause
Generally, EN indicates a better prognosis in patients who have sarcoidosis
Diagnosis
The diagnosis of EN is usually made on clinical grounds, but a biopsy may be helpful for confirmation
Management
If indicated, a complete blood count, erythrocyte sedimentation rate, throat culture, anti-streptolysin titer, Yersinia titers, PPD skin test, and chest film are performed
Treatment is symptomatic, consisting of bed rest and leg elevation for severe EN
Firm supportive bandages or stockings may be worn
Aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs)
A course of potassium iodide may be effective in clearing EN
Further tests, such as gastrointestinal tract evaluation and serum angiotensin-converting enzyme determination, can be performed if suggested by the review of systems and physical examination
Systemic corticosteroids, which often bring dramatic improvement, can be used if an infectious cause is excluded
Ultimately, treatment or avoidance of the underlying cause, if discovered, should be attempted
Nodular Vasculitis
Nodular vasculitis is an idiopathic panniculitis and vasculitis. When associated with Mycobacterium tuberculosis, it is known as erythema induratum. Erythema induratum is due to the tubercle bacillus and is rare in Western countries. Nodular vasculitis refers to the idiopathic type.
Distinguishing Features
Crops of small, tender, erythematous nodules may be observed
Both nodular vasculitis and erythema induratum are most often seen in females
The lower extremities are the most common sites for lesions to arise—often the calves. However, the shins (Fig. 18-14) and ankles also are sometimes involved
Lesions ulcerate, resulting in permanent atrophy scarring and hyperpigmentation
The nodules have a chronic, recurrent course