Le Fort III Advancement
Ghassan S. Abu-Sittah
Rawad S. Chalhoub
DEFINITION
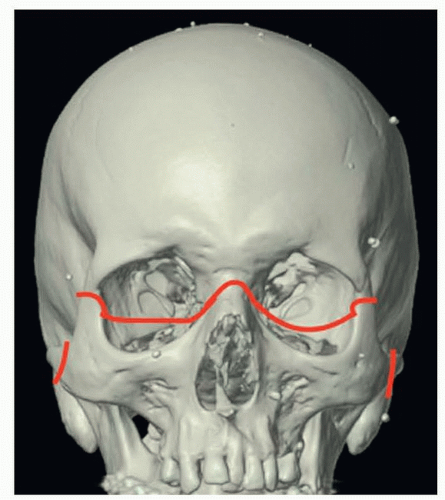
Le Fort III, first described by Rene Le Fort in 1901, is a pattern of craniofacial fractures that involves the nasofrontal suture, traverses the orbital floor, and crosses the zygomaticofrontal suture and zygomatic arch (FIG 1).1
In the 1960s and 1970s, Gillies and Tessier applied Le Fort’s classification to facial osteotomies for the treatment of patients with midface hypoplasia.
Le Fort III osteotomy with advancement, also known as craniofacial disjunction, is currently used for the correction of functional and aesthetic problems in patients with craniofacial dysostosis syndromes such as Crouzon, Apert, or Pfeiffer syndromes.
These conditions usually present with midfacial retrusion, shallow orbits, exorbitism, malocclusion, obstructive sleep apnea, and facial imbalance (FIG 2).
Le Fort III advancement restores normal midface projection, re-establishes normal dental occlusion, increases the vertical dimensions of the face, and corrects exorbitism.
ANATOMY
Normal facial growth depends on the coordinated expansion of the brain and overlying skeletal elements.
The skull is relatively well developed at birth to protect the brain, whereas the facial skeleton continues to grow during childhood to accommodate dental development, orbital modeling, and airway formation.
Cranial dysostosis describes syndromic craniosynostoses in which suture involvement includes the cranial vault, cranial base, and midface skeletal structures.
Midface skeletal hypoplasia leads to both functional and cosmetic problems.
Le Fort III advancement is generally required in these patients.
PATHOGENESIS
Mutations of FGFR genes 1 to 3 lead to syndromic craniosynostoses, including Apert, Pfeiffer, Crouzon, Beare-Stevenson, Jackson-Weiss, Crouzon with acanthosis nigricans, and Muenke syndromes.2
Environmental causes include paternal occupation, maternal age, exposure to tobacco smoke, and medications during pregnancy, including nitrofurantoin and warfarin.3
NATURAL HISTORY
Craniosynostosis occurs in an estimated 1 out of every 2000 live births; it can occur as an isolated condition or part of a syndrome.
Syndromic craniosynostosis affects 1:30 000 to 1:100 000 live births.4
The midface hypoplasia in these conditions is progressive, becoming more noticeable as the patient grows.
PATIENT HISTORY AND PHYSICAL FINDINGS
Craniofacial dysostosis patients suffer from a series of sequelae from growth abnormalities.
Increased intracranial pressure (ICP) can occur as a result of the rapidly growing brain during infancy with limited space for expansion.
Untreated ICP can cause papilledema and optic nerve atrophy, which can eventually lead to blindness.
Vision problems may also occur secondary to exorbitism (exophthalmos) leading to corneal exposure with ulceration.3
Dental, occlusal, and hearing deficits are higher in patients with craniofacial dysostosis than in the general population.2
The most severe consequence of midface deficiency is obstruction of the developing airway, with narrowing of nasal and nasopharyngeal spaces, leading to increased airway resistance.5
Newborns are obligate nasal breathers; airway obstruction forces them to breathe through the mouth, resulting in an inability to feed and breathe simultaneously. These newborns are at high risk for malnutrition and failure to thrive.
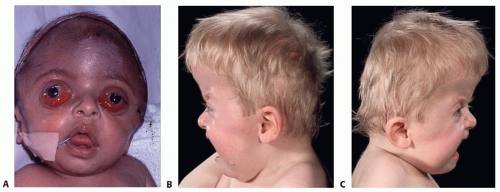
FIG 2 • A. Exorbitism secondary to shallow orbits. B,C. Lateral views of a patient with Apert syndrome. Midfacial retrusion and shallow posterior fossa are evident.
Patients with severe symptoms, generally obstructive sleep apnea or exorbitism, may require a combination Le Fort III advancement with cranial advancement. Monobloc advancement is preferentially performed as a distraction procedure.6
Patients who are mildly affected undergo Le Fort III advancement at skeletal maturity.
IMAGING
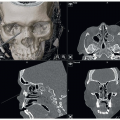
Preoperative imaging required for patients undergoing Le Fort III advancement includes
Anteroposterior and lateral x-rays
Panoramic x-rays
Two-dimensional (2D) and three-dimensional (3D) CT scans (FIG 3)
These images will demonstrate midface hypoplasia, as well as the various anomalies associated with the cranial sutures.
CT scans are the preferred imaging modality and can be used with computer-aided design and modeling for preoperative planning to optimized the surgical approach.7
SURGICAL MANAGEMENT
In planning and timing of the Le Fort III advancement in patients with craniofacial dysostosis, the experienced surgeon should take several factors into account.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree