In the last 5 years the Latino population seeking cosmetic treatments has substantially increased, and one of the main cosmetic concerns of this group is pigmentary disorders, with melasma being the primary clinical condition. It has been reported that the incidence of facial melasma induced by pregnancy in Mexican women can be as high as 50%.1 Other common cosmetic concerns are sunspots, acne scars, enlarged pores, and aged skin.
Latinos come from a mix of various cultures and races. In the pre-Hispanic world, from northern Mexico to southern Chile and Argentina, the local population was already diverse in race and culture. Then various European races came to the Americas and started mixing with the local people. The result was the mestizo population from the combination of Spanish, French, German, and African peoples with an already diverse native Central and South American population. “Latino” also defines all Hispanic and Latin American people. According to the last U.S. census, it is the fastest growing minority in the United States. Latinos are a group of many different, rich cultures and strong traditions. In 2013, the Associated Press reported that one half of the population in the United States under age 5 was composed of ethnic minorities. This means that in three decades, one half of the population of the United States will be non-White Americans.
Patient education is a key element in treating Latino patients and dark-skinned patients. It is mandatory that they understand how their skin can react to light-based treatments or chemical peels. They must be made aware of the risks and benefits attendant to each procedure. Latin people have a tendency toward excessive sun exposure without proper sunblock. Many believe that their darker skin will protect them from the sun, and most Latino men do not like to wear creams on their faces, including sunblock. Ethnicity and culture play important roles in how people perceive beauty and how they take care of their skin.
The authors’ practice is located in Hermosillo, Sonora, Mexico (northern Mexico, in the Sonoran Desert where the temperature reached 118°F in 2013, the area’s hottest day on record). Most, if not all, of the authors’ patients are mixed races with Fitzpatrick skin types IV to VI. The main conditions for which they seek cosmetic treatments are melasma, sunspots (▶ Fig. 33.1), acne scars (▶ Fig. 33.2 and ▶ Fig. 33.3), enlarged pores, and aged skin (▶ Fig. 33.4). The authors have been using fractional lasers since 2008. The experience in the practice has been with the Fraxel Restore erbium:yttrium aluminum garnet (Er:YAG) 1,550-nm laser (formerly Reliant; Solta Medical, Hayward, California) and the AcuPulse carbon dioxide (CO2) fractional laser (Lumenis Inc., Palo Alto, California).

Fig. 33.1 (a) Hands of a 55-year-old patient before carbon dioxide (CO2) fractional laser treatment for sunspots and wrinkles. (b) Same patient after CO2 fractional laser treatment with Lumenis AcuPulse (Palo Alto, California) spot treatment on the sunspots’ settings doughnut shape in smallest size, energy 17.5 mJ, 5% density; deep fractional full-hand fractional settings 10 mJ, 10% density; and superficial treatment settings 100 mJ, 40% density. Improvement is seen in skin texture and sunspots.
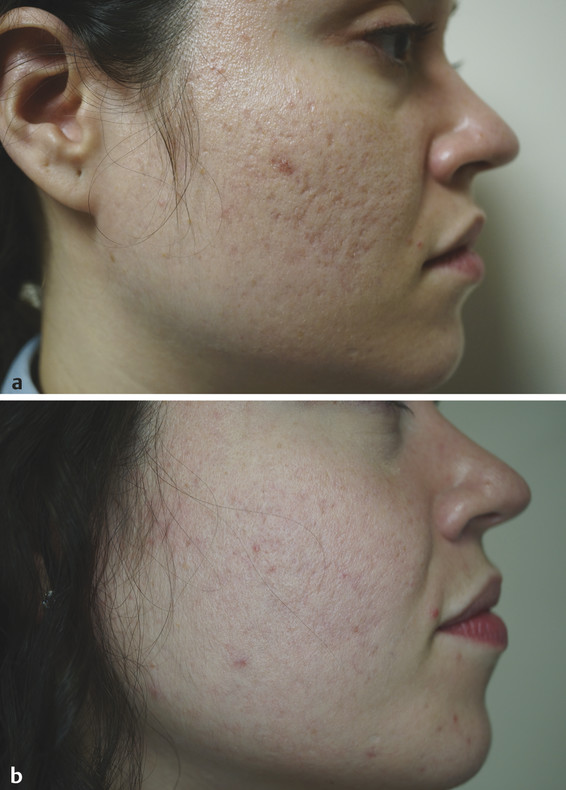
Fig. 33.2 (a) A 25-year-old Fitzpatrick skin type IV patient with deep acne scars before carbon dioxide (CO2) fractional laser treatment. (b) Same patient after CO2 fractional laser treatment with Lumenis AcuPulse (Palo Alto, California) spot treatment on the scars’ settings doughnut shape in smallest size, energy 22.5 mJ, 5% density; deep full-face fractional settings 12.5 mJ, 10% density. Improvement on acne scars and skin tone can be seen.
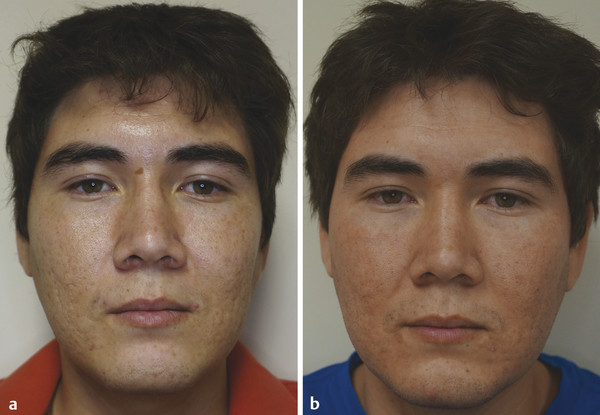
Fig. 33.3 (a) A 23-year-old Fitzpatrick skin type IV patient with deep acne scars and sunspot on the nose before carbon dioxide (CO2) fractional laser treatment. (b) Same patient after CO2 fractional laser treatment with Lumenis AcuPulse (Palo Alto, California) spot treatment on the scars’ settings doughnut shape in smallest size, energy 22.5 mJ, 5% density; deep full-face fractional settings 12.5 mJ, 10% density; and superficial treatment settings 90 mJ, 40% density. There is improvement in acne scars and skin texture; the sunspot on the nose has almost disappeared.

Fig. 33.4 (a) A 55-year-old Fitzpatrick skin type IV patient with photodamage, wrinkles, enlarged pores, acne scars, and sunspots before carbon dioxide (CO2) fractional laser treatment. (b) Same patient after CO2 fractional laser treatment with Lumenis AcuPulse (Palo Alto, California) spot treatment on the scars’ settings doughnut shape in smallest size, energy 17.5 mJ, 5% density; deep full-face fractional settings 12.5 mJ, 10% density; and superficial treatment settings 90 mJ, 40% density. Improvement shown in acne scars, skin texture, fine wrinkles, photodamage, and skin tone.
33.1.1 Latino Skin Considerations
The skin has 3 layers: epidermis, dermis, and subcutaneous.2 The epidermis is composed of the stratum corneum, stratum granulosum, stratum spinosum, and stratum basale. It has four cell types: keratinocytes, melanocytes, Langerhans cells, and Merkel cells. The stratum corneum, the outer layer of the epidermis, contains the nonliving cells (corneocytes) with a bilipid membrane that surrounds them. It is considered the epidermal barrier. This physical barrier maintains skin hydration, prevents evaporation, and is a defense barrier for microorganisms, ultraviolet light trauma, and so forth. The epidermis renews itself every month. During this process, the living keratinocytes migrate from the basal layer of the epidermis to become the corneocytes of the stratum corneum on the surface. They will ultimately desquamate.2,3 Melanin is mainly found in the epidermis; it can also be found in the dermis in some skin conditions such as melasma.2,3,4
33.1.2 Anatomical Differences of Darker Skin
In darker skin types eumelanin is more prominent; this is a darker melanin that goes from brown to black. In lighter skin types pheomelanin, a lighter melanin that goes from yellow to red in color, is more predominant. Melanogenesis occurs in melanocytes in the basal layer of the epidermis; a similar number of melanocytes are found in light and dark skin types. The difference is the type of melanin that predominates. In darker skin types, melanin is stored in large, single melanosomes containing darker melanin, and in light skin types melanin is stored in clustered, small melanosomes containing light-color melanin. Dark skin types have more melanin per square inch of skin.2,4
There are other differences between dark and light skin. Dark skin has more cell layers in the stratum corneum with higher lipid content and is more compact than in lighter skin types. Darker skin types also have a more compact and thicker dermis than lighter skin types. The thickness is proportional to the degree of pigment; also, darker skin types have prominent, thicker dilated blood vessels. The fibroblasts are larger in size and number in darker skin. These cells are responsible for synthetizing the main structural elements of the dermis but they also influence how skin scars; therefore, they have an important role in hypertrophic scars and keloid formation in darker skin types.2,4
33.2 Fractional Lasers in Latino Skin
The use of fractional lasers in Latino patients has always been a challenge―even with the use of pretreatment regimens with hydroquinone, alone or in combination with retinoids and corticosteroids, to avoid postinflammatory hyperpigmentation (PIH) or worsening of melasma. The first fractional laser that was available was the erbium 1,550 and it promised hope in the treatment of melasma and hyperpigmentation disorders in darker skin types, and was Food and Drug Administration (FDA)-approved for this purpose.5,6 Short-term follow-up studies claimed its efficacy, but medium- and long-term follow-ups were disappointing.7 The fractional ablative CO2 laser has become the “gold standard” in facial rejuvenation and skin resurfacing.8,9
33.2.1 Fractional Laser Concepts
Thermal Relaxation Time of Tissue
The thermal relaxation time of tissue is the time it takes tissue that has received laser energy to lose one half of the generated temperature, 0.8 ms. This means that the laser has to deliver the energy in less than 0.8 ms to avoid thermal damage to surrounding tissue.10
Photothermolysis―Nonablative Fractional Resurfacing
The erbium 1,550-nm Fraxel Restore (Solta Medical) is in the near-infrared wavelength. Its chromophore is water.11 It works by laying abundant microscopic zones of thermal damage in columnar fashion, leaving the surrounding tissue of each column damaged and the stratum corneum intact; the remaining undamaged tissue will migrate to the damaged zones to accelerate healing.8 This device has the ability to control the diameter and depth of each microthermal zone, as well as the density of each treatment. It covers 15 to 20% of the skin at a time.6 Following the treatment, microscopic epidermal necrotic debris (MENDs) will form just below each column of coagulated tissue and will be extruded in 5 to 7 days.6 During each treatment, the handpiece must pass eight times over each area of the face, causing elevation of the skin temperature eight times in a procedure. It requires one session per month for five to seven months, depending on the skin condition to be treated.
Ablative Fractional Resurfacing
The wavelength of the CO2 laser is 1,064 nm. This wavelength is highly absorbed by water. Human skin is 60 to 70% water. The laser creates small columnar holes of vaporized tissue surrounded by undamaged tissue that will help the healing process.12 The AcuPulse CO2 device (Lumenis) has the capability to deliver superficial and deep treatments with a single scanner. The deep treatment has a superpulse mode and a 0.12-mm spot size. For the superficial mode the system takes the 0.12-mm spot size and draws a spiral 1.3-mm superficial spot. Neither in the deep nor the superficial mode does the AcuPulse compromise the thermal relaxation time of tissue as ablation occurs.9,11 Thus the possibility of thermal damage to the surrounding tissue and the risk of PIH are minimized.
Preparation of Latino Skin Patient for Fractional Laser Treatment
The preparation of the skin takes at least 4 weeks prior to the treatment.13 In this period of time it is crucial to avoid ultraviolet radiation exposure. The use of sunblock with at least sun protection factor (SPF) 60 every 3 or 4 hours during daylight is advised. The daily, bedtime application of a bleaching cream containing hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% (Tri-Luma; Galderma Laboratories, Fort Worth, Texas) is encouraged. This triple combination therapy has been the gold standard in the treatment of melasma, and its principles also apply to PIH.14,15 It is believed that using hydroquinone for a period of 4 weeks will inhibit the melanocyte activity and melanin formation during the inflammatory phase of the laser treatment.10
Suggested Pretreatment Regimen
Avoid sun exposure 4 weeks before and 6 months after fractional laser treatment.
Use sunblock SPF 60 or higher every 3 to 4 hours during daylight, 4 weeks prior to treatment and 4 to 6 months after.
Use hydroquinone triple therapy 4 weeks before and 4 months after procedure.10
Topical Anesthesia
Cleanse the skin with neutral soap and water, so there are no residual creams and makeup; dry the skin completely to apply topical anesthesia. The authors use a compound pharmacy gel that consists of benzocaine 20%, lidocaine 7%, and tetracaine 7% (BLT). Apply this in a circular fashion giving a gentle massage, so the anesthetic penetrates the skin better. Apply an even coat (as demonstrated in Video 33.1) to the whole area to be treated and let it sit for 1 hour. The authors also give patients 1.5 g of acetaminophen 1 hour before the procedure to reduce discomfort. Side effects of BLT gel can go from allergy to death,16 and have a direct relation to the size, surface area, body location, the amount of product used, and length of time of skin contact; do not apply BLT to extensive or multiple areas at the same time. Check on the patient every 10 minutes; after an hour remove the BLT gel completely before starting the treatment.16,17
Use of Chillers
The authors use a Zimmer (Zimmer Cryo; Zimmer Medizin Systems, Irvine, California) chiller machine routinely. It is used at level 4 or 5 and moved around the treatment area at a distance of 10 cm from the skin to reduce heating and patient discomfort. Do not use the Zimmer at higher settings or too close to the skin because there has been reported PIH due to overcooling.18
Use of Smoke Evacuator
The authors use a Buffalo Filter Smoke Evacuation System with a ViraSafe 6 filter (Tekyard, Burnsville, Minnesota) that provides safety to clinical personnel and patients by preventing potential virus particles in the plume from floating around the procedure room.
Treating Latino Skin with Fractional Erbium 1,550-nm Laser
With the erbium 1,550-nm laser, the authors use low energy and low-density settings. The passes are carried out slowly. This ensures minimum heat diffusion to the skin. The Zimmer (Zimmer Medizin) skin chiller is set at low settings to avoid overcooling and subsequent skin damage. On small areas wait for a couple of seconds between each pass; do not perform more than one pass on Fitzpatrick skin types V and VI, and wait at least 6 to 8 weeks between treatments.10
Treating Latino Skin with CO2 Fractional Laser
In the case of a CO2 fractional laser, do a single pass, do not overlap passes, and use a superpulse or ultrapulse laser that does not compromise the thermal relaxation time.9 Use low-fluence, low-density settings. Air skin cooling is advised at a low setting because overcooling can also trigger PIH.18 In Fitzpatrick skin types IV and V with acne scars (▶ Fig. 33.2 and ▶ Fig. 33.3) or sunspots (▶ Fig. 33.1), we tailor the therapy, treating the scars or sunspots directly with the doughnut shape at the smallest size that will fit each acne scar. We spot treat at a higher energy but lower density (17.5–22 millijoules [mJ] and 5% density on the Lumenis AcuPulse), and treat the rest of the face at lower energy and lower density levels (10–12.5 mJ and 5–10% density on the Lumenis AcuPulse). This allows us to address the specific problem with adequate energy and avoid PIH for the rest of the face.
Fractional Laser for Fitzpatrick Skin Type VI
A different approach is used for Fitzpatrick skin type VI patients seeking fractional laser treatments. For scars or pigmentary disorders, the laser settings are below clinically noticeable results and the risk of complications such as PIH is still considerable. The authors prefer a series of superficial peels and topical bleaching treatments in this group of patients. Fillers are used in scars, sometimes combined with subcision, or punch elevation, or resection techniques.19
33.3 Chemical Peeling in Latino Skin
The authors always start on the safe side with chemical peels in any skin type. With chemical peels, do superficial peeling first. Once a comfort level has been attained with this type of peeling, advance to the medium chemical peels. When enough experience has been gained, graduate to the deep chemical peels. There will be less complications and better outcomes. The senior author does not recommend deep peels in Fitzpatrick skin types V and VI, as well as in patients with a history of PIH following cosmetic treatments, and hypertrophic or keloid scars. It is better to go slowly toward your clinical goal then to head rapidly into a cosmetic disaster.
Training is key to good outcomes when it comes to facial cosmetic procedures. The best investment you can make is in education and training. There are many organizations including the American Society for Laser Medicine and Surgery, the American Academy of Facial Plastic and Reconstructive Surgery, and the American Academy of Dermatology that offer educational meetings and training. It is critical to have proper training and have someone with experience to rely on when you are first starting.
The most common issue in Latino skin is melasma.20 This condition is an acquired dysfunction in the pigmentary system characterized by blotchy, brown macules distributed symmetrically on the face; it is most common in Fitzpatrick skin types IV to VI.20 Its treatment is still a challenge to the dermatologist and the facial plastic surgeon. Sometimes aggressive procedures can make it worse. A multitreatment approach, combining chemical peels, lasers, topical therapies, and photoprotection, has proven to be more promising but not a cure.20,21
33.3.1 Pretreatment Regimen
As with lasers, it is important to prepare the skin before a chemical peel. In the case of chemical peels, it is not only to prevent PIH but also to reduce seborrhea and thin the epidermis. This allows a better and more uniform penetration of the peeling agent.21 Hydroquinone, tretinoin or glycolic acid as a topical depigmenting agent is applied at least 2 weeks before the peeling. In patients with a history of herpes simplex, antiviral prophylaxis is indicated and active acne should be treated prior to the procedure. Antibiotics can be used to prevent a breakout.21
33.3.2 Chemical Peeling Agents for Fitzpatrick Skin Types IV to VI
There are a great many chemical peeling agents available, but the choice of these agents in darker skin types is limited due to their depth of penetration. Deep chemical peels are not recommended for Fitzpatrick skin types IV to VI.20 Medium-depth peels should be used with extreme caution because they can lead to permanent hyperpigmentation and hypertrophic scarring.2,17,20
Superficial Chemical Peels
The superficial chemical peels penetrate the epidermis and upper papillary dermis. They renew the epidermal layer of the skin where most of the pigment is found. They help dyschromias and improve sun damage, superficial wrinkles, acne control, and oily skin. They aid in evening out the skin tone, and represent little risk of PIH for the patient. In this category, the traditional glycolic acid peels have proven to be safe and effective. In the authors’ practice, superficial peels are the most commonly used peels, particularly glycolic acid peels at a 50% concentration at a 3- to 5-minute end point when used alone.20,21,22 In combination with microdermabrasion, the authors use the HydraFacial MD System (Edge Systems Corp., Signal Hill, California) (see Video 33.2) and their peeling formulas, which combine glycolic acid with salicylic acid in various concentrations that range from 7.5 to 30% glycolic acid and 2% salicylic acid. The authors like this system because the hydramicrodermabrasion is less irritating than dry microdermabrasion. The skin abrasion and the peeling are not that aggressive; nevertheless, together the desirable results can be achieved with no complications and no discomfort for the patient. It is very safe for dark skin types. The authors have not yet seen any complications with this system because the superficial peels and the HydraFacial treatments must be repeated in a series of sessions 3 weeks apart until the desired outcomes are obtained. The superficial peeling agents that are safe in dark skin types are glycolic acid solution, 30 to 70%; trichloroacetic acid (TCA), 10 to 30%; salicylic acid, 20 to 30%; Jessner’s Solution; and tretinoin 1 to 5%.2,20,23
Alpha Hydroxy Acid Peels―Glycolic Acid and Lactic Acid
Alpha hydroxy acid (AHA) peels work by producing epidermolysis (corneocyte detachment), dispersing basal cell melanin, thinning the epidermis, and increasing collagen synthesis in the dermis.21 These peeling agents are very safe to use in Latino skin when applied properly; a clinical end point of 3 to 5 minutes is advised.2,20,21,24
Beta Hydroxy Acid Peels―Salicylic Acid
Beta hydroxy acid (BHA) peels are lipophilic compounds that remove intracellular lipids that surround the epithelial cells. Salicylic acid stimulates the basal cells and underlying fibroblasts without directly wounding the dermis or causing inflammation.20,21,24 That is why all BHAs are safe to use in Fitzpatrick skin types IV to VI. They are used to treat acne, melasma, and PIH.
Trichloroacetic Acid Peel
Low concentrations of TCA (10–35%) can penetrate down to the upper papillary dermis. TCA works as a protein denaturant that precipitates epidermal proteins and produces dermal inflammation. The coagulation of epidermal keratinocyte proteins appears as frosting,21,24 which is the clinical end point of TCA peels. This is difficult to appreciate in darker skin and can lead to overpeeling that has a high risk of scarring and postpeel dyschromias. Despite these considerations, TCA peels are considered safe to use in darker skin types. They require a longer preconditioning of the skin and the use of low-concentration TCA. As with lasers, spot treatment can be done with TCA peels. For example, they can be applied inside ice-pick acne scars with a toothpick or a small brush to treat just the scars, and the rest of the face can be treated with a superficial peel. This lowers the risk of PIH.19,24
Jessner’s Peel
The Jessner’s Peel is a combination of 14 g resorcinol, 14 g salicylic acid, and 85% lactic acid in a 100-mL ethanol solution. It is used as a superficial peeling agent in all skin types. It is also used in combination with other peeling agents such as TCA peels, allowing a more uniform penetration at a safer, lower concentration of TCA.20,21,24
Tretinoin Peel
Also known as retinoic acid (vitamin A), tretinoin peel is available from 1 to 5%, increases the stratum corneum, decreases epidermal thickness, and causes melanin dispersion; it can also be used in combination with other peeling agents.20,21,24
33.3.3 Application Technique for Superficial Peels
Clean the skin with neutral soap and water and remove any oil left in the skin with acetone. Then with a piece of soaked gauze or a small brush apply an even coat of the chemical peel. Erythema or frosting will appear on the skin depending on the peeling agent used. That is the clinical end point of the superficial peel. Another clinical end point can be a period of time, for example 3 to 5 minutes. Some superficial peels do not need to be neutralized and others will need to be neutralized with saline, water, or an alkaline substance such as 1% bicarbonate solution. Some erythema and desquamation during the following days can be expected. Sun avoidance and sunblock are recommended. No other extra care is needed. The peel can be repeated every 2 to 3 weeks until the desired result is achieved.20,21,25
33.3.4 Superficial and Medium Chemical Peels’ Complications
Most of the complications of these types of peels are transitory. The most common is hyperpigmentation, more frequently seen in darker skin types due to a deep peel or improper postpeeling care and poor sun protection. Hyperpigmentation can be managed with hydroquinone, kojic acid, or retinoids alone or in combination with corticosteroids. It usually resolves in 1 to 3 months depending on the severity of the case. The use of intense pulsed light (IPL) is controversial. There are some IPL filters that are pigment-specific, but IPL can also worsen the pigmentation.17,20,21,23 Persisting itching and burning sensations can be issues. Advise the patient not to scratch or touch the face. Antihistamines and topical creams containing steroids and antibiotics can be used to minimize discomfort. For accidental eye involvement, rinse abundantly with tap water and refer to an ophthalmologist.17 Prolonged erythema can be managed with topical steroids and proper sunblock applied every 4 hours. Camouflage mineral makeup with sun protection is advised. Systemic steroids may also be used. Exudative lesions, if not treated promptly, may lead to scarring. These can be treated with 3% boric acid solution, topical antibiotics and steroids, and moisturizers; total sun avoidance is also important.2,17
Hypopigmentation is a complication most notorious in dark-skinned patients but it can affect any skin type. This condition is usually permanent; camouflage makeup can be used. Sometimes skin needling, micro-grafting, or a tattoo applied to the affected area can help. Hypertrophic scars should be treated immediately. Silicon gel sheets can be applied for 6 months, then intralesional triamcinolone acetonide 10 to 40 mg/mL at 4- to 6-week intervals. Alternatively, in case of hypertrophic scars, wait for 2 months after peeling and treat with fillers or needling. Frequent patient visits for observation are advised when treating darker skin types; early detection of complications and signs that there may be an impending complication are imperative signals to start early treatment. Most complications can be resolved when treated promptly.2,17
33.3.5 Laser Complications
As well as with chemical peels, fractional laser treatments have their complications. And, as one can guess, darker skin types are more prone to pigmentary complications.
PIH is an acquired hypermelanosis that occurs after cutaneous inflammation or injury.14 It is the most common complication of laser treatments. People with darker skin are at greater risk of PIH (▶ Fig. 33.5). It presents as brown macules or patches with poorly defined borders. The severity of the pigmentary response is determined by the degree of inflammation.26 Transitory pattern hyperpigmentation can occur. It usually resolves in the first 3 months with topical treatments.10

Fig. 33.5 A 31-year-old Fitzpatrick skin type V patient with postinflammatory hyperpigmentation (PIH) and transitory pattern hyperpigmentation (notice the pigmented dots) treated with Lumenis AcuPulse (Palo Alto, California) carbon dioxide (CO2) fractional laser―deep fractional settings10 mJ, 10% density; superficial settings 90 mJ, 40% density.









