The East Asian Patient
East Asia is a subregion of Asia that is made up of about 12% of the Asian continent including more than 1.5 billion people and one fifth of the people in the world. They are represented by countries such as China, Japan, Korea, Mongolia, and possibly Vietnam. The characteristics of the East Asian patient from a dermatological standpoint can also include countries normally considered Southeast Asian such as Laos, Malaysia, Singapore, the Philippines, Thailand, and Cambodia. The variation of skin types within these countries is between Fitzpatrick skin types III to V.
In general in the United States, the Asian American population has been listed as 4.8%. Because of this, the frequency of treating the Asian client is relatively low. With the darker skin, the fear of hypopigmentation and hyperpigmentation often leads to a higher anxiety level for the U.S. clinician presented with this clientele base. Generally for hyperpigmentation, the risk increases as the color of the hair darkens and the skin lightens because the contrasting reaction of the skin tends to take on the color of the hair. Hypopigmentation risks increase as the skin darkens for similar reasons.
The Asian patient has a tendency to form pigmentary disorders versus wrinkling. Histologically the skin of the Asian clientele is characterized by larger melanocytes with increased production of melanin and melanosomes. Two groups found that Asians developed wrinkling one to two decades later than age-matched Caucasians.2,3 Melasma, ephelides, lentigines, and postinflammatory hyperpigmentation (PIH) are the most common conditions.
Because of recovery length and severity with traditional ablative techniques, multiple nonablative options have been popularized in the past several years. Lasers from 500 to 2,000 nm based on selective photothermolysis have avoided epidermal ablation while targeting pigment and blood vessels within the skin at progressively deeper layers. Radiofrequency and ultrasound have been introduced to nonspecifically treat the deeper tissue layers and create nonablative tightening. Although significant results can be achieved through these choices, the greater number of treatments needed, risk of hyperpigmentation, inferior results to ablative techniques, and the decreased effectiveness of treating both wrinkling and pigmentary issues with one modality maintain the utility of ablative methods in the recent trend of nonablative techniques. Ablative methods are indicated when patients want skin tightening for wrinkles, improvement of the uniformity of skin texture/tone, and reduction of pigmentary issues together in one treatment and can accept the more prolonged associated downtime.
31.3 Chemical Peels
Chemical peels can improve skin texture/tone and decrease the presence of active acne, acne scars, actinic keratosis, ephelides, fine and deep lines/wrinkles, melasma, and telangiectasias. Depending on the severity of each condition, one can devise a plan for each person.4 A full discussion of chemical peels is beyond the scope of this chapter. The author concentrates on the pertinent elements regarding chemical peels in the East Asian patient. A personal perspective is presented along with literature findings4 to help with the discussion.
In regard to ablative techniques, one can consider an aggressive skin care regimen of alpha hydroxyl acid fruit-acid peels, beta hydroxyl acid peels, Jessner’s peels, retinoic acid peels, TCA peels, laser resurfacing, phenol peels, and dermabrasion in that approximate order of increasing strength and depth of treatment. An aggressive skin care regimen starting with topical vitamin A and alpha hydroxy acid peels can be started and this can be done for a period of 4 to 8 weeks to prepare the skin for a deeper treatment. This is not mandatory but is thought to prepare the skin to heal faster (i.e., rapid re-epithelialization) and allow a more even peel when the deeper treatment is applied. It can also serve as an effective skin care maintenance program. What has been a standard for deeper treatments with moderate-depth chemical peels (i.e., Jessner’s and TCA 35% combination), laser resurfacing, phenol peels, and dermabrasion techniques is a 2- to 6- week pretreatment of the skin with Retin A, hydroquinone (or other bleaching agent), and hydrocortisone 1 to 2%. Both approaches aim to prepare the skin to be at even levels so that the penetration of the ablative method is uniform and to prevent PIH. Many studies are showing, however, that pretreatment may not benefit either the goal of more rapid epithelialization or the prevention of hyperpigmentation.5 Although open to debate, if a pretreatment regimen is utilized it should be stopped 6 to 7 days prior to the deeper treatment. For the East Asian patient, 4 to 6 weeks of pretreatment have been historically advised.
Alpha hydroxy acid peels are sometimes referred to as fruit-acid peels and include citric, glycolic, lactic, malic, and tartaric acids, and so forth. They are often used to subtly treat fine wrinkles, patchy dryness, and uneven pigmentation. Glycolic acids are perhaps the most common and range from 10 to 70% concentrations. Beta hydroxy acid peels such as salicylic acid appear to have more penetration into pores than the fruit-acid peels and can decrease sebum production; they are often formulated in skin products to treat acne. Jessner’s peels are formulated with 14% weight/volume of salicylic acid, resorcinol, and lactic acid in ethanol; they can be used to achieve a deeper peel than can be accomplished with fruit-acid and beta hydroxy acid peels. Glycolic peels with stronger preparations are preferred in an office setting at 30 to 70%, whereas the 10 to 30% preparations are used at home for continual maintenance. Jessner’s peels are used for deeper peels in the office and are employed to prepare the skin to allow a deeper peel using TCA at 30 to 35% strength immediately after. There are many options for chemical peeling. Having a simplified approach can markedly ease patient anxiety during the subsequent discussion of options with patients. In terms of chemical peeling, a complete approach to skin rejuvenation can be accomplished in the office with 30 to 70% glycolic peels, Jessner’s peels, and TCA peels (20, 35%).
Preoperatively, along with the pretreatment regimen, there are other precautions that should be followed. The patient should avoid blood thinners 2 weeks before and after ablative resurfacing (mostly moderate-depth peels or ablation techniques) that may have significant risk of causing bleeding. Medical risk assessments, a full history, and physical and other preoperative checks are done as with other measures commonly used for sedation. Specific contraindications are covered in other relevant chapters. Contraindications can include the following:
A current or history of skin cancer, especially malignant melanoma, or recurrent nonmelanoma skin cancer, or precancerous lesions such as multiple dysplastic nevi
Any active skin infection
Disease that may be stimulated by light at 560 to 1,200 nm, such as history of recurrent herpes simplex, systemic lupus erythematosus, or porphyria
Use of photosensitive medication and/or herbs such as isotretinoin, tetracycline, or St. John’s Wort that may cause sensitivity to 560- to 1,200-nm light exposure. Accutane (Roche, Basel, Switzerland) could warrant 1- to 2-years cessation before deep skin-ablation methods.
Immunosuppressive disease, including acquired immune deficiency syndrome (AIDS) and human immunodeficiency virus (HIV) infection, or use of immunosuppressive medications
Patient history of hormonal or endocrine disorders, such as polycystic ovary syndrome or diabetes, unless under control
History of bleeding coagulopathies, or use of anticoagulants
History of keloid or hypertrophic scarring
Very dry skin or conditions that would create healing issues in postprocedure phase
Exposure to sun or artificial tanning during the 3 to 4 weeks prior to treatment. Sunblock should be applied 2 weeks or more before any ablative procedure, using a product that is sensitive for the skin and contains titanium dioxide or zinc oxide.
Fitzpatrick skin types V and VI
Pregnancy and nursing
Ectropion (outward turning of the lower eyelid), excessively dry eyes, and previous lower blepharoplasty
Koebnerizing diseases (prior radiation therapy leading to a loss of adnexal structures), extensive fibrosis resulting from prior cosmetic treatments (e.g., dermabrasion, deep chemical peels, silicone injections)
Perhaps the most important part of this discussion is about the levels of penetration that are reached through chemical peels and how to discern each level (▶ Fig. 31.1). When doing the Monheit moderate-depth chemical peel this can be paramount to avoid scarring. With this peel, the Jessner’s peel is started and two to four passes are done to prepare for the TCA 30-35% peel, which is usually one to two passes but based on the parameters enumerated below:

Fig. 31.1 The first level of peeling is shown in pink and red. The upper eyelid is starting to show a slight frost with speckles of white turning into a sheet of translucent white, indicative of the peel penetrating the superficial papillary dermis just beyond the basement membrane.
The first level is when the skin turns pink/red. The depth has been thought to reach the basement membrane, with stimulation of the dermal blood vessels leading to the pink/red hue. This is mostly done with the Jessner’s peel. Peeling may or may not occur at 1 to 3 days.
The second level is when the skin starts to have specks of white, indicating the penetration into the papillary dermis and coagulation of dermal proteins just beyond the basement membrane. This can be achieved with the Jessner’s peel as well; however, it is better to stay at the first level with the Jessner’s peel prior to the 30-35% TCA. Peeling may or may not occur at 2 to 4 days.
As the specks turn into a layer of translucent white with a pink background, you have essentially penetrated the basement membrane and your peel has gone into the superficial papillary dermis. Because the anchoring fibrils are disrupted, the epidermis slides or moves more readily with manipulation. Peeling may or may not occur at 3 to 5 days.
When the pink background disappears and a solid layer of white frost is created, the next layer is reached with a moderate-to-deep peel. At this depth, the peel has reached the deeper layers of the papillary dermis because the vessels are constricted (leading to the disappearance of the pink/red) with further coagulation of the dermal proteins. The further coagulation also restricts the movement of the skin and the epidermal sliding disappears. This is the usual goal for the moderate-depth peel. Peeling may or may not occur at 4 to 7 days.
A gray background indicates a peel that has gone to the papillary reticular dermis junction depth and this is to be avoided because the risk for scarring increases at this level. Peeling may or may not occur at 6 to 10 days.
Chemical peeling is an “art” and requires experience. The levels described can rapidly progress from one level to the next and one can find oneself with a gray background quickly, especially with the stronger peels. Starting slowly and being conservative is important. The amount of peeling agent left in the cotton ball or other applicator used should be consistent. It has been advocated that 1 to 3 drops of solution should be left in the applicator for each application. This has been detailed as a process where the cotton ball is squeezed until only 1 to 3 drops are left, and this can be tested a few times before the actual application. The thickness of the peel solution on the skin is subjective as well and can require experience. These points help the clinician to advance through the different levels of peeling in a gradual and safe manner.
What can be most important of all is the postprocedure care after chemical peeling and other deep ablative resurfacing (▶ Fig. 31.2). For superficial peels that penetrate to the basement membrane, the use of Vaseline or Aquaphor (Beiersdorf Inc., Wilton, Connecticut) for 1 to 2 days is indicated (with petroleum jelly being preferred). At this depth, the watertight barrier that is created partially by urocanic acid in the middle portion of the epidermis, epidermal lipids, the cell-to-cell tight barrier created by desmosome connections, and the basement membrane itself are compromised―along with the skin barrier protective functions. Applying a proven nonreactive formulation such as Vaseline or other petroleum jelly can prevent unwanted skin reactions that can occur with application of other products with multiple ingredients. The key to faster healing is frequent cleaning. If this is done in the most effective way, peeling is much less of an event because the constant cleaning removes the desquamation. Use 1 teaspoon of over-the-counter white clear vinegar in a quart of distilled water along with a gentle cleanser such as Cetaphil (Galderma Laboratories, Fort Worth, Texas) or an equivalent. The areas treated are first washed with the gentle cleanser by patting and with as little rubbing or massaging as possible. These are then rinsed with the vinegar/water solution for 5 to 10 minutes. This is repeated as frequently as possible to keep the crusting to a minimum. The goal is pink, raw skin. Sometimes, immersing the entire treated area in a bowl of solution is necessary to moisten the crusts and allow them to slough off. The patient is directed to cleanse as frequently as every hour to achieve the goal. Frequent follow-up is mandatory. Pictures sent daily via text, e-mail, or provided in person can help tremendously. Importantly, the faster the healing the less likely scarring, hyperpigmentation, and hypopigmentation will occur in the East Asian clientele.

Fig. 31.2 Postprocedure day 3 after ablative resurfacing. This patient has too much crusting and needs to increase the frequency and length of cleaning to remove the crusts. These should be removed after each cleaning session and before Vaseline is applied. Also, the pink/red, raw area is the clinical level reached during the actual procedure.
The combined use of the moderate-depth chemical peel using Jessner’s peel and TCA 30 to 35% peel with dermasanding, can be very effective (▶ Fig. 31.3). As can be seen in the before and after images (▶ Fig. 31.331.3a, b), the deep wrinkles have been markedly reduced along with the finer wrinkles. The skin, although still erythematous at the 2-month mark, shows a much more uniform tone and is lighter in complexion. The texture is generally smoother in the after photo as well.
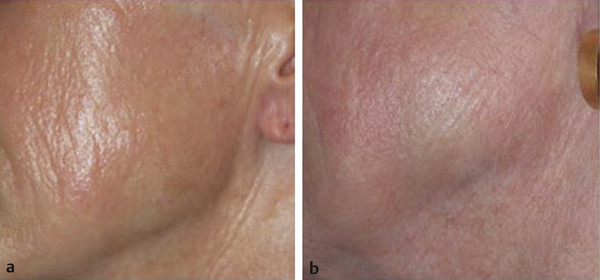
Fig. 31.3 Chemical peeling before (a) and after (b) the combined use of Jessner’s peel and trichloroacetic acid (TCA) 30 to 35% peel, and dermasanding for the lower cheek–jawline area 2 months postoperative.
31.4 Carbon Dioxide Laser Resurfacing
The CO2 laser was developed around the 1960s. It was the first laser to be utilized for skin, ophthalmological, and other surgical applications. Originally, the CO2 laser used continuous applied energy instead of pulses, which often led to adverse outcomes. In the 1980s, Dr. David Lawrence first used the CO2 laser for cutaneous resurfacing. With the continuous wave approach, extensive thermal injury that led to scarring and prolonged healing times occurred (measured in watts [W] = joules [J]/second [s]). Selective photothermolysis and the understanding of thermal relaxation times for different chromophores in the skin helped scientists develop pulsed lasers that were able to deliver high-energy pulses of short duration that limited the surrounding damage. The thermal relaxation time of skin 20 to 30 µm in thickness is about 1.0 ms, which is the time required for 50% of the heat to diffuse. The threshold for skin vaporization is about 5 J/cm2. With the fluence from 5 to 7 J/cm2, the CO2 laser can provide clean and efficient tissue ablation with much of the heat dissipated in the plume/smoke of the tissue (fluence is measured in joules/centimeters squared). This provides approximately 50 to 70 µm of ablation with about 20 µm of surrounding tissue injury.6 With the knowledge of average skin thicknesses,7 one can estimate the depth of resurfacing. This depends on the settings of the laser, with which one should be familiar. For example, at 100 mJ (millijoules), density scale 1, and 125-Hz frequency, the ablation depth is 70 µm and the thermal depth is 75 µm.
The preoperative and postoperative regimens for CO2 laser resurfacing are much the same as for chemical peels. The obvious difference is the mode by which the ablation is carried out. Traditional CO2 laser resurfacing is totally ablative, removing progressive amounts and layers of skin. The healing time can range from 5 to 10 days depending on the depth and the efficiency of the postoperative care.
Intraoperatively, because of the discomfort of CO2 laser resurfacing, a certain amount of sedation is needed. Oral sedation is quite commonly used. Intravenous sedation is perhaps more effective. Local and regional anesthesia is also a necessity to decrease the pain of CO2 laser resurfacing. With oral sedation, diazepam can be used at 5 to 40 mg to reach a level at which the patient is sedated but able to respond to vocal cues. The onset is slow, however, requiring 30 minutes to more than an hour to reach an effective state. Intravenous sedation is faster and potentially safer in some ways. A combination of propofol, ketamine, midazolam, fentanyl, and so forth can be used to reach a level of sedation where the patient is still able to respond to vocal and physical cues, while maintaining oxygen saturation above 95%. Eye shields are strongly recommended. Moistened, sterile towels around the field are necessary as well. Having a basin of saline as well as larger containers with water immediately around the field is useful for potential fires. Again, protective eye shields are needed. A complete CO2 laser resurfacing protocol for safety should be followed, as well as adherence to Accreditation Association for Ambulatory Health Care (AAAHC) standards or other appropriate credentialing institutions required by your state.
The laser settings used will require some familiarity with the particular CO2 laser. With the UltraPulse (Lumenis Ltd., Yokneam, Israel), a setting of 100 mJ, 150-Hz frequency, density scale 5, with cool scan is usually used with the first pass for traditional-type resurfacing. As seen in ▶ Fig. 31.4, traditional resurfacing entails the use of densities of 4 to 5, whereas fractional resurfacing utilizes densities of 1 to 3―which will be discussed. The second pass with traditional resurfacing is with 90 mJ, and a density of 4. The end results should show that the epidermis is ablated revealing the dermal layer. Viewing ▶ Fig. 31.2, the pink, raw area is the goal after the second pass and with removal using saline-soaked gauze. During the procedure what appears pink in ▶ Fig. 31.2 can be whiter in the operating room. Since skin thicknesses differ in individuals, one may find that for some patients this level is not reached after the second pass and in some this level may be too deep. In general these settings have been reliable. Of course, others vary these settings and still remain safe. Sasaki et al7 did an extensive study looking at the skin thickness of different areas of the body. The eyelids and neck are the thinnest areas and should require lower settings; 70 to 90 mJ are often used in these areas for the first pass and 60 to 80 mJ are used for the second pass with densities at 4 and 3, respectively. Some believe that the neck is better treated with fractional CO2 laser resurfacing, given the higher risk for complications in this part of the body. Nonfacial body parts tolerate CO2 laser resurfacing much the same as the neck and fractional resurfacing is often preferred as a safer option. The clinical indicators for CO2 laser resurfacing are:
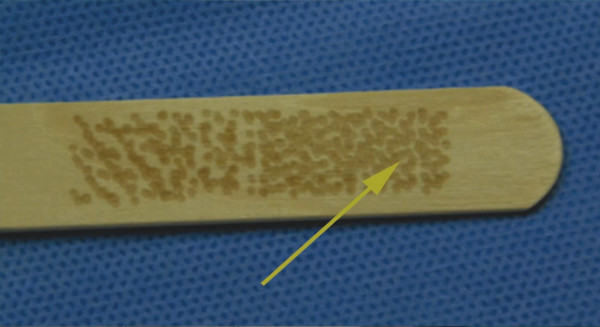
Fig. 31.4 The arrow points to density 5 for the UltraPulse (Lumenis Ltd., Yokneam, Israel) laser. Moving to the left-most spot size, the density becomes 2. This Active FX (Lumenis) handpiece uses a 1.3-mm spot size.









