Irritant Contact Dermatitis: Introduction
|
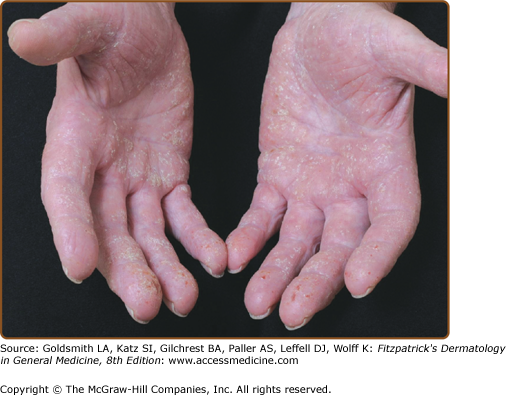
Dermatitis or eczema is a pattern of cutaneous inflammation that presents with erythema, vesiculation, and pruritus in its acute phase. Its chronic phase is characterized by dryness, scaling, and fissuring. Irritant contact dermatitis (ICD) is a cutaneous response to contact with an external chemical, physical, or biologic agent; endogenous factors such as skin barrier function and preexisting dermatitis also play a role (Figs. 48-1 and 48-2). The spectrum of presentation after contact with an irritant varies from overt dermatitis to subjective symptoms, contact urticaria, caustic and necrotic reactions as well as pigmentary changes and other dermatoses.
Epidemiology
In contrast to allergic contact dermatitis (ACD), no previous exposure to the causative agent is necessary in eliciting irritant reactions.1 ICD accounts for 80% of all cases of contact dermatitis,2,3 and is often occupation-related (occupational ICD is discussed in detail in Chapter 211). ICD caused by personal care products and cosmetics is also common; however, very few patients with these irritant reactions seek medical help because they manage by avoiding the offending agent.4
The incidence of ICD is difficult to determine because the accuracy of the epidemiologic data is limited. European cross-sectional studies for eczema due to all causes in the general population have shown point prevalence rates of 0.7%–40% and 1-year to lifetime prevalence rates of 7.2%–11.8%.5 Data from the U.S. Bureau of Labor Statistics show that of the 257,800 cases of nonfatal occupational illnesses reported in 2008 for all industries including state and local government and private industry, 18.9% (48,600 cases) were skin diseases, the second most frequent cause of all occupational illnesses reported.6 Based also on annual surveys of the Bureau of Labor Statistics incidence rates of occupational diseases in the American working population, contact dermatitis constitutes 90%–95% of all occupational skin diseases, and ICD constitutes about 80% of occupational contact dermatitis.7
Etiology and Pathogenesis
Four interrelated mechanisms have been associated with ICD: (1) removal of surface lipids and water-holding substances, (2) damage to cell membranes, (3) epidermal keratin denaturation,8–11 and (4) direct cytotoxic effects.11 There is a clearly demonstrated immunologic-like component to the irritant response,12 which is characterized by the release of proinflammatory mediators, particularly cytokines, from nonimmune cutaneous cells (keratinocytes) in response to chemical stimuli. This is a process that does not require previous sensitization.10 Disruption of the skin barrier leads to release of cytokines such as interleukin (IL) 1α, IL-1β, and tumor necrosis factor-α (TNF-α). A tenfold increase in the levels of TNF-α and IL-6, and a threefold increase in the levels of granulocyte-macrophage colony-stimulating factor and IL-2 have been observed in ICD. TNF-α is one of the key cytokines in irritant dermatitis, leading to the increased expression of major histocompatibility complex class II and intracellular adhesion molecule 1 on keratinocytes.10,13 The chemokine CCL21 that hones naive T-lymphocytes to the skin, has also been shown to be elevated in the skin during irritant reactions.14
Loss of function polymorphisms in the filaggrin gene, an important protein for skin barrier function, have been associated with an increased susceptibility to chronic ICD.15 At the same time, it is hypothesized that upregulation of ceramide 1 synthesis in the epidermis plays a major role in inducing the hardening phenomenon in cutaneous irritation.16
Influencing Factors
ICD is a multifactorial disease where both exogenous (irritant and environmental) and endogenous (host) factors play a role.
(See Table 48-1)
Type of irritant (pH, chemical activity) Cutaneous penetration of irritant Body temperature Mechanical factors (pressure, friction, abrasion) Environment (temperature, humidity) Other exposure factors: duration, prior or simultaneous exposures, direct versus airborne |
Other than with strong acids and alkalis, it has not been possible to predict the irritant potential of a chemical based on molecular structure. The irritant potential of compounded formulations may be more difficult to predict. Factors to be considered include: (1) chemical properties of the irritant: pH, physical state, concentration, molecule size, amount, polarization, ionization, vehicle, and solubility; (2) characteristics of exposure: amount, concentration, duration and type of contact, simultaneous exposure to other irritants, and interval after previous exposure;4,17 (3) environmental factors: body region and temperature; (4) mechanical factors such as pressure, friction, or abrasion;2 and (5) ultraviolet (UV) radiation. Low ambient humidity and cold temperature decrease the water content of the stratum corneum, making it more permeable to irritants. Larmi et al18 demonstrated that UVB radiation diminished the nonimmunological reactions caused by sodium lauryl sulfate (SLS)-induced irritation, probably as a result of anti-inflammatory effects.
When one or more irritants are combined or used simultaneously, a synergistic or antagonistic effect may occur as a consequence of specific cellular interactions between the compounds, or an alteration in the skin permeability by one or more of the compounds, that would not occur when an irritant is used alone.4,12 This is known as the crossover phenomenon. In a study by Wigger-Alberti et al,19 concurrent application of SLS and toluene twice daily for 30 minutes to the volar forearms of healthy volunteers induced significantly stronger irritant reactions than those caused by twice-daily application of each chemical alone. This study suggests a crossover phenomenon between the two compounds by which one irritant caused an increased susceptibility to the other. On the other hand, McFadden and colleagues20 demonstrated the neutralizing effect of benzalkonium chloride over the irritant effect of SLS.
(See Table 48-2)
Atopic dermatitis Skin site Skin permeability Individual (genetic) susceptibility Primary sensitive (hyperirritable) skin Lack of hardening Secondary hyperirritability of the skin (status eczematicus) |
It has been hypothesized that an individual’s ability to quench free radicals, to change the levels of antioxidant enzymes, and the ability to form protective heat shock proteins may all be under genetic control. These factors also determine the variability in responsiveness to irritants.21 Additionally, a genetic predisposition to irritant susceptibility may be specific for each irritant.22
The majority of clinical ICD affects the hands, and women account for a majority of these patients.23 Rather than a gender-related skin susceptibility, this demographic may reflect the facts that women have more extensive exposure to irritants and wet work and are more likely to seek treatment than men.4,17,24 On the other hand, there are anecdotal reports that suggest that the menstrual cycle can affect the sensitivity of women to primary irritants and can affect their dermatological response.25 No gender difference for ICD has been established experimentally.
Children younger than 8 years of age are more susceptible to percutaneous absorption of chemicals and to irritant reactions.4 Most studies show no compromise in skin barrier permeation with increasing age. Data on the influence of aging on experimental skin irritation are conflicting. Visible skin irritation (erythema) is decreased in older persons while invisible skin irritation (barrier damage) might be increased in the elderly.26
There are no studies that demonstrate a significant influence of skin types on the development of ICD.27–29 Because erythema is difficult to measure in dark skin, early studies30 using erythema as the only parameter to quantify irritation may have led to an erroneous interpretation that black skin is more resistant to irritation than white skin. It is also possible that variations among individuals rather than ethnicity play a role in the intensity of an irritant response.31
There are significant site differences in barrier function, making the skin of the face, neck, scrotum, and dorsal hands more susceptible to ICD. The palms and soles are comparatively more resistant.32
A history of atopy is a well-known risk factor for irritant hand dermatitis (see Chapter 14). A history of atopic dermatitis seems to be linked to an increased susceptibility to irritant dermatitis because of a lower threshold for skin irritation, impaired skin barrier function, and a slower healing process.33
In summary, the most important ICD risk factors are the inherent toxicity of the chemical for human skin and its penetration.34 The most important endogenous factors are an atopic diathesis and skin barrier function.26
Clinical Types of Irritant Contact Dermatitis
ICD has a spectrum of clinical features, which can be divided into several different categories, depending on the irritant and its exposure pattern.35 But these manifestations also depend on mechanical, thermal, climatic, and constitutional factors.17 The clinical types of ICD vary according to the irritant in question: ulceration (e.g., strong acids or alkalis), folliculitis (e.g., oils and greases), miliaria (e.g., aluminum chloride), hyperpigmentation (e.g., heavy metals), hypopigmentation (e.g., p-tert-butylphenol),10 alopecia (e.g., borax), urticaria (e.g., foods and plants), and granulomas (e.g., silica, talc)36 (see Table 211-1).
At least ten clinical types of ICD have been described. They are listed in Table 48-3 along with a number of clinical subtypes of acute and chronic ICD.
Irritation | Onset |
|---|---|
Irritant reaction | Acute, often multiple exposures |
Acute ICD | Acute, often single exposure |
Delayed acute ICD | Delayed (12–24 hours or longer) |
Chronic (cumulative) ICD | Slowly developing (weeks to years) |
Subjective (sensory) irritation | Acute |
Suberythematous (nonerythematous) irritation | Slowly developing |
Frictional dermatitis | Moderate–slow developing (weeks to months) |
Traumatic ICD | Slowly developing after preceding trauma |
Pustular or acneiform ICD | Moderately slowly developing (weeks to months) |
Asteatotic irritant eczema (exsiccation eczematid) | Moderate–slow developing |
Other clinical subtypes of acute and chronic ICD | |
Interdigital | Slowly developing (days to weeks) |
Frictional melanosis | Slowly developing (months to years) |
Diaper dermatitis | Acute or delayed |
Chemical burns | Acute or delayed |
Nonimmunologic contact urticaria | Acute |
Airborne | Acute |
Scalp irritation | Acute or delayed |
Nail irritation | Delayed to slow |
Tandema | Acute or delayed |
Photoirritationa | Acute |
Irritant reaction: An irritant reaction clinically presents as an acute monomorphic reaction that includes scaling, low-grade erythema, vesicles, or erosions and is usually localized on the dorsum of the hands and fingers. It is often seen in individuals who are exposed to wet work. An irritant reaction can resolve or progress to cumulative irritant dermatitis.10,12
Acute ICD: Acute ICD usually results from a single skin exposure to a strong irritant or caustic chemical, such as alkalis and acids, or as a result of a series of brief chemical or physical contacts. Most cases of acute irritant dermatitis are a consequence of accidents at work. A sensation of burning, itching, or stinging may occur immediately after the exposure to the irritant. The patient may present with erythema, edema, and vesiculation and with exudation, bullae formation, and tissue necrosis in more severe cases. The healing process of acute ICD occurs as a decrescendo phenomenon, where the irritant reaction quickly peaks and then immediately begins to heal upon removal of the irritant. Complete healing may take 4 weeks, with a good prognosis.4,12,17
Other forms of acute irritant reaction have been also described (see Table 48-3), such as airborne contact dermatitis resulting from exposure to irritant volatile substances and fumes or powders and dusts and particles (Table 48-4).4,17 Irritant cheilitis may result from lip licking or use of cosmetics and medication. Diaper dermatitis and perianal dermatitis may be the result of prolonged or too frequent contact with urine or fecal residues.17 Dermatitis resulting from sodium azide released by airbag deployment has also been described,37 causing an alkaline chemical burn; the accompanying talc powder may also contribute to the dermatitis.
Delayed acute irritancy: The delayed irritant reaction is acute but without visible signs of inflammation appearing until 8–24 hours or more after exposure. Otherwise, the clinical appearance and course are similar to those of an acute ICD.4,12 The delayed presentation may simulate that of an ACD, sometimes making differentiation of the two disorders difficult, even with patch testing. Substances causing delayed irritancy are listed in Table 48-5. Delayed acute irritancy in general has a good prognosis.10,12,17
Chronic cumulative ICD: This is the most frequent type of contact dermatitis encountered in clinical practice. Also called traumiterative ICD, cumulative ICD develops as a result of repeated insults to the skin, where the chemicals involved are often multiple and weak and would not in themselves be strong enough to cause irritant dermatitis.10,12,17 The most common marginal irritants include soap, detergents, surfactants, organic solvents, and oils,2

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree