Inverted L Osteotomy for Mandibular Surgery
Raymond J. Harshbarger
DEFINITION
Various procedures have been developed to alter the shape and position of the mandible, including the sagittal split osteotomy, vertical ramus osteotomy, and inverted L osteotomy (ILO).
The ILO allows separation of the proximal condylar bearing segment and the distal occlusal bearing mandibular segment, for advancement of the distal segment.
Improvements with distal segment advancement:
Enhancement of airway space at the tongue base, thus improving breathing functions
Treatment of class II dentofacial deformity, establishing abnormal bite, chewing, and speaking
ANATOMY
The mandible is a ring structure articulating with the skull base at the glenoid fossa.
In addition to bearing responsibility for the foundation of the lower third of the face, the mandible contains the lower dentition, and the inferior alveolar nerve transverses the marrow space through the ramus and body.
Pertinent features on the lateral (buccal) surface of the mandible include the anterior/posterior ramus, sigmoid notch, condylar process, and coronoid.
Medially, key landmarks include the sigmoid notch, lingua, mandibular foramen, and position/occlusal surface of molars.
The marginal mandibular nerve changes position depending on patient age: in neonates, the marginal mandibular nerve travels along mandibular border; with increasing age, the nerve migrates inferiorly. By skeletal maturity, the nerve is about two fingerbreadths below the mandibular border.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients who benefit from ILO are generally divided into two groups:
Neonates and children:
May present with airway obstruction, difficulty feeding, gastroesophageal reflux, and failure to thrive
Physical examination demonstrates micrognathia, glossoptosis, and possible cleft palate.
Skeletally mature patients:
May have had a history of obstructive sleep apnea, TMJ disorder (with pain), and chewing and speaking dysfunction
Physical examination demonstrates a sagittal deficiency of the lower third of the face with class II malocclusion.
IMAGING
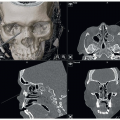
Computed tomography demonstrates sagittal deficiency of the mandible. Typically, other components exhibit normal morphology.
Operative airway evaluation (rigid and flexible exam) is done to assess glossoptosis, tongue-based airway obstruction, and prolapsed epiglottis. An anterior tongue pull and jaw thrust will improve the obstruction.
DIFFERENTIAL DIAGNOSIS
Pierre Robin sequence
Craniofacial microsomia
Treacher Collins
Micrognathia
Juvenile rheumatoid arthritis
SURGICAL MANAGEMENT
Candidates for ILO include patients with sagittal deficiency of the mandibular body, including neonates, children, and skeletally mature patients. Distraction may be performed in all three groups. Orthognathic surgery is indicated in skeletally mature patients; ILO may be chosen over a sagittal split osteotomy, or vertical ramus osteotomy, especially when dealing with patients who have asymmetric skeletal findings. With a single-step mandibular advancement, bone grafts are used to bridge the created gap.
Preoperative Planning
Neonates
Computed tomography
Operative airway (rigid/flexible) evaluation
Polysomnography
Possible virtual surgical planning with creation of operative cutting and positioning guides
Children and skeletally mature
All of the above
Placement of orthodontic appliances, with preparatory orthodontics
Positioning
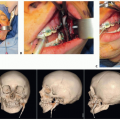
Neonates: Supine position, with head on a gel roll, a shoulder roll, neck in extension, and an oral ET tube that is microcuffed. ET tube should be taped to the upper lip, brought cephalically, and fixed at the hairline over egg crate foam with 2-0 silk. Eyes are protected with Tegaderm (FIG 1).
Children and skeletally mature patients: Nasal RAE tube sutured at the septum and at the hairline over egg crate foam with 2-0 silk. A shoulder roll should be placed, with eyes protected using Tegaderm. The patient’s head should be placed on a gel roll or foam.
Approach
The ILO technique may be approached from either an extraoral or intraoral incision or both. FIG 1 • Patient positioning (neonatal) for extraoral inverted L osteotomy.
TECHNIQUES
▪ Extraoral Inverted L Osteotomy
Exposure
This technique is commonly used for mandibular distraction osteogenesis.
Incision marking is designed to facilitate the osteotomy and protect the marginal mandibular nerve.
In neonates, the neck is placed in extension; palpate the mandibular angle, marking the incision one finger breadth below the angle. Starting posterior to anterior at the angle and maintaining one fingerbreadth below the mandibular border, the incision should be 2.5 cm in length. It may be helpful to dot the midline of the neck, to view the projected path of each incision, and to improve symmetry (TECH FIG 1A).
In children and skeletally mature patients, a similar approach is used; however, with increasing age, begin increasing the distance between the mandibular border and incision placement, migrating caudally to a position of two fingerbreadths below the border in adults.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree