16 Intralesional Injections
Indications
Indications for the use of intralesional steroid injections in dermatology include the following:
Equipment
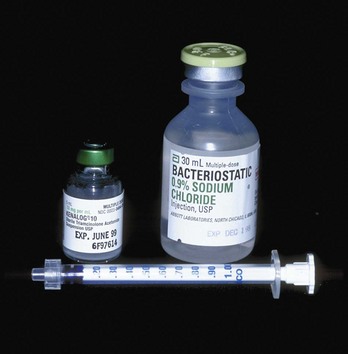
The equipment used for intralesional injections is listed here and shown in Figure 16-1:
Informed Consent
Patients should be informed of the risks of skin atrophy, incomplete resolution of the lesion, and hypopigmentation. Have the patient sign a consent form, especially if the lesion is on the face. Special care should be taken when treating lesions on the face in darkly pigmented individuals because hypopigmentation can be a particularly unacceptable side effect. As with all informed consents, the patient should be made aware of alternative therapies. Alternative therapies for keloids are listed in Table 16-1.
TABLE 16-1 Therapies for Keloids
| Topical | |
| Corticosteroids | |
| Retinoids | |
| Imiquimod | |
| Mederma | |
| Vitamin E | |
| Injectable | |
| Corticosteroids | |
| Interferons | |
| 5-Fluorouracil | |
| Verapamil | |
| Bleomycin | |
| Surgical | |
| Surgical debulking or excision | |
| Laser debulking or excision | |
| Radio-frequency electrosurgery planing | |
| Physical | |
| Laser therapy | |
| Radiation therapy | |
| Compression therapy | |
| Silicone sheeting | |
| Cryotherapy | |
| Fractional laser ablation |
Source: Adapted from Baldwin H. Keloid management (Chap 44). In: Robinson JK, et al., eds., Surgery of the Skin: Procedural Dermatology. Philadelphia: Elsevier; 2005.
Steroid Strength
Once the appropriate-strength steroid for the injection has been chosen, the standard-strength preparations may need to be diluted to produce the desired strength. Recommendations for steroid strength and needle size are listed in Table 16-2. Triamcinolone acetonide suspension is available in two strengths: 10 and 40 mg/mL. It is essential to dilute the steroid, especially for injections of cystic acne of the face. Dilution may be done for each patient just before giving the injection or may be done in a sterile vial of saline and saved for the injection of multiple patients over time. Unless giving intralesional injections frequently, it is probably better to perform the dilution for each patient. Diluted vials can lose their potency and have a higher theoretical risk of contamination.
TABLE 16-2 Recommended Steroid Strength and Needle Size for Intralesional Injections
Lesions | Triamcinolone (mg/mL)a | Needle size (gauge) |
|---|---|---|
| Acne cysts (face and neck) | 1–2 | 30 |
| Acne cysts (trunk) | 2–3.3 | 27–30 |
| Acne keloidalis nuchae | 5–10 | 25–27 |
| Alopecia areata | 5 for scalp and 3.3 for face | 27 |
| Discoid lupus | 2.5–5 | 27 |
| Granuloma annulare | 5 | 27 |
| Hidradenitis suppurativa | 3.3–5 | 27 |
| Hypertrophic scars | 10–20 | 25–27 |
| Keloids | 10–40 | 25–27 |
| Lichen simplex chronicus | 2.5–5 | 27 |
| Prurigo nodularis | 5 | 27 |
| Psoriasis | 2.5–5 | 27 |
| Sarcoidosis | 2.5 on face and 5 on body | 27–30 |
a For lesions on the face, always start with lower concentrations.
A 1-mL Luer-Lok or tuberculin syringe is useful for making a single dilution before injection. To create a 2 mg/mL concentration, draw 0.4 mL of sterile saline into a 1-mL syringe and add 0.1 mL of 10 mg/mL triamcinolone. Other dilutions are listed in Table 16-3. Turn the syringe upside down a number of times to mix the new suspension. It is recommended that the saline be drawn up first because it is more acceptable to get a little saline into the triamcinolone than vice versa. Recommended needle sizes by lesion are listed in Table 16-2.
TABLE 16-3 Common Triamcinolone Dilutions in a 1-mL Syringe
Concentration (mg/mL) | mL of Triamcinolone 10 mg/mL | mL of Sterile Saline for Injection |
|---|---|---|
| 1 | 0.1 | 0.8 |
| 2 | 0.1 | 0.4 |
| 2.5 | 0.2 | 0.6 |
| 3.3 | 0.2 | 0.4 |
| 5 | 0.3 | 0.3 |
Treating Specific Lesions
Acne Nodules and Cysts
Patients with tender large nodulocystic lesions can expect to get symptomatic relief within 24 hours of an intralesional injection. The lesion will flatten within 2 to 3 days with an effective injection.1 Although this should not be the primary treatment of acne, it can provide short-term relief while employing more long-term treatment regimens.
One small study evaluated the effectiveness of intralesional injections of steroids in the therapy of nodulocystic acne.1 They found that 0.63 mg/mL of triamcinolone was as effective as 2.5 mg/mL.1 Betamethasone injections were no better than saline controls.1 One review article states that concentrations of 3.3 and 5 mg/mL of triamcinolone are standard dilutions for intralesional acne injections.2
We recommend using 1 to 3.3 mg/mL of triamcinolone for nodulocystic acne depending on the location of the lesions and the experience of the clinician and patient. Triamcinolone can be injected with minimal pain using a 30-gauge needle on a 1-mL syringe at a 45- to 90-degree angle with the skin (Figure 16-3).

FIGURE 16-3 Nodulocystic acne being injected with dilute triamcinolone.
(Copyright Richard P. Usatine, MD.)
Acne Keloidalis Nuchae
Acne keloidalis (Figure 16-4) occurs on the posterior neck most commonly in men with highly pigmented skin. It is an inflammatory condition that is exacerbated by shaving the back of the neck. It has features of acne and folliculitis. Over time keloidal-type scars occur and can become very large. Treatment and prevention include not cutting the hair too short and using topical steroids and topical retinoids. Tender and painful keloidal nodules can be injected with triamcinolone for some relief. Concentrations of 5 to 10 mg/mL can be used. The heavier the fibrosis and scarring, the larger the needle needed to inject the lesion.
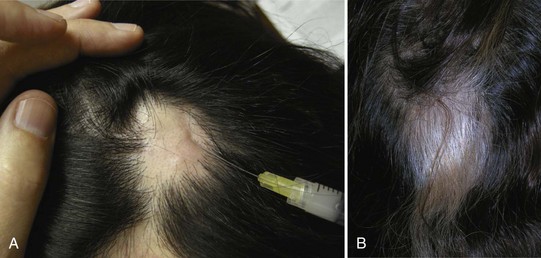
Alopecia Areata (Figure 16-5)
Although a recent Cochrane review on the treatment of alopecia areata (Figure 16-5) found no RCTs on the use of intralesional steroids (and many other treatments), they did acknowledge that this is a commonly used treatment for alopecia areata.3 Considering the possibility of spontaneous remission in the early stages of the disease, it is reasonable to reassure the patient and recommend tincture of time. However, many patients are seeking an active treatment. Intralesional steroid for alopecia areata is a well-accepted standard treatment and often gives patients hope that they will regain their hair. Recommended concentrations of triamcinolone range from 5 to 10 mg/mL for the scalp, but the higher concentrations often cause scalp atrophy. Therefore we recommend using 5 mg/mL of triamcinolone for the scalp. Alopecia areata can affect the eyebrows and the beard. For those regions it is safer to stick with a lower concentration of triamcinolone such as 3.3 mg/mL. A long 27-gauge needle (1.25 to 1.5 inches) will allow for treatment of larger areas with fewer injections per site.