■ When the sentinel node is mapped to above the inguinal ligament (typically with a flank primary melanoma), the sentinel node incision should ideally be obliquely or transversely oriented and at least 0.5 cm proximal to the groin crease (FIG 1B).
■ For planning the completion lymphadenectomy, the operative side and site should be identified with the agreement of the patient and/or the representative of the patient in the preoperative holding area.
■ Patients with a prior history of deep vein thrombosis (DVT) or known genetic predisposition to thrombosis are given a prophylactic dose of low-molecular-weight heparin preoperatively.
■ A first-generation cephalosporin such as cefazolin (or equivalent if allergic to cephalosporins or penicillin) are routinely given intravenously within 30–60 minutes of the creation of the skin incision.
Positioning
■ The patient is placed in the supine position on a standard operating table. A sequential compression device (SCD) (knee length ipsilateral and thigh length contralateral) should be placed for DVT prophylaxis prior to induction of anesthesia. General anesthesia is required using either a laryngeal mask or endotracheal tube for inguinofemoral lymphadenectomy, but endotracheal tube is preferred for ilioinguinal dissections. Long-acting paralytic agents at induction are often avoided to allow for motor nerve stimulation to be evident during the course of the procedure. A urinary catheter is inserted for ilioinguinal dissections but may potentially be omitted for inguinofemoral dissections at the discretion of the surgeon. The patient is placed in a slight frog-leg position with all pressure points padded. The operative field should be prepared from the abdominal wall at the level of the umbilicus to the level of the knee. A groin towel secured with a sterile adhesive drape can be used to cover and exclude the genitalia from the field.
TECHNIQUES
INGUINOFEMORAL (OR SUPERFICIAL) LYMPHADENECTOMY
Skin Incision and Raising of Flaps
■ As stated previously, a well-placed node biopsy incision, or avoiding the creation of a preexisting incision by percutaneous instead of open biopsy of palpable metastasis, is important to minimize the area of required skin flaps.
■ For a positive sentinel node where the sentinel node scar is below the inguinal crease, a curvilinear incision is made in a vertical orientation with an ellipse of skin to facilitate excision of the previous cavity of dissection (FIG 2A). For a positive sentinel node where the sentinel node scar is above the inguinal crease, a transversely or obliquely oriented incision is made to excise the previous cavity of dissection. A second counterincision can be made below the inguinal crease to reach the remaining femoral nodes (FIG 2B). In thin individuals, retraction can frequently allow for the extirpation of the femoral nodes distal to the inguinal crease without the need for the second incision.
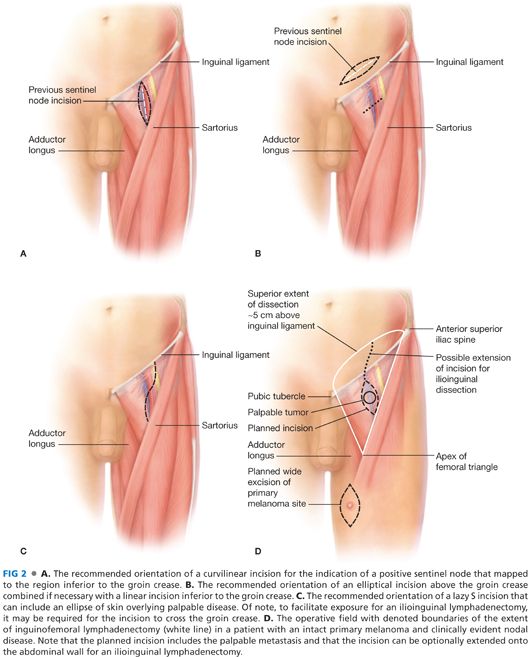
■ For palpable disease without a pre-existing biopsy scar, a skin incision is configured in a lazy “S” fashion (FIG 2C). If the tumor is close to the skin, an ellipse of skin overlying the palpable tumor should be included. The incision should also include any scar from prior node biopsy procedure if applicable. This incision can be extended in a cranial direction if needed for an ilioinguinal lymphadenectomy.
■ Skin flaps are raised in order to clear the anticipated boundaries of the dissection (below) without being so thin to cause postoperative skin necrosis. Limiting the extent of the flaps to the borders of the femoral triangle avoids an unnecessarily wide field of dissection and therefore may be associated with a reduction in morbidity.
■ The dissection is continued to the level of the muscular fascia with the following boundaries (FIG 2D):
■ Anterior superior iliac spine (ASIS) superolaterally
■ Pubic tubercle superomedially
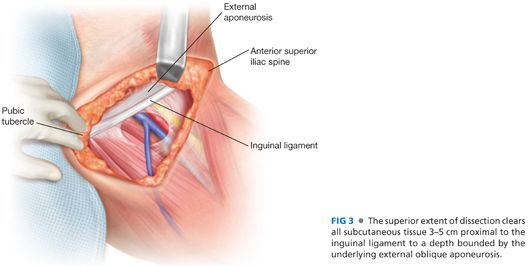
■ The superior extent of dissection should encompass the tissue from the ASIS to the pubic tubercle resulting in approximately 3–5-cm clearance above inguinal ligament while leaving external oblique fascia intact.
■ Sartorius muscle laterally, incising the fascia
■ Adductor longus medially, incising the fascia
■ Crossing of the sartorius and adductor longus distally (the so-called apex of the femoral triangle)
■ It should be noted that while there have been isolated reports suggesting that incising the fascia of the sartorius and adductor longus may increase lymphedema, this has not been established in large series and most surgeons incise the muscle fasciae as described earlier.
■ During the course of the dissection, tissue that potentially contains lymphatic vessels should be clipped, tied, or sealed with harmonic shears.3
■ A key point of the upper extent of the dissection on the abdominal wall is that the lymphadenectomy clears the subcutaneous and node-bearing tissue down to the external oblique fascia from the boundary of the ASIS to the pubic tubercle proximally and down to the inguinal ligament distally (FIG 3). The dissection can typically preserve the spermatic cord in males, but the round ligament can be divided, if necessary due to the presence of disease, in females.
Dissection of the Saphenous Vein Distally
■ The distal portion of the saphenous vein is encountered along the medial boundary of the dissection approximately 3–5 cm proximal to the apex of the femoral triangle. In most cases, the saphenous vein is tied off distally with 2-0 silk and divided. The saphenous vein can potentially be preserved in select cases where the procedure is performed for micrometastatic disease, when and if any existing seroma cavity and scar tissue is separate from the vein.1,4 Although saphenous vein preservation might theoretically reduce the likelihood of postoperative DVT and lymphedema, this maneuver has never been definitively shown to reduce postoperative complications in any prospective, randomized study. Therefore, saphenous preservation should only be considered in select cases performed for micrometastatic disease, where the vein is not involved with scar or seroma cavity, and the maneuver should never compromise the extent of dissection.
Dissection of the Femoral Vessels
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








