Infestations
Robert Stavert
Alix J. Charles
Sarah J. Harvey
Abel D. Jarell
PEDICULOSIS
I. BACKGROUND
Infestation with lice is known as pediculosis. There are two species of lice specific to the human host: Pthirus pubis (Fig. 23-1) and Pediculus humanus (Fig. 23-2). These wingless, six-legged insects are obligate parasites and are host specific for humans. The lice that inhabit the head or body are both types of P. humanus (P. humanus humanus and P. humanus capitis); only the body louse is capable of transmission of disease-endemic typhus (Rickettsia prowazekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis and Borrelia duttoni). Pediculus capitis is not known to be a disease vector. The head louse is transmitted through shared clothing and brushes; the body louse, by bedding or clothing; and the pubic louse, from person-to-person contact and not infrequently through clothing, bedding, or towels.
The adult body louse (Pediculosis humanis) is 2 to 4 mm long, has three pairs of legs with delicate hooks, and is gray-white in appearance. Body lice prefer to live in clothing, particularly seams, and move to the body to feed. Heavy infestation is common in crowded, unhygienic surroundings such as military personnel and refugees during wartime, prisons, chronic health-care institutions, and homelessness. Head lice (P. capitis) most commonly affect children, between the ages of 3 and 11. The incubation period from exposure to pruritus is approximately 30 days. The ova (nits), which are oval, 1 mm long and gray, and firmly attached to the hair, hatch in approximately 7 to 9 days and become mature in another week (Fig. 23-3). Ova are laid very close to the scalp and hatch before the hair grows more than 1/4”. If no nits are found within 1/2” of the scalp and no lice are seen, treatment is not necessary because nits more than 1/2” from the scalp are eggshells from a past infection. Head lice do not jump or fly from one person to another.
The crab or pubic louse (P. pubis), which usually inhabits the genital region, is short (1 to 2 mm) and broad, and the first pair of legs is shorter than the claw-like second and third pairs. Infestation may occur in other areas, including the moustache, beard, axillae, chest, scalp, and eyelashes. Adult lice can live off the host for up to 36 hours and viable eggs, for 10 days. The chance of acquiring pediculosis pubis from one sexual exposure with an infected person is approximately 95%. Transmission of crab lice can occur without body contact, especially in warmer environments.
II. CLINICAL PRESENTATION
Extreme pruritus is the primary characteristic of pediculosis. It takes 4 to 6 weeks for the pruritus to develop in a nonsensitized individual and only 24 to 48 hours with repeat exposures. Chronic infection may lead to lichenification and hyperpigmentation from repeated scratching. In some cases, patients may be totally asymptomatic. Sleeplessness
may be reported, because lice are more active during nocturnal hours. Nits may be found most easily on the hairs on the occiput and above the ears. It is often difficult to differentiate a viable from a nonviable nit. Pseudonits are desquamated epithelium encircling the hair but are more readily removed than true nits. Secondary impetigo and furunculosis with associated cervical lymphadenopathy may occur. In severe cases, fever and anemia may be found. Feeling “lousy” was a term developed to describe the symptoms of pediculosis.
may be reported, because lice are more active during nocturnal hours. Nits may be found most easily on the hairs on the occiput and above the ears. It is often difficult to differentiate a viable from a nonviable nit. Pseudonits are desquamated epithelium encircling the hair but are more readily removed than true nits. Secondary impetigo and furunculosis with associated cervical lymphadenopathy may occur. In severe cases, fever and anemia may be found. Feeling “lousy” was a term developed to describe the symptoms of pediculosis.
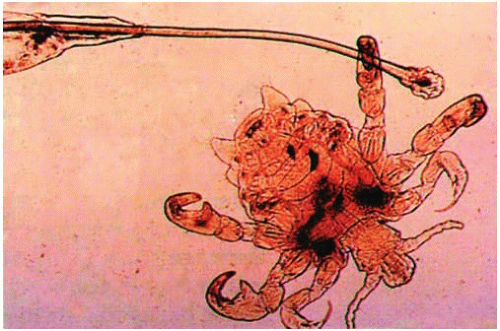 Figure 23-1. Pubic louse (crab). (Washington Winn Jr. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 5th ed. Philadelphia, PA: Lippincott-Raven; 1997.) |
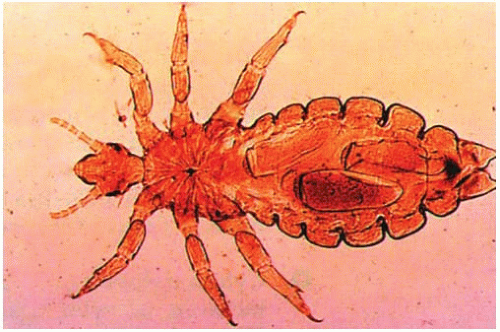 Figure 23-2. Body louse. (Washington Winn, Jr. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 5th ed. Philadelphia, PA: Lippincott-Raven; 1997.) |
In cases of body lice, scratch marks, eczematous changes, lichenification, urticaria, and persistent erythematous papules may be seen. Lesions are often
most noticeable on the back. The lice will be found in the seams of clothing and only rarely on the skin.
most noticeable on the back. The lice will be found in the seams of clothing and only rarely on the skin.
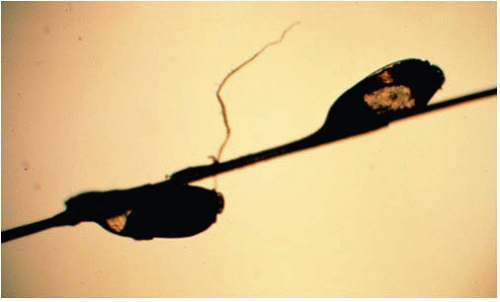 Figure 23-3. Nits. (From Goodheart HP. Goodheart’s Photoguide of Common Skin Disorders. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003.) |
Unexplained pubic pruritus is very often a manifestation of pediculosis. Pubic lice may infest pubic, perianal, and thigh hair with only a few or with uncountable numbers of nits (Fig. 23-4). The infection load may be particularly severe at the base of the eyelashes. The yellow-gray adults may be difficult to find and are usually located at the base of the hairs, resembling small freckles, scabs, or moles. Blue-black macules (macula cerulea) present in infested areas are associated with chronic infestations.
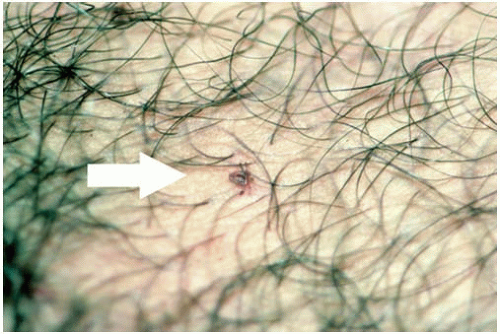 Figure 23-4. Pubic louse (see arrow). (From Goodheart HP. Goodheart’s Photoguide of Common Skin Disorders. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003.) |
III. WORKUP
For all forms of pediculosis, the presence of nits or adult lice is diagnostic (Fig. 23-5). Unexplained pruritus of the scalp should raise suspicion of head lice. Parents or school nurses can screen the posterior scalp with tongue blades or lice combs. It is necessary to be persistent in searching for nits. If suspicion is high, a therapeutic trial or reexamination in 2 to 3 days is indicated. In cases of body lice, close examination of clothing with attention to seams which come in contact with the neck, axillae, or waist may reveal lice or nits. In fastidious individuals, few adult lice and nits will be found, and a careful search—ideally employing a hand lens—should be made, with special attention to the genital area. In cases of public lice, the possibility of coexisting venereal diseases must be considered. Body and axillary hair as well as the eyelashes and beard should also be examined for nits; the scalp may rarely be involved.
IV. TREATMENT
First-line topical agents for pediculosis include permethrin, pyrethrins, and malathion. Lindane is considered a second-line agent due to neurotoxicity. Two additional topical agents recently approved by the Food and Drug Administration (FDA) are benzyl alcohol lotion 5% (Ulefsia) and Spinosad 0.9% creme rinse (Natroba), and recently a topical formulation of ivermectin lotion (Sklice) was also approved.
Increasing reports of resistance to permethrin, synthesized pyrethrins, malathion, and lindane have been noted. Besides resistance, other causes of treatment failure include improper technique, noncompliance, or reinfestation. In order to prevent reinfestation, treatment of close contacts is indicated. Most treatments for lice are pediculicidal and work by damaging the nervous
system of the louse. Pediculicides have varying ovicidal activity, and because eggs attached to hair shafts require 7 to 10 days to hatch, a second application is typically needed after this interval to ensure eradication.
system of the louse. Pediculicides have varying ovicidal activity, and because eggs attached to hair shafts require 7 to 10 days to hatch, a second application is typically needed after this interval to ensure eradication.
The eggs have a thick lipid layer that is difficult to penetrate; a 10-minute application is likely not sufficient to penetrate this membrane. A lice comb with an intertooth space less than the width of the nit is necessary between and after the treatment. Many parents prefer shampoo preparations but, overall, they are less effective than the cream rinse and lotion preparations. A great deal of counseling is required with any infestation as many patients feel socially stigmatized, confused, and distressed with the diagnosis.
All pediculicides kill lice, but the dead organisms do not fall off hairs or the body spontaneously. Most patients regard the continuing presence of dead organisms as evidence of continuing infestation, and it is necessary to clearly instruct them otherwise. The only certain way to remove dead nits is with a fine-toothed comb or forceps. Combs and brushes should be soaked in 2% Lysol or a pediculicidal shampoo for approximately 1 hour or heated in water to approximately 65°C (149°F) for 5 to 10 minutes.
For pediculosis corporis, the patient needs to only wash with soap and water and apply topical antipruritic lotions. If lice get on the body, pediculicides should be used. Lice in clothing may be killed by having the clothes washed and/or dried by machine (hot cycle in each); by boiling, followed by ironing the seams; by dry-cleaning; or by applying dry heat at 140°F (60°C) for 20 minutes.
For infestations of the eyelashes, if only a few lice are present, it may be possible to remove the lice and nits manually with the fingernails or with a nit comb. If further treatment is needed, ophthalmic grade petrolatum ointment applied to the eyelid margins two to four times daily for 10 days is considered the first-line treatment (Table 23-1).
1. Pyrethrins/Permethrin. The traditional treatment of choice for pediculosis capitis or pubis has been pyrethrins with piperonyl butoxide (RID, A-200 Pyrinate) or permethrin (Nix, Elimite); however, observation of increased resistance to these agents has led to more
frequent use of alternative agents. Pyrethrins, rapid-acting compounds, derived from chrysanthemum plants, are the leading over-the-counter louse remedy. Permethrin is a synthetic pyrethrin. These compounds interfere with neural transmission to the insects, leading to paralysis and death. For both head lice and pubic lice, the medication is applied to affected areas for 10 minutes and then rinsed off. It should not be used more than twice within a 24-hour period. RID and R&C are 0.33% pyrethrin shampoos; A-200 is a 0.33% Pyrinate shampoo and is less ovicidal than the pyrethrins. These products are unstable in heat and light and contraindicated in individuals with known allergy to ragweed, chrysanthemums, or other pyrethrin products, but these reactions are rare.
frequent use of alternative agents. Pyrethrins, rapid-acting compounds, derived from chrysanthemum plants, are the leading over-the-counter louse remedy. Permethrin is a synthetic pyrethrin. These compounds interfere with neural transmission to the insects, leading to paralysis and death. For both head lice and pubic lice, the medication is applied to affected areas for 10 minutes and then rinsed off. It should not be used more than twice within a 24-hour period. RID and R&C are 0.33% pyrethrin shampoos; A-200 is a 0.33% Pyrinate shampoo and is less ovicidal than the pyrethrins. These products are unstable in heat and light and contraindicated in individuals with known allergy to ragweed, chrysanthemums, or other pyrethrin products, but these reactions are rare.
TABLE 23-1 Primary Treatment Options for Pediculosis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
2. Malathion. Malathion lotion 0.5% is rapidly effective against head lice (5 minutes) and is ovicidal (95% killed). The FDA recommended application time is 8 to 12 hours. This organophosphate is one of the least toxic agents, as it is rapidly metabolized by mammalian carboxylesterase. This formulation is marketed in the United States under the name Ovide and is available by prescription; it was previously available as a 1% preparation. It binds slowly to hair but can maintain a residue for 2 to 6 weeks, which helps protect against reinfestation. This product is flammable until dry, and hair dryers and open flames should be avoided. Because of increased resistance to pyrethrin and permethrins, some authors have recommended that malathion be used as a first-line agent.
3. Benzyl Alcohol Lotion. Benzyl alcohol lotion 5% (Ulefsia) was approved by the FDA in 2009 for treatment of head lice and works via asphyxiating the louse. The lotion is applied to the scalp for 10 minutes and then rinsed out. Since it is not ovicidal, this must be repeated after 1 week. It can be used in children as young as 6 months of age and in pregnant women.
4. Spinosad. In 2011, spinosad 0.9% was approved by the FDA to treat head lice in patients 4 years old and older. Spinosad is derived from actinomycete, Saccharopolyspora spinosa, and although its precise mechanism of action is unknown, it appears to function by interfering with louse nicotinic acetylcholine receptors and γ-aminobutyric acid-gated chloride channels, leading to motor neuron excitation, muscular contraction, and eventually paralysis and death. The creme rinse is applied to dry hair and scalp for 10 minutes, followed by rinsing off. Nit combing is not required, and the process can be repeated if live lice are seen 7 days after treatment.
5. Dimethicone. Treatment with Dimethicone 4% lotion has been found to be effective in the treatment of head lice. Two treatments are administered 1 week apart and nit combing is performed in between and after treatments. Dimethicone is a silicone oil which is believed to work by coating the louse and interfering with water homeostasis.
6. Ivermectin. Recent studies have also demonstrated effectiveness with the use of oral ivermectin in the treatment of pediculosis capitis. In those studies, ivermectin was dosed at 400 µg/kg (28 mg for 70 kg patient) and given in two doses, 7 days apart. In 2012, the FDA approved Sklice, a formulation of 0.05% ivermectin lotion for the treatment of head lice.
Two recent randomized controlled trials demonstrated good results with a single application of the lotion applied thoroughly to dried hair and rinsed off after 10 minutes.
Two recent randomized controlled trials demonstrated good results with a single application of the lotion applied thoroughly to dried hair and rinsed off after 10 minutes.
7. Trimethoprim—Sulfamethoxazole. Trimethoprim—sulfamethoxazole (Bactrim, Septra) PO twice daily (or Bactrim DS once daily) for 3 days, repeated in 10 days, seems effective in the treatment of pediculosis capitis. However, because of the risks of severe drug reactions associated with trimethoprim—sulfamethoxazole, this treatment is generally reserved for severe or refractory cases.
8. Lindane. γ-Benzene hexachloride (Kwell), a pesticide also known as lindane, is an organochlorine with very slow onset of action and poor ovicidal activity; it takes over 3 hours to kill the lice during which increased lice crawling and twitching can cause increased pruritus for the patient. Lindane is available as a shampoo for the treatment of pediculosis capitis and/or pubis and in cream and lotion form for treating scabies and all forms of pediculosis. Up to 10% of the topically applied drug may be absorbed percutaneously, and therefore it should be applied to the skin after it has completely dried; alternative treatments should be considered in infants, young children, pregnant women, and individuals with significant alteration in epidermal barrier function (i.e., erythroderma). Due to concern for potential neurotoxicity, in 2003 the FDA recommended considering lindane as a second-line treatment for pediculosis, and in a separate update, the American Academy of Pediatrics no longer recommends lindane as a treatment option in children.
9. Alternative Regimens. Parents have undertaken alternative therapies because of fear of use of pesticides and frustration with treatment failures. Products with an oil base (Vaseline, olive oil, mayonnaise, and margarine) may smother the adult lice, but have no affect on the nits. Dippity-Do styling gel applied overnight under a shower cap is water soluble and is reported to smother lice. Vinegar or formic acid has been reported to remove the glue that holds the nit firmly to the hair shaft. Detanglers, plant oils, and cream rinses will also help lubricate the hair shaft and remove nits. Alcohol, kerosene, and paint thinners have also been used but carry extreme risks.
SCABIES
I. BACKGROUND
Scabies is caused by infestation with the mite Sarcoptes scabiei




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









