Key Words
breast reconstruction revision, implant exchange, capsulorrhaphy, capsulotomy, acellular dermal matrix, inframammary fold, capsular contracture
Introduction
Rates of breast reconstruction after mastectomy are increasing and have been paralleled by a rise in implant-based reconstruction. Single-stage immediate implant placement and two-stage tissue-expander techniques have demonstrated good safety profiles and patient satisfaction with outcomes. Advances in total submuscular and dual-plane reconstruction with acellular dermal matrix (ADM) or mesh as well as more recent prepectoral placement of implants have allowed for low complication rates with reproducible outcomes. However, despite optimization of these techniques, patients will often require revision of their reconstructions.
Over the long term, rates of revision for implant-based breast reconstruction can be significant, with risk of reoperation over a nine- to ten-year period ranging from 47.9% to 54.6% in large multicenter core silicone implant trials. While these include sequelae of acute infectious and ischemic complications, the majority of cases are secondary to more chronic processes. Tertiary revision rates are additionally high, with risk of reoperation near 50%. Single-stage reconstructions have decreased the number of reconstructive procedures after mastectomy. However, immediate implant reconstructions still require an average of 1.3 procedures per breast in our experience with revision rates of around 21% described in the literature.
Several techniques are available to the plastic surgeon to address secondary aesthetic and functional complications that necessitate revision of breast reconstruction. These techniques along with their respective indications for subacute and long-term revision of implant-based breast reconstruction will be reviewed in this chapter. Other common revision procedures such as fat grafting as well as correction of nipple–areola complex (NAC) malposition are discussed elsewhere in this textbook.
Indications and Contraindications
There is a broad spectrum of indications for several different secondary revision procedures in implant-based breast reconstruction ( Table 14.1 ). Adjustment of the inframammary fold (IMF) is indicated for correction of vertical implant malposition. Failure to secure the IMF to the chest wall if intentionally disrupted can result in inferior migration of the implant and a “bottoming out” phenomenon. Setting the fold too high, or inadequate dissection of the pocket inferiorly, can result in a high-riding implant. If the fold is intentionally lowered, but attachments of the native IMF to the pectoralis major are not completely obliterated, a second transverse band can become apparent, similar to a milder form of the double-bubble deformity in breast augmentation.
| Indication | Procedures |
|---|---|
| Implant malposition | IMF repositioning |
| Capsulorrhaphy | |
| Capsulotomy/capsulectomy | |
| ADM/mesh reinforcement | |
| Size asymmetry | Implant exchange |
| Fat grafting | |
| Capsular contracture | Capsulectomy |
| Implant exchange | |
| Pocket change to submuscular | |
| ADM | |
| Animation deformity | Pocket change to prepectoral |
| Rippling | Implant exchange |
| Pocket change to submuscular | |
| ADM/mesh support |
* Indications for nipple–areola complex repositioning and fat grafting described elsewhere in this textbook. IMF, inframammary fold; ADM, acellular dermal matrix.
Pocket adjustments include capsulorrhaphy to tighten various aspects of the capsule, capsulotomy or scoring of the capsule to allow for release in a particular direction, and even capsulectomy, or removal of portions of the capsule. Indications for capsular modifications include medial and lateral implant malposition in addition to vertical malposition causing asymmetry. Lateral migration of the implant may occur due to excess lateral dissection of the pocket as well as a size mismatch between the implant and the implant pocket. Similarly, medial migration due to overdissection over the sternum will result in symmastia and requires lateralization of the implant. Malposition of the NAC can also be corrected with capsular procedures if NAC displacement is secondary to an underlying capsular deformity.
Asymmetry in breast size can be addressed with implant exchange to either larger or smaller implants, in conjunction with capsular modifications as needed. Baker grade III/IV capsular contracture also necessitates removal of implants and replacement if desired. Reported rates of capsular contracture in primary reconstructions have traditionally been around 14%, though these have decreased significantly with utilization of acellular dermal matrix in certain series. Regardless, severe capsular contracture requires aggressive treatment with capsulectomy and implant exchange as well as possible pocket change and utilization of adjunctive biomaterials in appropriate scenarios. Other indications for change of the implant pocket include animation deformity with pocket change to a subcutaneous plane. On the other hand, complications more common in the subcutaneous plane, such as overlying breast rippling due to a lack of soft tissue coverage, can be treated with pocket change to the submuscular plane or change to a more cohesive implant.
Acellular dermal matrix (ADM) and mesh have recently emerged as a tool for treating several common complications after implant-based breast reconstruction. Acellular dermal matrix and/or mesh can be used for inferior support and definition of a new or pre-existing IMF when performing adjustment of the fold in cases of vertical malposition including high-riding and bottomed-out implants. ADM can also be utilized as an adjunct treatment for severe capsular contracture. Similar to the concept of submuscular pocket change in rippling, ADM can also serve to provide additional overlying soft tissue coverage in cases of rippling due to deficiencies in soft tissue.
Each planned revision procedure must be considered with regards to its efficacy in solving the presenting problem as well as in the overall clinical care of the patient. The integrity of the reconstruction and risk for compromising a reconstruction must be considered in each case. Any planned revisions during a patient’s oncologic treatment should be coordinated with the patient’s oncologic surgeon and oncologist. Lastly, patients must be counseled on realistic expectations and revisions should not be undertaken solely to please the patient or the surgeon if there are no defined and attainable goals.
Preoperative Evaluation
A thorough understanding of all the relevant factors of the preceding procedures is critical in preparing for a successful revision. If a patient has undergone nipple-sparing mastectomy, great care must be taken to prevent nipple–areola complex ischemia and maintain appropriate nipple position during revision surgery. The plane of prior implant placement is relevant in assessing implant malposition and the need for pocket exchange. Furthermore, prior expansion versus immediate implant placement can affect pliability of the skin envelope in accommodating changes in implant size.
The patient’s postoperative course after initial reconstruction is important to consider with regards to implications for secondary revisions. Postoperative hematoma has been associated with an increased risk of capsular contracture. Ischemic complications of mastectomy flaps can compromise the availability of skin and soft tissue if full-thickness necrosis requires excision. Adjuvant therapies such as chemotherapy can also influence complication rates. Patients that have undergone or are planned to receive radiation treatment must be approached with caution due to contracture of the skin envelope, fibrosis and impaired perfusion of the soft tissues.
Breast asymmetry should analyzed and addressed in a methodical fashion. Discrepancies in breast size are analyzed to determine whether apparent asymmetry is secondary to implant size, chest wall deformity, implant positioning, and/or the overlying soft tissue envelope. Next, implant malposition is similarly analyzed in a stepwise fashion, first in the vertical and then the horizontal vectors ( Table 14.2 ). In cases of inferior malposition, the relation of the implant to the IMF and distance of the inferior pole of the implant from the IMF is noted. In cases of superior malposition, it should be determined if the IMF was incorrectly set too high, if contracture of the soft tissue envelope and capsule is contributing, or if the high-riding implant is secondary to a combination of these factors.
| Skin | Quality and elasticity of skin envelope |
| Excess or deficient skin in relation to implant size | |
| Scars | |
| Radiation changes | |
| NAC position | |
| Soft tissue & capsule | Location of native IMF |
| Integrity of IMF | |
| Presence of remnant native IMF if fold relocated | |
| Quality of capsule & presence of contracture | |
| Medial and lateral extents of implant pocket | |
| Implant | Implant size |
| Anatomic versus round implant | |
| Plane of implant placement | |
| Use of acellular dermal matrix or mesh |
Malposition in the horizontal vector is analyzed with consideration of either over- or under-dissection of the implant pocket, as well as the congruity of the pocket with implant size and the overlying skin envelope. Medial overdissection, especially with dissection beyond the borders of the breast and over the sternum during mastectomy, can result in symmastia. Lateralization of the implant can also occur with overdissection, particularly with a discrepancy between a larger soft tissue envelope and the implant, when the implant can “fall” laterally. The appropriate pocket adjustments should be planned in concert with evaluation of the skin envelope to determine ease of repositioning and natural redraping of the skin.
When assessing implant malposition and planning corrective procedures, it is critical to take into account the position of the nipple–areola complex. Standard measurements including nipple to sternal notch distance and nipple to inframammary fold distance should be taken again. It must be determined if manipulation of the underlying implant and capsule will affect nipple position favorably or unfavorably. In these cases, additional manipulation of the nipple with mastopexy or directional techniques may be required, and must be planned in advance to avoid nipple malposition after revision procedures.
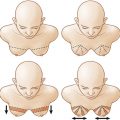
Capsular contracture should be graded according to severity and also evaluated with regards to the particular cosmetic deformation of the breast in relation to the natural anatomic breast. Rippling should be analyzed with regards to the size of the implant placed, the implant pocket and the quality of the overlying skin. In patients presenting with animation deformity of the breast, the severity of the deformity should be assessed, particularly with regards to its impact on the patient’s lifestyle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree