Implant-Based Reconstruction
James C. Yuen
After Standard and Modified Radical Mastectomy
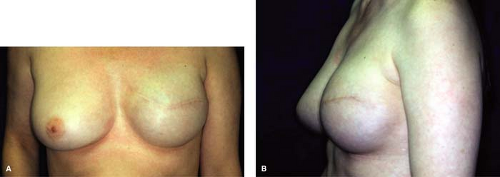
Implant-based breast reconstruction is currently the most common method for breast reconstruction. Implantation of a breast implant under the available soft-tissue is technically the simplest method. However, in most cases of standard mastectomy, this is not appropriate if local soft-tissue coverage is inadequate to allow placement of a permanent implant large enough to match the size of the contralateral breast. With placement of a tissue expander (Fig. 26.1), the soft-tissue envelope can be expanded until the desired volume is reached to match the opposite breast, or in bilateral cases, until the volume is reached to match the patient’s desired size. At a second procedure, the expander is exchanged for a permanent implant, saline or gel (currently available cohesive gel implant).
The advantages of implant-based breast reconstruction, especially with a single-stage implant insertion, are obvious. The surgery is localized to the same area, thus avoiding major surgical trauma, complications, and scars to other areas. The surgery does not eliminate the chance for autologous reconstruction if deemed necessary in the future. In a single-stage reconstruction, the procedure and process is relatively simple and completed in a single step, not including any need for nipple reconstruction. In the case of tissue expansion, the procedure is also relatively simple compared with the complexity of autologous reconstruction using pedicled or microvascular flaps. However, in addition to the need for a second operation, there is a major commitment for multiple office visits and a long delay of 3 to 6 months between the two operations. On the other hand, for bilateral cases, the patients can choose to reconstruct neo breasts that are larger than their preexisting breasts. These patients also can decide, to a certain extent, on their final breast size. Therefore, they gain the advantage of a sense of control when their femininity and normal health have been threatened by cancer.
Implant-based reconstruction obviously is much less invasive compared with autologous reconstruction; however, a host of potential immediate and delayed complications are present. In ipsilateral cases, the natural breast will descend with age while the reconstructed
side remains resistant to gravitational ptosis. In addition, it is generally more difficult to achieve a natural result compared with autologous tissue. After simple mastectomy in a patient with a remaining large breast, the expanded soft tissue may have difficulty producing a well-defined inframammary crease or significant ptosis. Despite these advantages, many patients still choose to undergo implant-based reconstruction for various reasons. This decision may be influenced by surgeon’s choice. The patient may wish to avoid major flap reconstruction for concerns of associated complications and longer recovery time. She may not have enough donor tissue, which is more commonly true in bilateral cases.
side remains resistant to gravitational ptosis. In addition, it is generally more difficult to achieve a natural result compared with autologous tissue. After simple mastectomy in a patient with a remaining large breast, the expanded soft tissue may have difficulty producing a well-defined inframammary crease or significant ptosis. Despite these advantages, many patients still choose to undergo implant-based reconstruction for various reasons. This decision may be influenced by surgeon’s choice. The patient may wish to avoid major flap reconstruction for concerns of associated complications and longer recovery time. She may not have enough donor tissue, which is more commonly true in bilateral cases.
 Figure 26.1 Representative samples of tissue expanders. This set is from Mentor: low-height, medium height, and tall height. |
In the case of the standard mastectomy, especially modified radical mastectomy, insertion of a tissue expander is routinely needed to recruit additional soft tissue by expansion, unless that patient’s contralateral breast in relatively small and there is not significant ptosis or atrophy. Expansion is normally performed 2 to 4 weeks after expander insertion and continued serially 1 to 2 weeks apart until desired size, at which point overexpansion is performed up to 20% extra. After an additional waiting period of at least 2 months, the expander is then exchanged for a permanent breast implant (Fig. 26.2). For immediate reconstruction, traditionally, the tissue expander is inserted with elevation of the pectoralis major and origins of the serratus anterior muscles in order to provide complete or near coverage of the prosthetic device. Muscle coverage helps protect the tissue expander under the thin mastectomy skin flap and prevent implant extrusion or exposure in the event of mastectomy skin necrosis or ischemic suture line dehiscence. Muscle turnover flaps and abdominal fasciocutaneous flap advancement have been described for implant coverage and enhanced development of the inferior pole. Single-stage
reconstruction with this modification has been described. The use of the latissimus flap with an implant is not included in this discussion, since this is considered a hybrid technique between autologous and implant-based reconstruction.
reconstruction with this modification has been described. The use of the latissimus flap with an implant is not included in this discussion, since this is considered a hybrid technique between autologous and implant-based reconstruction.
For two-stage reconstruction, because of the difficulty in expanding the inferior pole with complete muscle coverage, the technique was modified later to a dual-plane coverage in which only the pectoralis major muscle was raised to cover the upper aspect of the expander. Subpectoral positioning, and not complete muscle coverage, allowed for quicker and less painful surgery and gave rise to better inframammary fold definition. However, the limitations of the dual-plane positioning include less secure coverage of the implant’s inferior pole by the mastectomy skin flap. There is also less control over the position of the inframammary fold and possible superior retraction of the pectoralis major muscle postoperatively.
Use of Human Acellular Dermal Matrix
Over the past decade, simultaneously in a multitude of centers, the use of human acellular dermal matrix (HADM) in implant reconstruction emerged seemingly as a revolutionary promising augmentation in nonautologous breast reconstruction. This matrix is used to cover the lower and lower lateral part of the breast implant or tissue expander, while the pectoralis covers the respective upper portion. Several products of human acellular dermal tissue matrix are available: Alloderm (LifeCell Corp., Branching, NJ); AlloMax (CR Bard/Davol Inc., Cranston, RI); DermaMatrix (Synthes Inc., West Chester, PA); FlexHD (Musculoskeletal Transplant Foundation/Ethicon Inc., Somerville, NJ); and NeoForm (Mentor Corp., Santa Barbara, CA). These products are biologically prepared human dermis in which components causing rejection are removed and viral, bacterial, and fungal organisms are tested and removed. Alloderm was the first HADM used, which has been shown to revascularize rapidly with high retention rates. The HADM suspends and stabilizes the implant, while allowing high-volume fill within the implant. The tissue expander is no longer restricted by the tightness of complete muscle coverage. Since the pectoralis major is released along the inframammary crease and there is preservation of natural skin envelope with skin-sparing mastectomy (SSM) or total skin sparing mastectomy (TSSM, also referred to as nipple-sparing mastectomy or NSM), there is greater inferior pole and inframammary crease definition, which is usually difficult to achieve in traditional tissue expansion reconstruction following conventional mastectomy. The HADM provides some support between the implant and the mastectomy skin flap. In the case of SSM or TSSM, because of extra surface area of preserved skin compared with standard mastectomy, there is an associated higher rate of ischemic changes and skin necrosis. When not accompanied by secondary infection, the HADM provides coverage of the underlying prosthetic device, thus increasing the chance of implant retention. The advantages of the acellular dermal allograft are the following:
Creates a large pocket, confluent with the pectoralis major muscle to accommodate a full permanent implant or a substantially inflated tissue expander
Allows definition of inframammary and lateral mammary fold
Provides suspensory support of the implant at the lower pole
Establishes a protective interface between the prosthetic device and the mastectomy skin flap
Contributes to thickness of soft tissue over the prosthetic device
Minimizes or even obviates the need for serial expansion
Decreases periprosthetic changes, such as soft-tissue atrophy and chest-wall deformity
By attachment to the lower cut edge of the muscle, it prevents cephalad displacement of pectoralis major muscle
In summary, implant-based reconstruction is indicated for the patient who does not wish to undergo lengthy and complicated autologous reconstruction, who does not wish to take the risks of donor site morbidity, and who will not tolerate prolonged recovery time. However, for implant-based reconstruction to be indicated, the patient has to accept the host of potential complications associated with implantation and she
has to accept the staged procedures. In ipsilateral cases, implant reconstruction is indicated only if the patient accepts the potential inherent asymmetry and the need for a contralateral procedure, such as mastopexy or reduction mammoplasty. If the patient cannot accept the implant-related complications and the limitations of asymmetry in ipsilateral cases, or if she will not accept a contralateral procedure to improve symmetry, then implant-based reconstruction is relatively contraindicated, especially if the patient is a candidate for autologous reconstruction. In bilateral or even ipsilateral mastectomy, if the patient does not possess large enough volume of donor tissue for the breast size desired, then implant-based reconstruction is also indicated.
has to accept the staged procedures. In ipsilateral cases, implant reconstruction is indicated only if the patient accepts the potential inherent asymmetry and the need for a contralateral procedure, such as mastopexy or reduction mammoplasty. If the patient cannot accept the implant-related complications and the limitations of asymmetry in ipsilateral cases, or if she will not accept a contralateral procedure to improve symmetry, then implant-based reconstruction is relatively contraindicated, especially if the patient is a candidate for autologous reconstruction. In bilateral or even ipsilateral mastectomy, if the patient does not possess large enough volume of donor tissue for the breast size desired, then implant-based reconstruction is also indicated.
Single-Stage Versus Two-Stage with Tissue Expansion
Indications for single-stage versus tissue expander reconstruction depend on a multitude of variables. With the one-stage procedure in ipsilateral cases of standard mastectomy, the contralateral breast has to be small and cannot exhibit significant ptosis. In bilateral cases of standard mastectomy, if the patient desires small neo breasts, then single-stage reconstruction may be indicated. In moderate-sized breasts, traditional reconstruction using tissue expander with complete muscle coverage or dual-plane positioning would be indicated. With the utilization of HADM, single-stage reconstruction with permanent breast implant insertion has found wider applications, even in the presence of large and ptotic breasts.
After Skin-Sparing and Total Skin-Sparing Mastectomy
Especially, in the case of skin-sparing and nipple-sparing mastectomy, single-stage reconstruction with a permanent breast implant is a viable option. However, if larger breasts are desired, insertion of tissue expanders with HADM would still be indicated. If the patient has large breasts, for example “D” cup, and wishes to maintain a large size, tissue expander reconstruction would afford more control in the final breast size in the patient who does not wish to downsize. Keep in mind that for the patient with massively large breasts (above “D” cup), a skin reduction procedure would likely be indicated. Nipple-sparing (or total skin-sparing mastectomy) would be relatively contraindicated in face of mammary gigantism because the excessively redundant mastectomy skin, void of perforator perfusion from the breast, would be destined for major skin ischemia and necrosis. In addition, the volume of mastectomy skin flap would supersede the sizes of available tissue expanders, leading to unacceptable overhang and wrinkling of skin.
When skin-sparing or nipple-sparing mastectomy is performed, especially in moderate size or large-breasted patients there is a need to fill this empty space beneath the preserved skin flap. Insertion of a large-volume prosthetic device is needed to minimize wrinkling of the overlying skin. The use of HADM is indicated for coverage and stabilization of this large-volume prosthetic device. Alternatively, partial muscle coverage by the pectoralis major only or the addition of a turnover muscle flap are also options in place of HADM. Partial muscle coverage does have its limitations as described earlier, especially in immediate reconstruction where the mastectomy skin flap has inherent ischemia. Muscle turnover flaps require major dissection below the inframammary, which, in skin-sparing or nipple-sparing mastectomy, can render more ischemia to the mastectomy skin flap.
Contraindications for Implant-Based Reconstruction
A definite contraindication for implant reconstruction, as in any type of reconstruction, is advanced local disease and the presence of metastatic disease. Relative contraindications include a history of radiation with this becoming a definite contraindication when there is associated significantly adverse skin damage. Preoperatively, anticipated radiation therapy may be viewed as a relative contraindication for implant-based reconstruction. However, some centers advocate initiation of the required radiation therapy after completion of implant-based reconstruction.
The most important part of preoperative planning is to decide the operation of choice for the patient. First, the surgeon needs to ascertain whether the patient has chosen immediate or delayed reconstruction. The type of mastectomy chosen by the surgical oncologist has to be determined:
Modified radical mastectomy
Standard mastectomy (conventional mastectomy)
Skin-sparing mastectomy
Total skin-sparing mastectomy (also known as nipple-sparing mastectomy).
If the patient is not highly motivated and undecided with regard to reconstruction, then delayed reconstruction is recommended as a possibility. If the patient is undergoing a nipple-sparing mastectomy with moderate-sized or large breasts, then immediate reconstruction is more favorable to avoid contour irregularities from skin contracture with delayed reconstruction. If the patient is capable of tolerating implant reconstruction from the risk factor standpoint, the surgeon has to decide whether she can emotionally accept the staged procedures, including a delay of 4 to 6 months, or more, between the two operations from tissue expander insertion to exchange.
The patient must be informed of the relatively high rate of potential complications: bleeding, seroma, infection, dehiscence, skin necrosis, implant exposure, explantation, deflation or leak of the implant, migration of implant, capsular contracture, contour irregularities, asymmetry, and pain. The patient needs to be informed that body’s response to implantation is quite variable from person to person. While one person may suffer very little pain with the tissue expander in place, another person may have significant discomfort or pain. The process of tissue expansion can be quite uncomfortable for some but less for others. While most patients would accept the prosthetic device without significant contracture, a small subset of the population may develop significant capsular contracture. In the event the patient requires postoperative radiation, the potential untoward effects of radiation on the reconstructed breast needs to be discussed with the patient ahead of time.
If the patient undergoes a standard mastectomy, then there is a higher chance that a tissue expander would provide a better result. If the mastectomy is skin-sparing or nipple-sparing, then there is relatively higher change that a single-stage reconstruction with a breast implant would be favorable. The surgeon has to ascertain whether the patient would like to have reconstructed a slightly smaller breast size or to maintain her current breast size. The patient may choose to have smaller or even larger breast size. The surgeon may favor selection of tissue expansion for the individual who adamantly desires to maintain the same or larger breast size.
The surgeon has to ascertain the patient’s view of quality of life with or without reconstruction and the patient’s tolerance to complications. If the patient feels that having breast reconstruction is not a high priority, then relative to her intolerance to potential complications, reconstruction is not recommended.
Once the decision is made to proceed, the size and type of the implant or tissue expander is chosen. This is determined by measuring the width and height of the breast mound. The goal is to maximize the width of the prosthetic device, whether it would be a permanent breast implant or a tissue expander. The author uses the Mentor textured (Siltex®) Contour Profile®, integrated-valve expanders (Mentor Corporation, Santa Barbara, CA). This is an anatomically shaped expander. The maximum width of prosthesis aids in defining the mammary fold laterally and the cleavage medially. For ipsilateral cases, the base diameter of the contralateral breast is the critical measurement. Other factors to consider are the height and projection of the breast. The majority of patients are amenable to the medium height expander, style 6200. For the obese patient with low chest height the low-height expander, style 6100, is used. In the thin, tall patient with firm breast without much ptosis the tall-height expander is chosen, that is, style 6300.
A multitude of expander products can be used, depending on surgeon’s preference from previous experience. Inamed tissue expanders and permanent breast implants (Allergan, Santa Barbara, CA) have comparable anatomically shaped tissue expanders and implants (BioDIMENSIONAL® System). Other available brands include PMT (Permark Corporation, Chanhassen, MN) and SSP (Specialty Surgical Products, Inc., Victor, MN). For completeness, it should be noted that an adjustable permanent implant with a remote port can also be used for implant reconstruction, especially, if a high-volume permanent implant cannot be employed at the time of the mastectomy.
Surgical Prep and Positioning
It is crucial to reprep and redrape the patient to minimize contamination from the mastectomy surgical field. The old draping from the mastectomy is taken down without disturbing the surgical wound. The patient’s arms are positioned on arm boards and secured with slight flexion at the elbow. The operating table is checked to make sure that the back can be elevated to a sitting position during the surgery. Fresh prepping and draping are then performed, and the use of a new set of instruments is implemented.
Immediate Reconstruction
Inspection and Hemostasis
The skin is evaluated for its circulatory status. Any areas of obvious loss of perfusion within the mastectomy skin flap would need to be resected, which can change the plan for a single-stage implant reconstruction. In rare cases, in nipple-sparing or skin-sparing mastectomy, if significant portion of the mastectomy skin flap is compromised, initial plan for a single-stage implant insertion would need to be converted to a two-stage reconstruction with tissue expander. After copious irrigation, meticulous hemostasis utilizing electrocautery and bipolar cautery is performed.
Dissection of the Prosthesis Pocket
Generally, the mastectomy incision is not enlarged to complete the reconstruction. In the case of nipple-sparing mastectomy, this incision can be quite small and can be
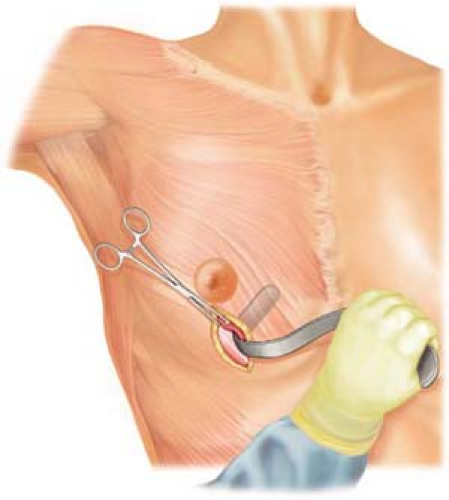
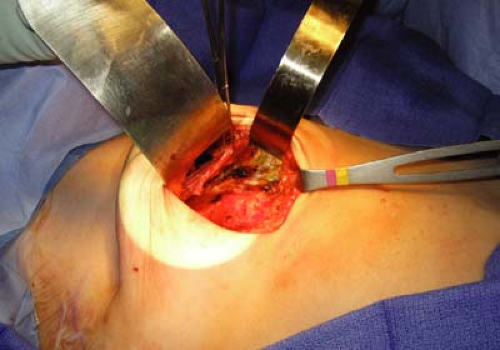
located in a number of possible locations depending on the oncological surgeon and previous biopsy incisions. The preferred mastectomy incision for nipple-sparing mastectomy at our center is a vertical incision centered on the breast meridian (6 O’clock) between the areola and the inframammary crease (Fig. 26.3). Through this incision, the lateral border of the pectoralis major muscle is controlled by an Allis clamp and dissection is performed using electrocautery (Figs. 26.4 and 26.5). In combination with digital blunt dissection, a plane is established beneath the pectoralis major muscle proper (Fig. 26.6). The pectoralis major is separated from the pectoralis minor muscle. The origin of the pectoralis major is separated off the entire width of the inframammary
crease and partially up along the border of the sternum (Fig. 26.7). Depending on patient’s existing cleavage, the more medial the breast mount desired, the more releasing is required of the pectoralis major origin along the sternum, even up as high as the second intercostals space. Attention is paid to avoid vigorous dissection here with the electrocautery to prevent creating a button hole of the skin or creating a plane too close to the opposite side, which would lead to symmastia. Depending on the extent of space needed, some of the most medial pectoralis major muscle fibers along the sternum may be maintained along its line of release. Hemoclips are required as necessary for parasternal perforators, which can be clipped and divided with impunity if they are no longer contributing to the mastectomy skin flap circulation.
located in a number of possible locations depending on the oncological surgeon and previous biopsy incisions. The preferred mastectomy incision for nipple-sparing mastectomy at our center is a vertical incision centered on the breast meridian (6 O’clock) between the areola and the inframammary crease (Fig. 26.3). Through this incision, the lateral border of the pectoralis major muscle is controlled by an Allis clamp and dissection is performed using electrocautery (Figs. 26.4 and 26.5). In combination with digital blunt dissection, a plane is established beneath the pectoralis major muscle proper (Fig. 26.6). The pectoralis major is separated from the pectoralis minor muscle. The origin of the pectoralis major is separated off the entire width of the inframammary
crease and partially up along the border of the sternum (Fig. 26.7). Depending on patient’s existing cleavage, the more medial the breast mount desired, the more releasing is required of the pectoralis major origin along the sternum, even up as high as the second intercostals space. Attention is paid to avoid vigorous dissection here with the electrocautery to prevent creating a button hole of the skin or creating a plane too close to the opposite side, which would lead to symmastia. Depending on the extent of space needed, some of the most medial pectoralis major muscle fibers along the sternum may be maintained along its line of release. Hemoclips are required as necessary for parasternal perforators, which can be clipped and divided with impunity if they are no longer contributing to the mastectomy skin flap circulation.
 Figure 26.3 Bilateral total skin-sparing (also known as nipple-sparing) mastectomy via a vertical incision between the nipple and the inframammary crease. |
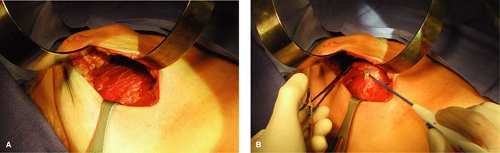 Figure 26.5 A. The pectoralis major muscle via the vertical mastectomy incision after total skin-sparing mastectomy on a large patient who previously wore D-cup brassieres (same patient as in Fig. 26.13). B. Elevation of the pectoralis major muscle toward the sternal border. |
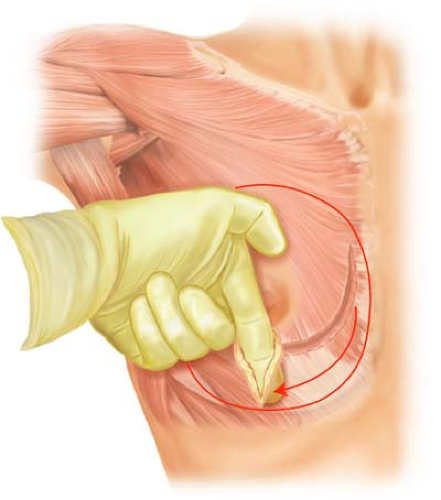 Figure 26.6 The use of blunt dissection in creating much of the submuscular pocket beneath the pectoralis major muscle. |
At this point the procedure is different depending on whether it is a conventional tissue expansion reconstruction with complete muscle coverage or an acellular dermis-assisted reconstruction following a skin-sparing and nipple-sparing mastectomy.
Two-Stage Reconstruction after Conventional Mastectomy-Complete Muscle Coverage over the Expander
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree