Key Words
immediate, implant, breast, reconstruction, single, stage, one-stage, direct, mastectomy
Introduction
Implant-based, or alloplastic, breast reconstruction is the most commonly performed method of breast reconstruction. Within implant-based reconstruction, myriad techniques and reconstructive strategies are at the surgeon’s disposal to provide each individual patient with a successful breast reconstruction. Traditional immediate alloplastic breast reconstruction involves a two-stage approach in which a temporary tissue expander is placed and variably expanded in the outpatient setting, after which it is exchanged for a permanent implant in a second operative procedure. Alternatively, a permanent implant may be placed immediately after mastectomy in a one-stage fashion. This technique obviates the need for tissue expansion and subsequent device exchange. When combined with nipple-sparing mastectomy, the need for nipple reconstruction is also obviated, offering patients the potential for a complete breast reconstruction in a single operative setting.
Compared to two-stage tissue expander–based breast reconstruction, placement of an immediate, permanent device requires greater technical precision in implant pocket creation as well as device selection and placement. While the majority of tissue expander–based reconstructions may be performed with a total submuscular technique, immediate placement of a permanent implant will often require the use of a scaffold for inferolateral support and coverage given the greater initial device volume. Moreover, permanent implants do not allow for adjustment of initial device volume as with tissue expanders. Therefore, a greater initial tissue stress is placed on the overlying breast skin envelope by the underlying implant. Proper patient selection and intraoperative assessment is thus critical to minimize risk of adverse outcomes.
Implant-based breast reconstruction continues to evolve and progress towards complete breast reconstruction in a single stage. Two-stage reconstruction using tissue expansion remains the traditional approach, demonstrating safe and aesthetic results. However, with careful preoperative evaluation and patient selection as well as meticulous operative technique, immediate placement of a permanent device offers the potential for one-stage implant-based breast reconstruction with excellent outcomes.
Indications and Contraindications
General indications for one-stage immediate implant breast reconstruction include two groups of patients in our practice. The first group is patients who qualify for nipple-sparing mastectomy (total skin-sparing) with smaller, minimally ptotic breasts who desire similar sized breasts postoperatively. The second group is patients who are undergoing skin-sparing mastectomy with larger breasts who desire smaller breasts postoperatively.
Patients desiring a larger breast size compared to their preoperative size will inherently require tissue expansion and a two-stage reconstruction. Moreover, elderly patients or those with significant co-morbidities may be preferentially offered single-stage reconstruction to avoid a second surgery and general anesthetic.
Constricted as well as large or ptotic breasts represent relative contraindications for immediate implant-based reconstruction. In these patients, it is often difficult to match the overlying skin envelope to the underlying implant pocket comprised of the pectoralis muscle and, most often, soft tissue scaffold support, such as acellular dermal matrix. This discrepancy will compromise the final aesthetic result of the reconstruction. In patients with larger or ptotic breasts, mastectomy flaps with greater distance to edges and surface area will have increased risk for inadequate perfusion, elevating risk of wound healing complications. Patients with nipple to sternal notch distances greater than 25 cm, severe grade II or grade III breast ptosis must thus be approached cautiously. Further, direct-to-implant reconstruction with devices greater than 400 mL in volume has been associated with increased complications, providing further evidence that patients with and desiring larger breasts represent suboptimal candidates for one-stage implant reconstruction.
Immediate reconstruction using a skin reduction pattern mastectomy incision or delayed mastectomy and reconstruction after staged reduction mammaplasty are strategies to mitigate these issues in patients with larger, ptotic breasts, but carry a higher scar burden with inherent risk of wound healing issues. Reconstruction using a Wise pattern incision and immediate, permanent implant placement may also be combined with an inferior dermal flap for implant coverage. However, wound healing complications remain elevated and were observed in 25% of cases in one series.
Lastly, the volume of a permanent implant cannot be manipulated as with a tissue expander. This places greater immediate stress on the breast skin envelope; therefore any factor that necessitates skin envelope reduction will inherently create greater tissue strain. Therefore, non-nipple-sparing mastectomy techniques and breast tumors close to the skin requiring skin excision may be considered relative contraindications to immediate implant-based breast reconstruction. Severe nipple–areola complex malposition within those undergoing nipple-sparing mastectomy as well as chest wall asymmetry in all patients represent additional contraindications for one-stage implant-based breast reconstruction ( Table 9.1 ).
| Indications | Absolute Contraindications |
|---|---|
Small-breasted patients
Nipple to sternal notch distance <25 cm
Larger-breasted patients
| Patient desire for larger postoperative breast size Severe macromastia Severe chest wall asymmetry Severely constricted base (tuberous breast deformity) Severe preoperative nipple–areola complex malposition (with nipple-sparing mastectomy) Severe grade II/III ptosis desiring nipple-sparing mastectomy |
| Relative Indications | Relative Contraindications |
| Elderly or co-morbid patients | Large, ptotic breasts (grade II/III ptosis) Nipple to sternal notch distance >25 cm Predicted permanent implant size >400 mL Non-nipple-sparing mastectomy Breast tumor close to skin |
Preoperative Evaluation
Patients presenting in consultation for immediate implant-based breast reconstruction should undergo a comprehensive examination to assess their candidacy for a one-stage reconstruction. Such examination should begin with an evaluation of the patient’s breasts. Four aspects of the breast exam are essential in evaluation.
First, the breast footprint and chest wall symmetry should be examined carefully. A constricted breast base or asymmetrical chest wall are relative contraindications for one-stage reconstruction. Any asymmetry should be pointed out and discussed with the patient.
Secondly, the breast envelope including skin quality, elasticity, and ptosis are assessed. Standard breast measurements, including nipple to sternal notch distance, nipple to inframammary fold distance, and base width should be measured. In this regard, the most appropriate candidates for one-stage implant-based reconstruction are those with good skin quality and elasticity, minimal skin laxity, and grade I or mild grade II ptosis with a nipple to sternal notch distance of less than 25 cm. In these patients, mastectomy skin flaps are optimally perfused while the underlying implant pocket can be matched to the overlying breast skin envelope to maximize outcomes. As discussed earlier, patients with nipple to sternal notch distances greater than 25 cm, severe grade II or grade III breast ptosis must thus be approached cautiously as they are at greater risk of reconstructive complications as well as suboptimal aesthetic results.
Thirdly, in patients undergoing nipple-sparing mastectomy, nipple–areola complex position must be carefully assessed. Optimal position is defined as that centered at the most projecting point of the breast combined with minimal or no ptosis. Patients with no or mild nipple–areola complex ptosis are optimal candidates for one-stage implant-based reconstruction whereas moderate ptosis must be approached with caution. Patients with severe nipple–areola complex malposition are better served with a two-stage reconstruction to allow for staged adjustment of nipple position. Nipple position asymmetry should be assessed and discussed. Inter-nipple distance relative to the nipple to anterior axillary line should be assessed. Patients with natural nipple divergence are at a higher risk for lateral nipple malposition postoperatively. In appropriately selected patients, strategies for optimizing nipple–areola complex position at the time of initial reconstruction includes suturing it to the underlying muscle or scaffold as well as setting the proper position after the incisions are closed and immediately placing drains on closed suction. If nipple–areola complex malposition persists or presents postoperatively, various strategies including crescentic excision and mastopexy-type procedures may be successfully employed.
Lastly, breast volume should be assessed and discussed in relation to the desired size. If the patient desires her breasts to be at least one cup size larger, one-stage immediate implant reconstruction should not be offered. In this case, a two-stage technique is preferred as, with a nipple-sparing technique, only a slightly fuller upper breast pole can realistically be achieved with one-stage immediate implant reconstruction. If the patient’s breasts are very large or ptotic and prophylactic mastectomy is planned, we prefer to perform reduction/mastopexy first followed by nipple-sparing mastectomy and one-stage reconstruction in a second operative procedure. In patients with large, ptotic breasts undergoing therapeutic mastectomy in which a staged reduction/secondary reconstruction is precluded, a one-stage immediate implant reconstruction may be performed using a Wise pattern skin incision combined with an inferior pedicle adipodermal flap for additional implant coverage.
With regards to implant selection, there are many important factors to consider. Perhaps the most important measurement in making this decision is base width. Once the base width is measured and selected, implant size and projection are selected based on mastectomy weight and patient preference, balancing implant dimensions with the requisite of minimizing final tension on mastectomy flaps. Implant type must then be determined in conjunction with the patient. Smooth, round implants offer advantages such as a natural feel with less risk of complications, compared to the infectious risk seen with their textured counterparts. Textured, anatomic implants may offer a superiorly visualized breast aesthetic, especially in unilateral reconstructions and patients with a long or tall breast footprint. However, patients must be advised of potential risks of implant rotation and breast implant–associated anaplastic large cell lymphoma with use of textured implants. In our practice, smooth, round implants are utilized in approximately 90% of immediate one-stage implant reconstructions.
Consideration should be given to the possibility of revision. This should be discussed prior to the surgery. Once this reconstructive plan is established, patients may conclude that no further surgery will ever be needed. It is important to emphasize that one-stage implant-based breast reconstruction entails a one-stage breast mound restoration. However, refinement or fine-tuning of the initial result may require a touch-up surgery. This may include fat grafting, implant exchange, scar revision, nipple–areola complex position adjustment, or nipple reconstruction, among other procedures.
Surgical Techniques
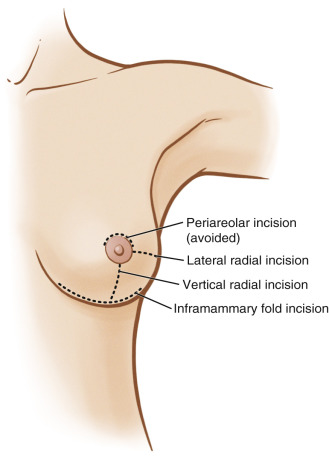
Patients are marked in the upright procedure. The midline is marked using the sternal notch and xiphoid as landmarks. The inframammary fold is marked along with the upper breast border. Mastectomy incisions are designed in conjunction with the oncologic surgeon. In non-nipple-sparing mastectomy techniques, an elliptical incision encompassing the nipple–areola complex is typically chosen. Incision options in nipple-sparing mastectomy include lateral radial and vertical radial as well as inframammary fold approaches. Radial incisions are marked from the edge of the nipple–areola complex. For instance, for a vertical radial incision, the marking extends from the 6 o’clock border of the nipple–areola complex to the midpoint of the inframammary fold whereas in a lateral radial incision, the marking extends from the 3 o’clock or 9 o’clock position of the nipple–areola complex to the midpoint of the lateral breast footprint. Advantages of radial incisions include excellent surgical access to the entirety of the breast for mastectomy; however, the scars are visible on frontal view postoperatively. Inframammary fold incisions may be marked along the entire inframammary fold or only its lateral portion, extending from the midpoint of the breast to the lateral aspect. Advantages of inframammary fold incisions include a well-hidden final scar, but access for mastectomy is more limited, particularly to the superior extent of the breast.
In our practice, these three incision types are most commonly utilized for nipple-sparing mastectomy: inframammary fold (58.3%), lateral radial (18.6%) and vertical radial (13.3%). Inframammary fold incisions are employed for patients with small or moderate-sized breasts while radial incisions are utilized for patients with larger breasts to provide greater surgical access for mastectomy. Radial incisions are also favored in microsurgical reconstruction to allow for better access to the internal mammary recipient vessels. In general, periareolar incisions are avoided, even as extensions of radial incisions, to limit the ischemic insult to the nipple–areola complex ( Fig. 9.1 ). Although less common, vertical radial and inframammary fold incisions may be combined in nipple-sparing mastectomy, especially in patients having undergone a previous breast reduction, to increase surgical access and visualization.
If a skin reduction pattern is chosen in conjunction with skin-sparing mastectomy, markings are similar to those for a Wise pattern breast reduction. Divergent vertical limbs are marked with an apex above the nipple–areola complex and extend along the lateral borders of the nipple–areola complex for approximately 6 cm. The angle of divergence is determined by displacing the breast medially and laterally, aligning the medial and lateral limbs with the breast meridian. Horizontal limbs are then drawn connecting the vertical limbs with the previously created inframammary fold marking. Another horizontal line is then drawn connecting the inferior points of the vertical limbs. This creates a triangle through which the mastectomy will be performed. Once the mastectomy is complete, the inferior pedicle adipodermal flap (hatched lines in Fig. 9.2A ) is de-epithelialized and the horizontal limbs are incised. The remaining procedure is identical to that discussed below with the inferior pedicle adipodermal flap being used for additional inferior device coverage ( Fig. 9.2 ).