Hyperhidrosis
Julia M. Kasprzak
David C. Reid
I. BACKGROUND
Hyperhidrosis is a condition of excessive sweating beyond the expected amount for environmental conditions and thermoregulatory needs. It can be a primary disease process, or it can occur secondary to medications or general medical conditions. Focal hyperhidrosis is a disorder of excess sweating usually in areas of high eccrine density, including the axillae, palms, soles, and, less commonly, the craniofacial area. Focal hyperhidrosis can be idiopathic, related to Frey syndrome (gustatory sweating), or related to neuropathies or spinal conditions. Generalized hyperhidrosis is characterized by diffuse sweating and can occur as the result of a myriad of underlying medical conditions, including endocrine, neurologic, malignancy, infection, cardiovascular, respiratory, medications, and toxicity.
Primary idiopathic focal hyperhidrosis, the form most often encountered in dermatology, has been estimated to affect 3% of the population. While the exact pathologic mechanism is unknown, it is thought that dysregulation of cholinergic fibers of the sympathetic nervous system plays an important role in its pathogenesis. Approximately two-thirds of patients with hyperhidrosis report a positive family history, suggesting a genetic basis for disease.
II. CLINICAL PRESENTATION
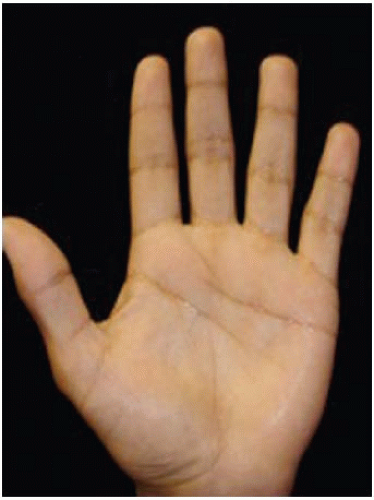
Primary idiopathic focal hyperhidrosis affects men and women equally. The average age of onset is 25 years; however, palmar and axillary hyperhidroses exhibit earlier onset (Figs. 21-1 and 21-2). In order to diagnose primary focal idiopathic hyperhidrosis, the patient must have focal, visible, excessive sweating for at least 6 months with at least two of the following characteristics:
Occurrence of at least one episode of sweating per week
Sweating that is bilateral and relatively symmetric
Impairment of quality of life/daily activities
Onset before 25 years of age
Positive family history of primary idiopathic focal hyperhidrosis
Lack of sweating during sleep
It is important to keep in mind that hyperhidrosis may inflict a significant psychosocial burden on patients. It may cause social anxiety and embarrassment and impair daily activities and intimacy. Focal hyperhidrosis also predisposes patients for infection in the areas of excess perspiration, especially dermatophyte infections.
III. WORKUP
It is important to distinguish between generalized and focal hyperhidrosis by taking a detailed history from the patient. When clinical presentation suggests idiopathic focal hyperhidrosis, no further workup is necessary. If there is suspicion of secondary or generalized hyperhidrosis, additional workup may be needed, including a detailed neurologic evaluation, blood pressure reading, and laboratory tests (complete blood count, fasting serum glucose, and thyroid function tests).
The Hyperhidrosis Disease Severity Scale (HDSS) is a qualitative diagnostic tool that provides a measure of the impact on the patient’s quality of life. This scale can help the clinician to tailor therapy to the severity of the case (Tables 21-1 and 21-2).
IV. TREATMENT
Treatment options include nonsurgical (medical and procedural treatments) and surgical treatments (local dermatologic surgery for axillary hyperhidrosis and sympathectomy for refractory cases). Treatment is guided by severity of symptoms and, often, by the patient’s insurance coverage. Topical medication is usually first-line therapy for focal idiopathic hyperhidrosis, due to its safety and efficacy profile. Procedural therapies such as botulinum toxin A (BTX-A) injections and iontophoresis are second-line treatments useful if topical or oral approaches are ineffective. Oral agents commonly used for hyperhidrosis include anticholinergics, antihypertensives, anxiolytics, and antidepressants; however, there are little data to support the use of oral medications (Table 21-3).
A. Aluminum Chloride Hexahydrate (AC). This is a well-established therapy for focal hyperhidrosis. AC blocks aluminum salt production in the distal acrosyringium, which leads to degeneration of the eccrine acini. Mild cases of hyperhidrosis may respond to over-the-counter antiperspirants. Unresponsive cases may demand prescription strength aluminum chloride 20% solution in ethanol. It should be applied nightly to the affected area, after it has been dried thoroughly. This can be done every night for 1 to 2 weeks, after which application frequency may be tapered. Irritation of the treated area, a common side effect, may be mitigated by occasional application of a low potency topical corticosteroid, such as hydrocortisone 1% cream, on the morning following treatment. A newer formulation of 15% aluminum chloride in salicylic acid gel appears to have similar efficacy as the standard formulation, with the benefit of decreased irritation.
B. Topical Glycopyrrolate.




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree