(1)
Plastic Aesthetic and Laser Surgery, Hygeia hospital, Athens, Greece
Keywords
Complications in eyelid surgeryPatient careReassuranceDecision-makingTiming of complications correctionCorrection of complicationsHematoma, ecchymosisBruisingConjunctival chemosisDry eye syndromeEpiphoraLevator muscle impairment––ptosisPost CO2 laser resurfacing erythemaHyperpigmentationScarring–webbingScleral showResidual fat protrusion in eyelid surgeryInfectionRetrobulbar hematomaVision lossSevere ectropionLower eyelid retractionLagophthalmosSingle-suture traction technique7.1 The Patient’s Management After a Complication
Blepharoplasty is one of the most successful and gratifying operations in facial plastic surgery. Although blepharoplasty operation has a high rate of success, surgeons must always be alert and avoid complacency in their surgical technique. Patients are often unaware of the complexities of eyelid surgery; so thorough patient information and inclusion in management decisions is essential. Even the most skilled aesthetic eyelid surgeon will encounter surgical complications at some point during his career. The experienced surgeon recognizes that many complications can be minimized with thoughtful preoperative planning and careful, meticulous and precise surgical technique. Nonetheless, complications can occur with the best techniques in the best of hands.
The patients’ management after a complication is a very important issue and has to be dealt with care and understanding. Early identification and diagnosis of the problem will significantly enhance the final outcome. Therefore, no compromises are allowed, and symptoms should always be considered seriously and precisely.
Patients should be aware of the existing problem right after the diagnosis of a complication is definite by the surgeon. This is more important in patients who appear with relatively more severe complications such as hematomas, dry eye syndrome, lagophthalmos, ectropion, lower eyelid retraction, etc.
Minor complications which are proved to be resolving spontaneously should also include patients’ awareness and information to avoid undesirable upset and stress in the postoperative period. Reassurance in such cases and instructions for treatments or other measures will help in faster solution of the problem. Most frequent minor to intermediate complications include
Hematoma-ecchymosis-bruising
Conjunctival chymosis
Dry eye syndrome––epiphora
Levator muscle impairment––ptosis
Post CO 2 laser resurfacing erythema and hyperpigmentation
Scarring-rounding
Scleral show
Residual fat protrusion
Infection
Major complications that can lead to long-term problems and need more specific care and evaluation are as follows:
Retrobulbar hematoma and vision loss
Severe ectropion
Lower eyelid retraction
Lagophthalmos
7.2 Decision-Making and Timing of Correction
It is more than important, the timing of correction, for any of the above complications to be decided in sobriety and composure, with no sentimental affect to the surgeon’s decision from the justified pressure of the patient for solution of the problem in the shortest time frame possible. Patients with any kind of complications can develop very serious psychological effects, for several reasons, such as professional, social, personal, etc., which are directly associated to their appearance and the expected long downtime ahead. Detailed explanation of the measures that have to be applied for the correction of a complication should be discussed with them and the possibility of an inadequate or failed final outcome revealed, if inappropriate decisions related to the above mentioned facts are to be taken.
I have found that the majority of patients that presented with, most commonly, minor complications overexaggerate the situation, pressing for quick and accelerated treatment. Dedication of time, pampering, and explanation of anatomical and physiological factors that have contributed to the complication, together with appropriate layout of its management, have proved to be very helpful in increasing the patient’s compliance to my decisions and time frame of the correction.
Complications which do not need any further surgical intervention for their resolution, such as excessive postoperative edema, bruising, minor hematomas, ecchymosis, mild chemosis, or dry eyes have to be addressed as soon as they are diagnosed with appropriate medical treatment or other procedures which can be helpful. The use of low-level laser treatments (LLTT), light treatments, lymphatic drainage massage treatments, etc. can adequately improve the postoperative course of the patients who present with prolonged edema, bruises, minor hematomas, post laser erythema, or hyperpigmentation and significantly reduce the patients’ discomfort and impatience. Closer and more frequent follow-up is also an important factor to keep the patient reassured and relaxed.
Complications that will potentially need further surgical intervention in the future have to be initially addressed with conservative treatments, which will improve the postoperative early surgical sequelae of the tissues involved. These include minor or major scleral show, ectropion, lower eyelid retraction, and lagophthalmos. On the contrary, early incision dehiscence due to trauma, incorrect intraoperative wound closure, or patients’ incompliance to postoperative instructions in the first week following surgery has to be corrected when diagnosed, with wound debridement and resuturing. Late scar dehiscence needs to be addressed differently and at a later stage, with scar revision.
Surgical correction of persisting lagophthalmos, scleral show, ectropion, or lower eyelid retraction has to take place at later postoperative stages, depending on the evaluation of the tissue’s postoperative course and quality. To my experience, shortening of the postoperative interval of the correction, due to patients’ impatience, has mostly led to unlucky and unfavorable results which create a new vicious circle with unpredictable effects both to the patient’s psychology and to the tissue itself to be recorrected.
7.3 Correction of Complications
Depending on the kind of complication, appropriate measures should be undertaken to address them, as stated above. Patient should be informed of what he might consider as a complication than a common postoperative effect in the first postoperative days and reassured. In the existence of a complication, the surgeon has to frankly announce and explain to the patient the plan of treatment. Most common complications and their treatment are described below.
7.3.1 Conservative and Nonsurgical Management of Complications
7.3.1.1 Postoperative Bruising, Ecchymosis, and Edema
Although these side effects are very common and expected, following a blepharoplasty operation, many patients become very stressed when they appear and despite the fact that they have been aware of such sequelae. Postoperative edema usually worsens during the initial 24–48 h after surgery. The degree of swelling is often directly related to surgical factors such as ecchymosis, excessive cauterization, extensive tissue manipulation or excision, and dissection in the lateral canthal area resulting in lymphatic disruption. Therefore, measures to avoid such intraoperative manipulations should be taken in order to reduce the incidence of severe edema. Moreover, ice water compresses right after surgery and continuous use for 72 h reduce the possibility of severe edema and bruising.
If, even though, the onset of severe and bruises cannot be avoided, either medication or other treatments can help to delay further deterioration and resolve the problem faster.
Use of Arnica orally or locally has been claimed to help, and some patients ask for this even without mentioning them the treatment.
Light treatments with low-emission diode (LED) high-intensity phototherapy devices, emitting in red and near-infrared spectrum, have also proved to help in wound healing and as anti-inflammatory tools. Everyday treatments postoperatively during the first week help in accelerating edema and partial bruising resolve. Low-level laser therapy with devices emitting in the same spectrum as LED provide the same results.
Massage-induced lymphatic drainage is also very helpful. Special exercises instructed to the patients using their fingers and applying smooth and efficient pressure periodically on the affected area have also been advocated in our practice in such cases.
Treatments start right after diagnosis of severe or annoying edema in the first follow-up visit of the patient.
7.3.1.2 Conjunctival Chemosis
Chemosis of the eye is a medical condition, in which the conjunctiva of the eye becomes swollen. The condition is mainly caused by the exudation of the small capillaries of the eye, presenting an abnormal permeability. Chemosis occurs when the eye has been irritated, representing however a nonspecific sign. The conjunctiva will appear as if having liquid in it. The inflammation of the conjunctiva leads to an overall gelatinous appearance. The degree of the swelling varies from one patient to the other and, sometimes, it can become so inflamed that the patient will have difficulties closing the eye (completely or partially). Due to the inflammation, the eyeball might appear as if moved from its original position (it should also be noted that the eyeball is not covered by the excess fluid) (Fig. 7.1).
Fig. 7.1
Conjunctival chemosis
The cause of conjunctival chemosis is multifactorial, and includes exposure, periorbital edema, postoperative lymphatic dysfunction, mechanical injury during surgery or pharmaceutical agents. It appears intraoperatively or in the first postoperative week, with an average duration of 4 weeks, depending on the mechanism which caused it.
Authors have classified chemosis in four different types as follows [1]:
- 1.
Acute mild chemosis with complete lid closure
- 2.
Acute severe chemosis that prohibits complete lid closure (chemosis-induced lagophthalmos)
- 3.
Subchronic chemosis that persists longer than 3 weeks and
- 4.
Chemosis associated with lower lid malposition
In most cases, chemosis resolves spontaneously with the use of local lubricating and anti-inflammatory agents.
Transconjunctival incision can be a triggering factor of chemosis formation, particularly if not performed accurately and precisely. Transconjunctival infiltration of local anesthetic solution in lower blepharoplasty in a superficial plane under the conjunctiva might also cause chemosis due to dispersion of fluid under the conjunctiva. In both cases, the effect is temporal and resolves with local treatment in due course.
Surgical procedures for fluid drainage with conjunctivectomy or temporary tarsorrhaphy have also been reported, but in very rare cases. Prevention of chemosis-triggering factors during surgery is the most appropriate and important procedure to avoid this complication.
7.3.1.3 Dry Eye Syndrome and Epiphora
This quite common complication following a blepharoplasty operation can be triggered by several factors such as intraoperative canthopexy, postoperative temporary lagophthalmos, concurrent upper and lower blepharoplasty, and transcutaneous approaches violating the orbicularis oculi muscle.
Patients may experience dry eyes within the first few weeks after surgery. Persistent dry eye can occur and, in some cases, can be due to a preexisting problem or a surgical complication.
Some factors that can make it more likely to develop dry eyes after an upper eyelid blepharoplasty include thyroid problems, bulging eyelids, prior history of dry eyes, poor eyelid skin tone, weak eyelid ligaments, certain autoimmune diseases, defects in the tear duct pathways, as well as removal of too much eyelid skin during surgery, or significant postoperative swelling.
When these factors can be identified preoperatively, measures can be taken to avoid or reduce the risk of permanent dry eye. Depending on the nature of the problem, a conservative eyelid skin removal may be needed. In other patients, special lid-tightening procedures, such as SSTT, can be performed in addition to eyelid surgery to avoid problems. In some cases where there is a high risk of developing dry eyes, complete avoidance of blepharoplasty surgery may be advised.
Treatment of dry eye early on after a blepharoplasty includes the application of natural tears or medical eyedrops as well as lubricating ointments to keep the eyes moist. If dry eye persists for more than a few weeks despite topical treatment, special care and ophthalmological evaluation should be undertaken.
While permanent dry eye after eyelid surgery can be prevented in many instances, dry eye syndrome is a risk of surgery. Patients should be aware of all the risks of surgery, even when they are low.
In our series, we have noticed a low evidence of dry eye syndrome after blepharoplasty surgery, due to meticulous preoperative patients’ assessment and continuous efforts for precise surgery and avoidance of tissue damage during the operation. However, in 17% of patients, despite all the appropriate measures, dry eye symptoms have developed following blepharoplasty, which in the vast majority were transient and quickly resolved after local treatment.
Treatment of dry eye syndrome should be initiated right after patients complain of dryness of the eyes and include the following.
- 1.
Lubricant treatments
Mild-to-moderate cases of dry eye syndrome can usually be treated using lubricant eye treatments that consist of a range of drops, gels, and ointments.
These lubricants are often called artificial tears, because they replace the missing water in the tear film. However, they do not contain the antibodies, vitamins, and nutrients found in normal tears that are essential for eye health. Eye ointments can also be used to help lubricate the eyes and keep them moist overnight, as tears can evaporate during sleep time if the eyelids are not completely closed. These ointments tend to be used overnight because they can cause blurred vision.
- 2.
Anti-inflammatory treatments
The underlying problem with long-term dry eye syndrome is inflammation in and around the eye.
Corticosteroids are powerful anti-inflammatory medications that can be given as eyedrops or ointments in severe cases of dry eye syndrome and with cautious use due to their side effects (cataract, raise of eye pressure, etc.).
In severe cases, most unlikely to my experience, occlusive patches, contact eye lenses, and lipid and hormonal treatments have been used.
Epiphora is an excessive tearing condition of the eyes caused by a reflex tear secretion due to several factors. The eyelid blinking dysfunction after blepharoplasty is a common side effect due to postoperative swelling of the eyelid tissues. This dysfunction interferes with the tear pump mechanism.
The swelling can also cause the puncta to turn inward or evert by swelling or tissue contraction caused by incision lines or laser resurfacing, which also causes epiphora.
Lagophthalmos also can increase reflex tear secretion, due to primary dryness of the eyes, leading to relative epiphora.
Epiphora, if present, following a blepharoplasty operation and caused by the above reasons, is transient and resolves with edema reduction by time.
However, measures have to be taken during surgery not to damage important anatomical structures which can lead to very persistent and difficult-to-correct epiphora. Damage to the lacrimal outflow system can occur if the incision line is carried too medially and too close to the horizontal midline. The punctum is a useful landmark for the upper lid and lower lid incision. For an upper lid blepharoplasty, ending the incision just lateral to the punctum avoids medial canthal webbing as well as lacrimal system injury. Incisions should be at least 4–5 mm above the punctum to avoid the canaliculus. In the lower lid blepharoplasty, the medial part of the lower eyelid incision should stop lateral to the punctum, both in the transconjunctival and the subciliary type of incision.
Mild and transient epiphora has very rarely been noticed in some of our patients as a reflex tear secretion developed due to dry eye syndrome after blepharoplasty operations, and in all cases resolved spontaneously with eye lubrication, after diagnosis.
7.3.1.4 Levator Muscle Ptosis
Levator muscle and levator aponeurosis are two anatomical features that should be protected from injury during upper blepharoplasty operation.
Symptoms similar to ptosis, but not due to levator muscle or aponeurosis injury, can occur on the next postoperative day in several patients. However, this is a result of the consequent edema of the eyelid and the muscle itself, and the experienced surgeon who has identified and preserved the levator muscle and aponeurosis will not be alarmed.
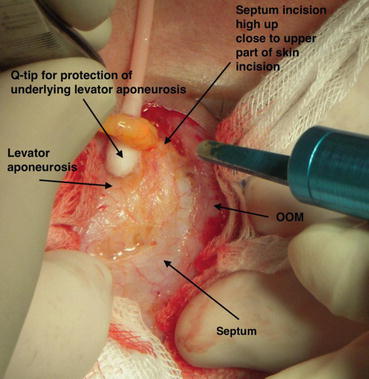
As described in Sect. 4.3.3, the levator muscle and its aponeurosis is the plane where the upper blepharoplasty fat removal is performed. To avoid any injury, incision to the septum should be performed high up toward the upper part of the skin incision, and the levator elements should be identified before fat removal, as the pulling of the freed fat pad upward can bring together the superficial part of the levator aponeurosis. Gentle detachment of the aponeurosis is required with a q-tip and not sharp instruments at this stage. The excision of the fat pad with CO2 laser should also provide protection of the underlying aponeurosis with a backstop which in most cases is a cotton pad or q-tip Fig. 7.2. The same protection measures, as for the levator aponeurosis in upper blepharoplasty, also apply in the lower eyelid transconjunctival or subciliary approach, to protect the inferior oblique muscle injury.