Chapter 55 Graft Remodeling and Ligamentization After Anterior Cruciate Ligament Reconstruction
Several studies have analyzed the various changes that occur during graft healing.1–24 Two main sites of healing exist, which should be separately assessed because their biological processes vary substantially: the intraarticular graft remodeling, often referred to as ligamentization, and the intratunnel graft incorporation, which develops either by bone–bone or tendon–bone healing.
In the beginning of the 20th century, Wilhelm Roux described the “law of functional adaptation,” elucidating on the fact that “an organ will adapt itself structurally to an alteration, quantitative or qualitative in function,”25 laying groundwork for later research on ligamentization. He observed that soft tissue structures such as ligaments and tendons undergo specific changes in their mechanical and biological properties when they are exposed to a different mechanical loading and biological environment. Amiel et al were among the first authors1,26 to analyze the specific functional adaptation of an ACL replacement graft and postulate the term ligamentization. They found a continuous development of a patellar tendon graft with biological and mechanical properties different from the ACL into a structure that closely resembled these properties of the intact ACL. They showed that the patellar tendon underwent several phases of remodeling: an early phase with central graft necrosis and hypocellularity and no detectable revascularization of the graft tissue. This was followed by a phase of proliferation—the time of most intensive remodeling and revascularization—and finally a ligamentization phase that provided characteristic restructuring of the graft toward the properties of the intact ACL. Amiel described this process as a transformation, not a restoration, of the native ACL because characteristic differences remained compared with its replacement grafts. This study laid the foundation for increased research efforts to improve the understanding of the basic science of intraarticular ACL graft healing or ligamentization. With the evolution of ACL reconstruction techniques to graft fixation in bone tunnels, it was not until the beginning of the past decade that the first studies were published on the biological processes during osseous graft incorporation.* It was recognized that the combined healing of the intraarticular remodeling and the intraosseous graft incorporation was dictating the mechanical function of the joint after ACL reconstruction.
Early Graft-Healing Phase
In comparison to studies of the subsequent proliferation and ligamentization phases, significantly less studies exist with analyses of the biological events of this early graft healing phase. Most authors agree, using different in vivo animal models,1,2,18,30,31 that this time period is marked by increasing graft necrosis, mainly in its center, and hypocellularity. Ultrastructural cell changes such as mitochondrial swelling, dilatation of the endoplasmatic retinaculum, and intracytoplasmatic deposition of lipids, as well as macroscopic swelling and increased cross-sectional area, illustrate the increasing graft necrosis and degradation.30 During this time, no graft revascularization can be observed.2,9,32,33 The graft necrosis leads to a release of a number of cytokines, such as tumor necrosis factor (TNF)–a, interleukin (IL)–1ß, and IL-6, in addition to chemokines that trigger a cascade of growth factors expression, which in turn result in cell migration and proliferation as well as extracellular matrix synthesis and revascularization.11,34 This remodeling activity becomes more pronounced during the latter proliferative phase. However, already between the first and second weeks, an influx of cells can be seen into the graft’s periphery.30,31 Kleiner et al9 and later Yoshikawa et al33 were able to demonstrate that these cells were originating from tissue other than the graft itself and that all original graft cells were completely replaced by 2 to 4 weeks. They hypothesized that the source of cells was either the synovial fluid, cells from the stump of the native ACL, or bone marrow elements originating from drilling maneuvers. Therefore Arnoczky2 suggested that preservation of the ACL stump and the Hoffa fat pad might be beneficial, especially for the early healing period.
During the first postoperative weeks, the graft’s overall collagen structure and its crimp pattern are still maintained,1 even though the beginning disintegration of the collagen fibrils and their orientation can be observed as early as 3 weeks after reconstruction.30,35 This explains the slow decrease in the mechanical properties of the graft at this early healing phase.4,15,20
Very little is known about the healing processes in the osseous tunnels, which will be described in more detail in the following chapter of this book. In summary, only little graft incorporation can be seen during this early stage of healing, such that the mechanical properties of the freshly ACL reconstructed knee joint are primarily relying on the mechanical fixation of the graft. Biomechanical testing of intraarticular ACL reconstructions between 2 and 4 weeks4,5,13,20 shows consistent failure by graft pullout from the tunnel, indicating insufficient anchorage of the graft to the tunnel wall. The mechanical strength of the ACL reconstruction at this time is significantly lower than that at the time of implantation. However, it continues to decrease until around 6 weeks, when a further increase in graft remodeling activity can be found and the failure site shifts to the intraarticular graft region.4,15,20
The decrease in mechanical strength might lead to the conclusion that early graft loading (i.e., immediate loading of the freshly reconstructed knee joint) should be avoided. However, several studies have pointed out the importance of adequate mechanical loading for the healing graft. Ohno et al36 stress-deprived the patellar tendon in vivo and found a significant loss of tensile strength as early as 1 week with further deterioration until 6 weeks of healing. This loss in tensile strength was accompanied by splitting and defragmentation of collagen bundles as early as 2 weeks. Similar findings were reported by Majima et al,37 who examined differences in complete and partial stress-shielding of a soft tissue graft, detecting a significantly higher loss in tensile strength from the first to third week of healing for the complete stress-shielded group. In another study38 the authors explained this observation with ultrastructural changes in the collagen composition that shifted to small-diameter fibrils, which were shown to provide less mechanical strength than the large-diameter fibrils found in the intact ACL.39,40 However, overloading of the graft can also lead to impaired graft healing. Tohyama and Yasuda showed in their model using an in situ frozen patellar tendon that a reduction of the cross-sectional area of the tendon by half (thereby doubling the tendon stress during loading) resulted in substantially reduced tensile strength as early as 3 weeks, contrary to only a slight increase in tendon stress (when the cross-sectional area was reduced by only one-third), which did not significantly impair the mechanical strength.41
Proliferation Phase of Graft Healing
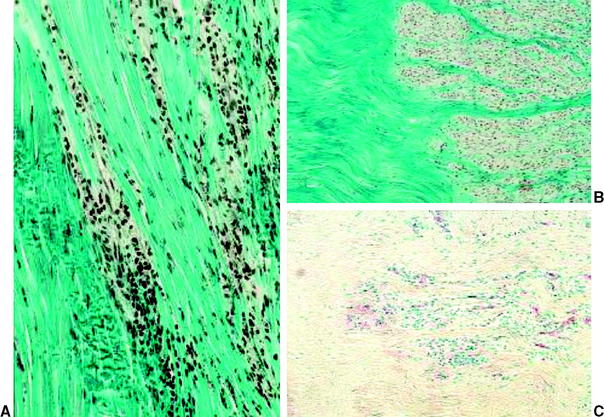
During this phase, cellularity constantly increases and substantially surpasses that of the intact ACL, as was observed in various in vivo animal models.3,8,18,20,42 Cell clusters are found at the perimeter of the graft around 6 weeks, with large acellular areas remaining in the graft’s center (Fig. 55-1). These hypercellular regions were shown to consist of mesenchymal stem cells18 and activated fibroblasts11 that are actively secreting several growth factors such as basic fibroblast growth factor (bFGF), TGF-ß1, and isoforms of platelet-derived growth factor (PDGF) to initiate and maintain graft remodeling. Kuroda et al11 found that the release of these growth factors peaks between the third and sixth week and almost completely ceases at 12 weeks of healing, which lends further explanation for the maximum remodeling activity during this proliferation phase. A more even distribution of cells throughout the graft slowly develops thereafter. Cell numbers are still increased but recede toward the intact ACL cellularity at the end of the proliferation phase.17,20 An increased number of specific fibroblasts, so-called myofibroblasts, are also found during this healing phase.43,44 These fibroblasts have the ability to exert isometric tension on the surrounding cellular and extracellular matrix. In the intact ACL they seem to be responsible for the crimping structure of the collagen fibers.45 These contractile fibroblasts are progressively expressed during the first three postoperative months17,44 in the healing ACL graft, when they seem to be responsible for the restoration of the in situ tension that is required for the later ligamentization process.
At the same time of increased cellular proliferation and intense revascularization of the graft tissue, Yoshikawa et al24 found upregulated expression of vascular endothelial growth factor (VEGF), a potent stimulator of angiogenesis, already at 2 to 3 weeks postreconstruction, which is triggered by hypoxia during the avascular necrosis of the early healing phase (Fig. 55-2).47 However, they did not find a significant increase in vascular outgrowth before the fourth and eighth week, confirming the descriptive findings of other previously published studies. Petersen et al14 and Unterhauser et al42 independently showed that revascularization progresses from the periphery of the graft toward the entire graft diameter at the end of the proliferation phase around 12 weeks of healing (see Fig. 55-2). Vascular density then returns to values of the intact ACL during the phase of ligamentization by 6 months.14,42 It is assumed that this intense revascularization triggers and retains the maximal remodeling activity. It has been a matter of debate whether such increased revascularization is beneficial to the healing of the graft. Recent studies found that upregulation of revascularization (e.g., by exogenous application of VEGF) enhanced cellular infiltration and fibroblast expression during the proliferation phase of healing, but this also included a significant deterioration of the graft’s mechanical properties.33 Weiler et al were able to relate the vascularity of the healing ACL graft in sheep to its mechanical properties using gadolinium-enhanced magnetic resonance imaging (MRI).23 They found that the time of maximal revascularization coincides with the lowest mechanical properties of the healing graft tissue, which was seen around 6 weeks. Tohyama and Yasuda were able to show that increased remodeling activity in terms of extracellular infiltration and revascularization was directly related to the decline in the graft’s mechanical properties.19 These findings support the reports of numerous other studies that all found the mechanical properties to be at their minimum around the proliferation phase of healing at 6 to 8 weeks.*. Graft failure at this time point occurs either by midsubstance tear20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree