Genital Anatomy
Libby Edwards
Knowledge of the anatomy of the genitalia is important, because both the vulva and the male genitalia are composed of different structures and types of skin, each of which is predisposed to different diseases. Both male and female genitalia contain dry, keratinized skin and modified mucous membranes, and the female vestibule is composed of a mucous membrane. Also, understanding of different anatomical sites is useful in communicating with other providers. For example, a biopsy labeled “vulva” is less useful to the pathologist than one labeled “vestibule,” since the normal histology for these two areas is considerably different.
Dermatoses on genital skin often present differently than when occurring on extragenital dry, keratinized skin surfaces. Scaling is inapparent in damp skin folds, and some diseases, such as lichen sclerosus, preferentially affect modified mucous membrane skin rather than true mucous membrane. A knowledge of anatomy and the various normal appearances of the genitalia helps with the recognition of both normal structures and pathologic findings.
Female Genitalia
Vulva
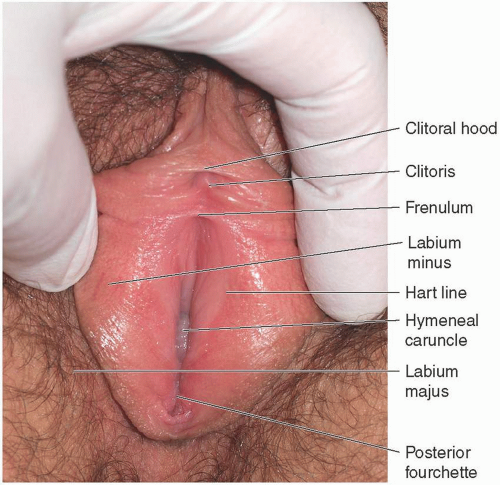
The vulva consists of the mucocutaneous structures that compose the external female genitalia (Fig. 1.1). The vulva extends from the mons pubis anteriorly to the perineum posteriorly and from the crural folds laterally to the hymen and hymeneal ring medially.
The labia majora (singular = labium majus) are two fatty folds of skin that are derived from ectodermal tissues. The labia minora (singular = labium minus), medial to the labia majora, are much thinner folds of connective tissue and squamous epithelium. The vestibule, or introitus, is mucous membrane that extends from the medial origin of the labia minora to the hymeneal ring. The mons and labia majora cover and protect more delicate structures such as the clitoris, the clitoral hood, the labia minora, the vestibule, and the posterior fourchette, which is the posterior vestibule, extending to the perineal body.
The vulva exhibits several different types of epithelium. The lateral aspect of the labia majora is covered with dry, keratinized, conspicuously hair-bearing skin. Each hair follicle is part of a pilosebaceous unit comprising the follicle itself, its hair shaft, the sebaceous gland, and the arrector pili apparatus—a smooth muscle that contracts to form gooseflesh.
Although the medial aspect of the labia majora and the entire labia minora are generally considered to exhibit hairless mucous membrane epithelium, these areas actually are covered with partially keratinized skin that contains several structures, including subtle hair follicles. Numerous apocrine sweat glands lie on the modified mucous membranes of the labia minora, and ectopic sebaceous glands (Fordyce spots) are often prominent, especially on the medial aspect of these skin folds. Sebaceous glands appear as small, yellow to white, lobular papules (Fig. 1.2). A variably distinct line of demarcation (the Hart line) is evident at the base of the medial aspect of each labium minus, separating modified mucous membrane from the mucous membrane skin of the vestibule. The medial aspect of the labia majora and the entire labia minora display moist, partially keratinized modified mucous membrane. Nonkeratinized, non-hair-bearing squamous mucosal epithelium with mucus-secreting glands extends from the Hart line to and including the vagina and the external surface of the cervix. Mucosa is defined as a membrane that lines body structures that communicate to the air, and generally produce lubricating mucous. In general, mucous membrane skin is non-hair-bearing epithelium that contains mucus-secreting glands. Both the vagina and the vestibule are covered with mucosae, whose surfaces are variably wet (depending on estrogen status) as a result of mucus produced by associated glands and the cervix.
The vestibule, or introitus, extends from the Hart line to the hymen. Variable numbers of mucus-secreting vestibular glands open onto the mucous membrane of this area. These glands are shallow pits lined with secretory cells; these primarily open circumferentially around the external aspect of the hymeneal ring and between the hymen and urethra (Fig. 1.3) but are occasionally visible
on other areas of the vestibule (Fig. 1.4). They supplement lubrication in young, postpubertal women. Bartholin glands are paired glands that lie under the posterior portion of the vestibule, with duct openings just outside the hymen at the 5 and 7 o’clock positions. Skene glands exit into the distal urethra.
on other areas of the vestibule (Fig. 1.4). They supplement lubrication in young, postpubertal women. Bartholin glands are paired glands that lie under the posterior portion of the vestibule, with duct openings just outside the hymen at the 5 and 7 o’clock positions. Skene glands exit into the distal urethra.
The vulva undergoes marked change from birth until puberty (see Chapter 14). The skin of the mons and the lateral labia majora is characterized by fine vellus hair at birth, but with puberty, coarse terminal hair appears. In addition, the labia minora are almost absent until the onset of puberty, when estrogen appears. The modified mucous membranes are smooth in prepubertal girls, before developing the normal sebaceous glands and redundant tissue of the estrogenized vulva. Apocrine glands become better developed with sexual maturity.
 FIG. 1.2. Fordyce spots most often appear as faintly yellow papules on the medial labia majora and lateral labia minora. |
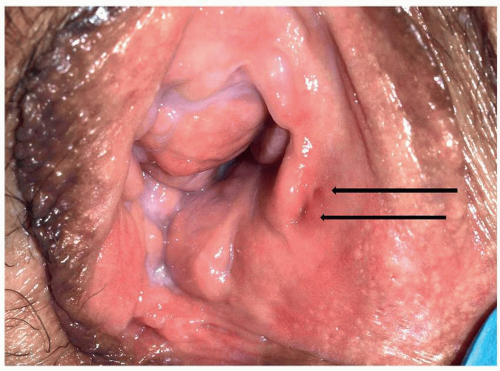 FIG. 1.3. Pits that represent the ostia of vestibular glands occur regularly adjacent and lateral to the hymenal caruncles (arrows). |
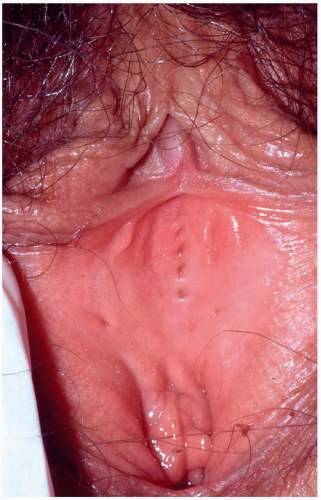 FIG. 1.4. Vestibular gland ostia also occur on other areas of the vestibule but are often very subtle. This vulva shows distinct ostia in the anterior vestibule. |
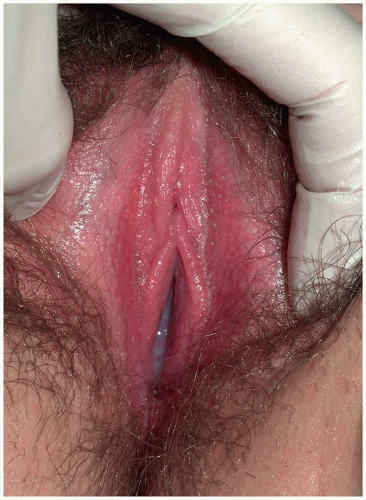
Normal Variants
Similar to the mucous membrane epithelia of the mouth and conjunctivae, mild erythema of the vulva and vagina is normal and varies from patient to patient. In one reported series of premenopausal women, 43% showed erythema (Figs. 1.5 and 1.6) (1). This redness is more evident in patients of light complexion, especially those with a naturally ruddy complexion. This finding is often misinterpreted by patients and their physicians as indicative of inflammation because the asymptomatic vulva is rarely examined critically. In addition, more than half of the women with vestibular erythema report no dyspareunia, but experience pain when the area is touched with a cotton-tipped applicator (the Q-tip test). This indicates that redness and a positive Q-tip test are normal findings and do not, alone and in the absence of real-life symptoms, constitute the vestibulodynia pattern of vulvodynia, formerly called the vulvar vestibulitis syndrome.
Vulvar papillae (see Chapter 5) are also common normal variants, occurring in about one third of premenopausal women (Figs. 1.7, 1.8, 1.9, 1.10 and 1.11) (1,2). When these occur in the vestibule, they are called vestibular papillae. These variants are often mistaken for signs of disease, usually condylomata acuminata. Initial descriptions of vulvar papillomatosis reported biopsies consistent with human papillomavirus (HPV) infection as the cause. However, biopsies of even normal vulvar skin generally show large, clear keratinocytes that mimic koilocytes of HPV infection. More recent studies have evaluated for the actual presence of the virus. The current consensus is that vestibular papillomatosis is a variant of normal, and this morphology is distinct from HPV infection (2,3). These small, soft, monomorphous, tubular projections are located symmetrically within the vestibule, whereas papillae of other areas of the vulva are more likely to be dome-shaped and less tubular. Vulvar papillae differ from condylomata acuminata by their rounded rather than acuminate tips and symmetric pattern. Vulvar papillae are
discrete to the base, whereas condylomata acuminata generally are fused at the base to adjacent lesions. Moreover, genital warts are often keratinized and appear white in this moist area.
discrete to the base, whereas condylomata acuminata generally are fused at the base to adjacent lesions. Moreover, genital warts are often keratinized and appear white in this moist area.
 FIG. 1.8. Vulvar papillae sometimes form symmetrical lines, particularly at the edge of the Hart line. |
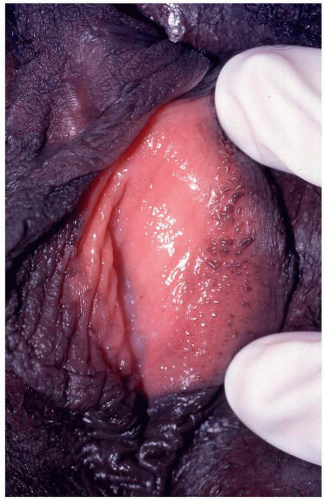 FIG. 1.9. Vulvar papillae can be more discrete and separated and, in some patients who are darkly complexioned, pigmented. |
 FIG. 1.10. Vulvar papillae can be short and closely set, giving a cobblestoned appearance to the skin. |
Occasionally, similar dome-shaped, smooth papules that coalesce into a cobblestone texture on the inner labia minora occur in some women. Sometimes, these lesions form papules on the edge of the labia minora. These changes are also often mistaken for warts. Although vulvar papillae were once believed to produce itching or pain, they are now known to be asymptomatic.
The whitening of vulvar skin following the application of 5% acetic acid has been believed to be pathognomonic of HPV infection and intraepithelial neoplasia. Although very sensitive, this is a nonspecific finding occurring with any condition that produces hyperkeratosis or thickening of the skin (4). Some investigators have found that
5% acetic acid predictably produces acetowhitening of all vulvar skin with prolonged contact (1).
5% acetic acid predictably produces acetowhitening of all vulvar skin with prolonged contact (1).
 FIG. 1.11. Although vulvar papillae are found most often in the vestibule and medial labia minora, they can occur on edges of the labia minora, as seen here. |
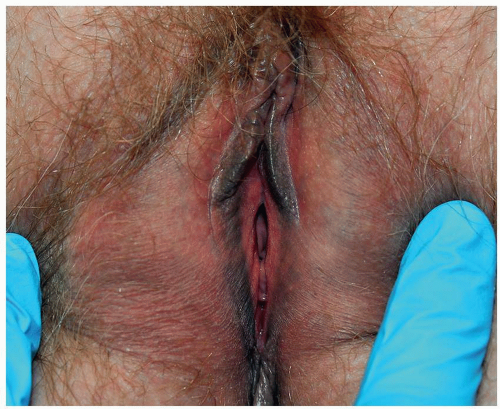 FIG. 1.12. The labia minora in this woman are very small and also display physiologic hyperpigmentation. |
Labia minora exhibit wide morphologic variability. These folds of skin can be large and pendulous, so small as to be nearly absent, or very asymmetric (Figs. 1.12, 1.13 and 1.14). The anterior origin of the labia minora is the frenulum of the clitoris, but often the anterior origin is from several structures, with a contribution from the skin lateral to the clitoral hood (Fig. 1.15), and the posterior aspect of the labia minora can be fused (Fig. 1.16).
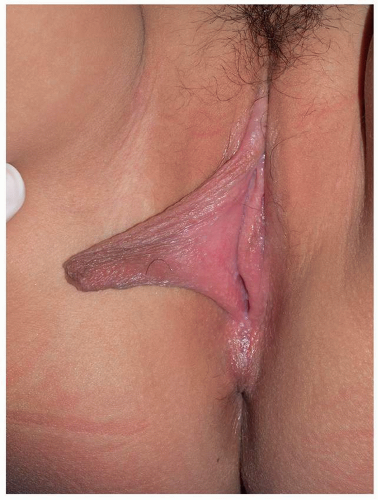 FIG. 1.13. Labia minora normally enlarge at puberty; this 12-yearold presents asking for labioplasty of her enlarged right labium minus which catches in her underwear. In the next 8 months, her left labium minus enlarged to that same size.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|