Frontal Sinus Obliteration With Fat
Matthew M. Smith
Alessandro de Alarcon
DEFINITION
Obliteration of the frontal sinus is the process of replacing a diseased frontal sinus that is normally air-filled.
The diseased frontal sinus is obliterated with another material, such as fat.
ANATOMY
The midface is made up of five paired paranasal sinuses (maxillary, anterior ethmoid, posterior ethmoid, sphenoid, and frontal)
The boundaries of the frontal sinus are as follows:
Anterior: Anterior wall of the frontal sinus
Posterior: Posterior wall of the frontal sinus and anterior cranial fossa
Inferior: Orbit
The anterior wall of the frontal sinus is significantly thicker than the posterior wall.
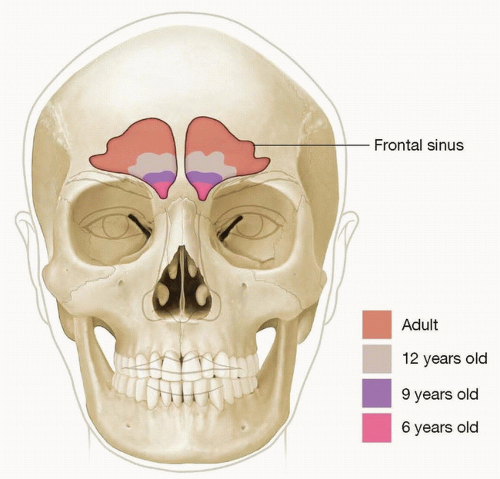
The frontal sinus is the last paranasal sinus to develop and usually begins to pneumatize around 6 years of age (FIG 1).
It is innervated by the supraorbital and supratrochlear nerves, which are branches of the first branch of the trigeminal nerve (V1).
The frontal sinus drains into the middle meatus via the hourglass-shaped frontal sinus outflow tract. The boundaries of the frontal sinus outflow tract are as follows:
Anterior: Nasofrontal bar, agger nasi cell
Posterioinferior: Ethmoid bulla
Posterosuperior: Anterior cranial fossa
Medial: Middle turbinate
Lateral: Lamina papyracea
PATHOGENESIS
Frontal sinus injury is the primary indication for frontal sinus obliteration.
Chronic frontal sinusitis secondary to obstruction of the frontal sinus outflow tract.
Prior frontal sinus surgery with subsequent mucocele formation.
Frontal sinus malignancy with subsequent need for obliteration after resection of tumor.
Direct forehead trauma with subsequent frontal sinus wall fractures.
Isolated anterior frontal sinus wall fractures with displacement and nondisplaced posterior wall frontal sinus fractures without CSF leak are the most amenable to frontal sinus obliteration.
Displacement of the posterior frontal sinus wall and/or CSF leak is more frequently treated with cranialization of the frontal sinus rather than obliteration.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history for each patient will be directed toward the proposed cause of his or her frontal sinus problem.
For all patients, it is important to obtain history regarding changes in vision, mechanism of frontal sinus injury (chronic inflammatory, traumatic), nasal obstruction, persistent clear rhinorrhea, purulent rhinorrhea, fevers, headaches, swelling of the forehead, changes or lack of smell, prior sinus surgeries, and symptoms of meningitis.
A complete visual examination should be performed, including visual acuity, visual fields, pupillary reflex, accommodation, and extraocular movements.
Anterior rhinoscopy should be used to examine the nasal cavities for any evidence of trauma, CSF leak (clear rhinorrhea), or malignancy prior to frontal sinus surgical intervention.
Nasal endoscopy is not needed to view the frontal sinus prior to surgery but is useful if the patient has had prior surgery and allows the frontal sinus outflow tract to be easily viewed with an angled endoscope (45 or 70 degree).
If the patient has symptoms of persistent or intermittent clear rhinorrhea, the patient should be instructed to sit in a sniffing position for 3 minutes with a small basin or cup to collect the clear nasal drainage. This fluid can then be sent for examination of beta-2-transferrin for confirmation of CSF leak.
For those patients with a history of traumatic frontal sinus fracture, the evaluation for potential foreign bodies within the frontal sinus and other craniofacial fractures should be completed.
IMAGING
CT scan of the sinuses is paramount for the bony framework of the frontal sinuses.
Axial, sagittal, and coronal views should all be obtained to fully view the frontal sinus in different planes (FIG 2A,B).
0.5-mm cuts should be obtained in order to detect small defects in the frontal sinus.
3D reconstruction of the frontal sinus can be obtained and is helpful, but not necessary.
Historically a 6-foot Caldwell view with an AP x-ray of the head was obtained. A quarter was placed over the patient’s forehead during the x-ray to create an image that could then be laid over the patient for an actual size of the frontal sinus.
MRI with contrast should be obtained prior to surgery if violation of the posterior frontal wall is suspected to ensure there is no evidence of an encephalocele and to further evaluate the surrounding soft tissues (FIG 2C).
DIFFERENTIAL DIAGNOSIS
Chronic frontal sinusitis
Pott puffy tumor
Frontal sinus mucocele
Frontal sinus fracture
Encephalocele
Frontal sinus malignancy
NONOPERATIVE MANAGEMENT
For nondisplaced fractures of the anterior frontal sinus, observation is an option, but with any type of mucosal disruption, the patient will be at risk for mucocele or mucopyocele.
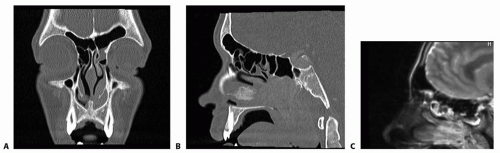
FIG 2 • A. Coronal CT showing bone window. B. Sagittal CT showing bone window. C. Sagittal MRI T2 sequence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access