Fig. 49.1
(a, b) Penile anatomy
The super-wet technique is used for lipoextraction. Approximately 100 mL of lipo- aspirate is obtained and processed. A small incision allowing for the cannula size just above the peno-pubic junction is made. After identifying the dartos muscle and Buck’s fascia (Fig. 49.1), the author pre-tunnels in a crisscross fashion with the injection cannula. This prevents degloving, which would diminish the blood supply, and the fat is then injected into the tunnels from distal to proximal. The tunnels hold the fat in place and prevent its migration. The fat is allowed to drain by gravity and no washing done in order to preserve the SVF. Washing done in the past was a mistake since it removed much of the SVF. The SVF is separated and the fat is centrifuged at 3,000 RPMs for 3 min. Oil and debris are discarded. The fat, albumin, PRP, and SVF are combined (Fig. 49.2) and injected with the control gun syringe technique, in a plane created by the tunneling. This plane allows for the best exposure of the fat to the capillary ingrowth (Fig. 49.3). Care is taken as a rule not to inject fat beneath the urethra. The skin is very thin and damage to the urethra is possible.
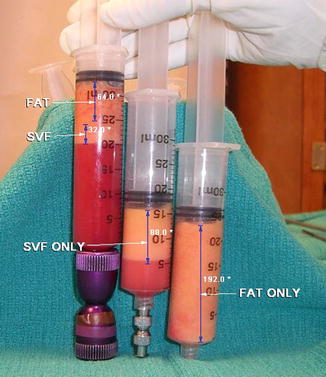

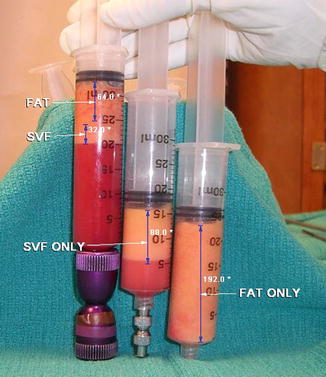
Fig. 49.2
The stromal vascular fraction (SVF) is separated and the fat is centrifuged at 3,000 RPMs for 3 min. Oil and debris are discarded. The fat, albumin, PRP, and SVF are combined

Fig. 49.3
Retrograde injection of free fat graft using automatic injection
The average amount of material injected varies from 60 to 80 mL or however much is decided upon to use. The incision is closed and a protective dressing applied (Fig. 49.4). The patient is discharged when fully awake and normal activity is allowed the next day. Normal follow-up care is according to the surgeon’s routine and of course as needed.
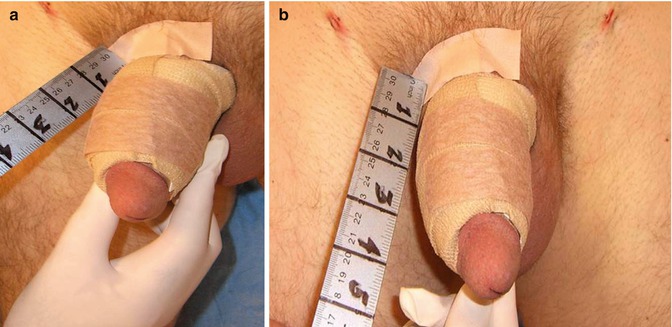
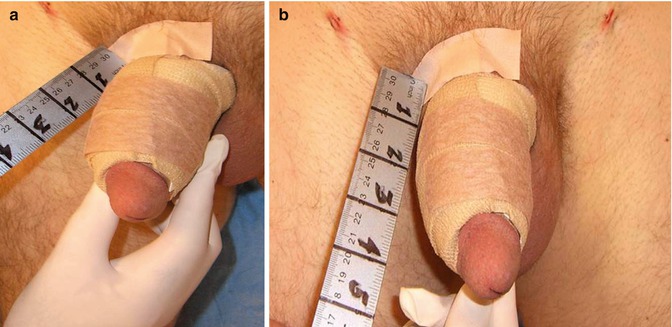
Fig. 49.4
(a, b) Postoperative wrap
The second stage is planned at or after 3 months. Accurate statistics are difficult to obtain since many men, being men, fail to follow the program or do not return. However, approximately 20–25 % of the patients return for the second stage within the first year, and half of these are to make the penis even larger, not because of significant loss of fat or complications. Several patients have returned many years later doing well but requesting further enlargement for various reasons. The same post-op program is followed with second-stage patients.
Postoperative care program includes:
Usual postoperative antibiotics, pain killers, and regular diet
Vitamin E 400,000 UQD 1 month
No sexual activity for 6 weeks
No lower body or aerobic exercises for 4 weeks
Wrap penis 10 days (Fig. 49.4)
Hand stretching every 2 h for 1–2 min while awake
49.6 Complications
True complications are rare and not to be confused with the post-op side effects of swelling and bruising. In FFG alone pain is minimal or absent. Donor site problems are virtually nonexistent, and these are best prevented by adherence to Halsted’s fundamental principles of asepsis, hemostasis, and gentle handling of tissues. The “real” complication is the failure of the FFG to survive. A certain amount of loss is to be expected and must be explained to the patient along with emphasis on the two-stage approach and strict adherence to the postoperative program (POP). Total loss of fat is rare and usually due to the failure to follow the POP or unexpected events.
49.6.1 Infection
Infection of the FFG alone is less than 1 %. Superficial infections are rare and respond to standard care. Deep infections in the FFG are extremely rare and deemed statistically insignificant. In any event, waiting 4–6 months to replace any loss of fat is advised after the infection has cleared.
49.6.2 Lumps, Clumps, and Bumps
These are the main object of criticism for FFG both in the public and physician minds. Prevention is the best treatment by following the POP; however, fibro fatty nodules (FN) occur in 3–4 % of patients and vary in size (Figs. 49.6 and 49.7). Early treatment by massage and manual disbursement can prevent formation of FNs. The patient should be made aware to start to do this to himself, since the earlier the better. Surgical treatment consists of morselizing the formation when possible or excision. Avoid incisions on the penile skin; they heal with noticeable scaring. Approach from the skin of the peno-pubic junction or the circumcision scar. Use of Cavitron Ultrasonic Surgical device (CUSA) works well to “melt” the exposed nodule and avoid surrounding damage. However, this may not be readily available [20].


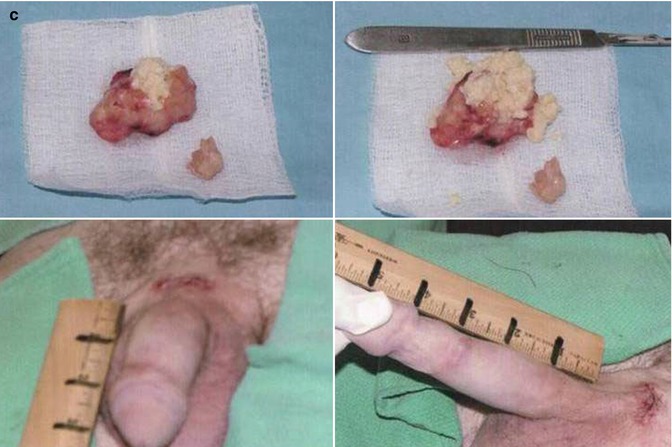

Fig. 49.6
Fibronodular excision

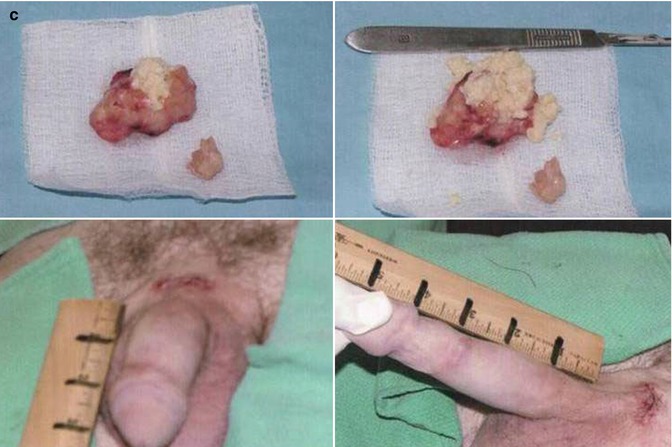
Fig. 49.7
(a) Patient with nodules. (b) Surgical approach. (c) (Upper) Specimen. Note cheese-like appearance of degraded fat. (Lower) Postoperative
49.6.3 Overfilling
Overfilling with fat is easily avoided. The area distal to the circumcision scar is problematic due to diminished blood supply and scarification.
49.6.4 Other Complications
Irregular accumulation of fat can occur in this area (Fig. 49.8). Approach through the circumcision scar will provide the best exposure and least chance of damage to the glans (Fig. 49.8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









