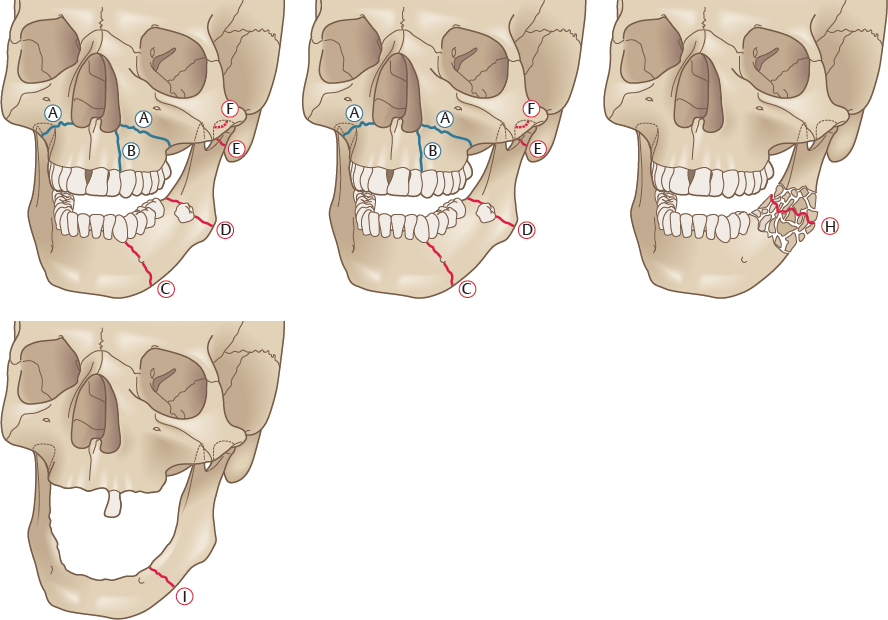
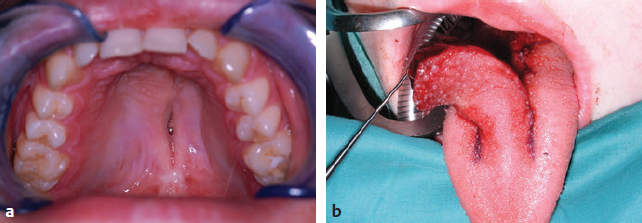
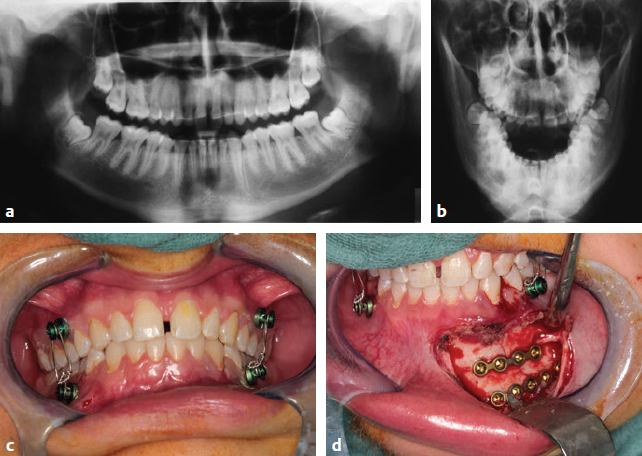
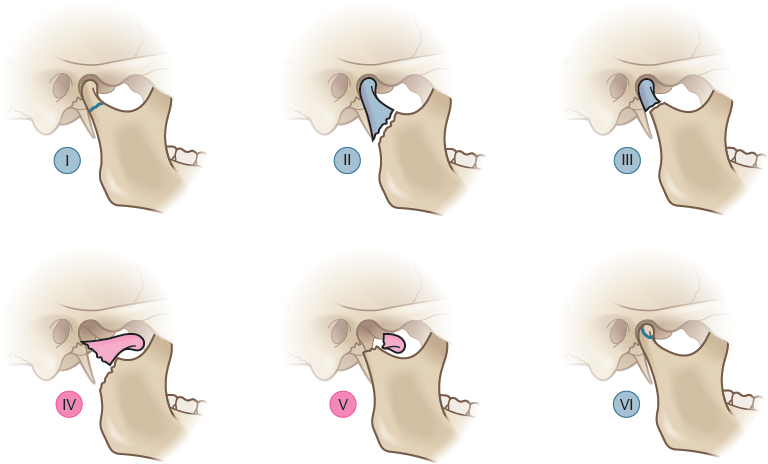
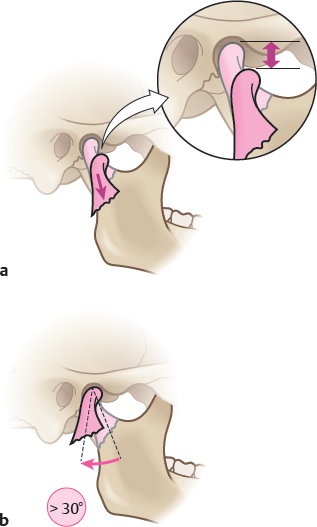
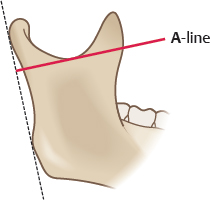
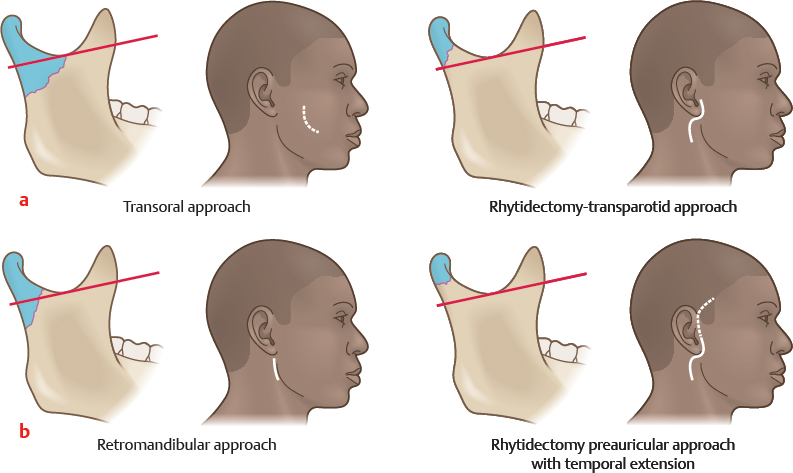
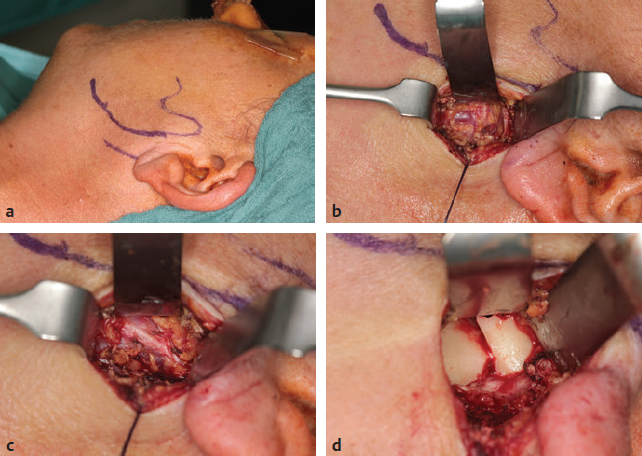
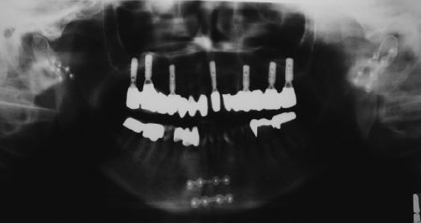
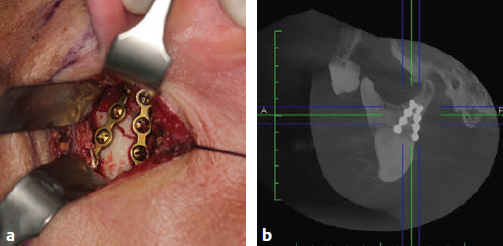
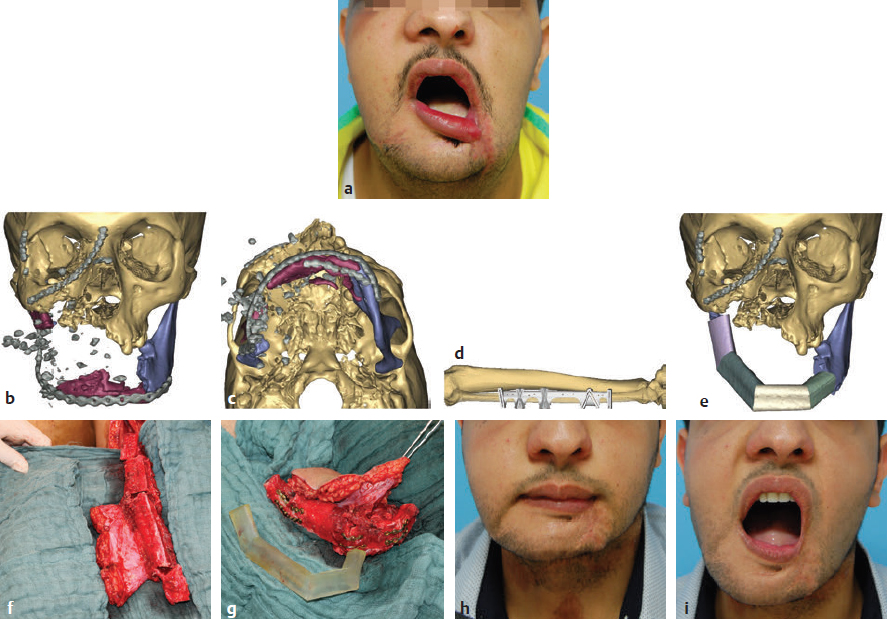
CHAPTER The long-term outcome after jaw fractures depends not only on the type of fracture and the precise restoration of the broken bone, but also on the integrity of all anatomic structures neighboring the fracture. Choosing the appropriate surgical approach is an additional key factor for avoiding complications. This chapter focuses on the management of upper and lower jaw fractures. Direct and indirect forces to the lower and upper jaw result in fractures. Several low-resistant anatomic locations with thinned bone are prone to fractures. Typical fractures (Fig. 47.1) of the maxilla include the so-called Le Fort I fracture, in which the maxilla breaks off the midface (A in Fig. 47.1), and sagittal fractures (see B in Fig. 47.1), which involve transverse expansion of the upper jaw. With regard to the mandibular bone, the parasymphyseal (see C in Fig. 47.1) and the angle (see D in Fig. 47.1) regions are prone to fractures. The extended root of the lower canine and the foramen of the mental nerve are responsible for parasymphyseal fractures, whereas retained wisdom teeth are a determinant in angle fractures. The thin condylar neck (see E in Fig. 47.1) including the condylar head (see F in Fig. 47.1) is another fragile region of the mandible. High-velocity trauma leads to comminuted fractures (see G in Fig. 47.1). In particular, the uncompleted median symphysis in children is highly vulnerable. Pathologic conditions of the bone such as osteomyelitis or osteonecrosis (see H in Fig. 47.1) increase the risk of fractures, as does an edentulous, highly atrophied body of the mandible1,2 (see I in Fig. 47.1). The anatomical complex of the upper and lower jaw is functionally involved in clenching and speaking, but also plays a significant role for facial aesthetics. Restoration of painless unlimited mouth opening, laterotrusion, and protrusion is one of the main targets after jaw fracture. Perfect occlusion should be recovered in dentate patients, and the harmonic red-white aesthetics of teeth and gingiva should be reestablished. As a basis for later prosthetic rehabilitation, the accurate positioning of the maxilla and mandible in the vertical, transversal, and sagittal dimension is always necessary.3 Undesirable results after treatment of jaw fractures arise, in most cases, because of deficient clinical and radiological diagnostics and insufficient treatment planning.4 To a lesser extent, poor outcome results from the failure of the patient to cooperate or from a lack of postoperative care. Open reduction and internal fixation (ORIF) is the basic reconstructive principle in nearly all types of jaw fractures. Since their development in the 1970s, titanium miniplates represent the osteosynthesis material of first choice for the maxilla and for the mandible.5 Fundamental publications have described the buttresses of the facial bones.6 Most postoperative complications can be avoided when the rules of miniplating along the natural strains of the bones are strictly observed. For exceptional cases in which bone has been sheared off, lag screws might be a therapeutic alternative. Particular attention must be paid to jaw fractures in childhood. The jaw bones of children have a high potential for bone remodeling. Reconstructive principles have to be modified; closed reduction is a sufficient therapy in many cases.7 If ORIF is conducted, plate removal must be performed much earlier. Fig. 47.1 Types of jaw fractures (blue, maxillary fractures; red, mandibular fractures). A, Le Fort I fracture. B, Sagittal upper jaw fracture. C, Parasymphyseal fracture. D, Angle fracture. E, Fracture of the condylar process. F, Fracture of the condylar head. G, Comminuted fracture. H , Pathologic fracture (osteomyelitis, osteoradionecrosis, medication-related osteonecrosis). I, Fracture of the atrophic jaw. This chapter concentrates on the most challenging types of jaw fractures, because of their high potential of therapeutic failure. After the breaking off of the midface, the pterygoid muscles pull the fractured upper jaw into a dorsal position. Nonocclusion, open bite, and nasal airway restriction result. In the long term, the facial profile changes by the retral position of the maxilla and the subnasal region. The patient presents with pseudoprogernia. When reducing the fracture, retral positioning of the maxilla must be avoided, and particular attention should be paid to the exact positioning of the maxilla. A posteriorly impacted maxilla must be pulled forward. Significantly delayed cases should be reduced with Rowe’s maxillary disimpaction forceps. The two-pronged instrument grasps the maxilla with a palatal blade and a blade positioned in the nasal cavity. After reduction, meticulous mandibulomaxillary fixation is necessary to secure the occlusal relationship until osteosynthesis with miniplates is performed. After ossification of the malpositioned maxilla, a secondary correction must be carried out. Preoperative planning is therefore indispensable. First, plaster models from the maxilla and mandible are made, a checkbite is performed, and the positions of the maxilla with respect to the temporomandibular joint (TMJ) and the cranial base are determined with a face-bow. To imitate the position of the jaws and the mandibular movements, upper- and lower-jaw casts are positioned correctly in an adjustable articulator. With respect to the posttraumatic and intended facial profile, occlusion and aesthetics model osteotomy is performed on the casts. The exact movement of the maxilla in three dimensions is ascertained and marked on the model. Occlusal splints, namely a starting splint and a postosteotomy splint, are made on the basis of the model operation. These splints are fixed between the maxilla and the mandible during the Le Fort I osteotomy. Summary Box Unfavorable Results and Complications Associated with Fractured Jaw Repair Maxilla Fractures • Le Fort I fractures – Open bite – Nasal airway restriction • Sagittal fractures Mandibular Fractures • Plate exposure • Injury to mental nerve • Injury to root of lower canine • Infection Condylar Process Fractures • Malocclusion • Condylar absorption • Arterial hemorrhage • Nonocclusion • Reduced mouth opening • Limited mandibular movement • Osteonecrosis • Scarring • Facial nerve paralysis • Parotid fistulae • Infection • Scarring stenosis of the auditory canal • Dislocation of osteosynthesis material Comminuted Fractures • Discontinuity of the bone • Infection (abscesses, cellulitis, osteomyelitis) • Nonunion and malocclusion • Nerve injury Pathologic Fractures • Class A • Class B • Class C Atrophic Jaw Fractures • Complication in bone healing • Stability loss of mandible • Extraoral plate exposure • Intraoral plate exposure • Fractured osteosynthesis material Childhood Jaw Fractures • Facial asymmetry • Malocclusion/open bite • Joint ankylosis Secondary correction of maxilla malpositioning can also be carried out by virtual planning of a Le Fort I osteotomy. Once a computed tomography (CT) scan of the middle and lower face is obtained, the data is prepared with a special software to gain a virtual three-dimensional model. The required movement of the maxilla can be simulated, and individual cutting guides and osteosynthesis material for the Le Fort I osteotomy can be produced by industrial partners within a few days.8 Sagittal fractures are accompanied by transverse malposition, resulting in transverse expansion of the maxilla and nonocclusion. In some cases, sagittal fractures with extensive dislocation cause lacerations of the palatal soft tissues with oronasal communication. The alveolar process is often tilted, which makes it difficult to achieve a sufficient occlusion solely by maxillomandibular wiring. The fabrication of an individual acrylic palatal plate might be indicated for better stabilization of the palatal vault. After this pretreatment, osteosynthesis is carried out with miniplates being placed on the frontal part of the maxilla. Additional problems might arise from laceration of the palatal gingiva. Primary tension-free closure is challenging, because mobilization of the palatal soft tissue is nearly impossible. As an unfavorable result, a persistent oronasal fistula might occur. Closure of such fistulas is hampered by scarring. The use of a pedicled palatine flap and the mobilization of the buccal fat pad are therapies of the first choice for oronasal fistula closure. Techniques for the closure of recurrent or extended oronasal fistulas are associated with much more donor site morbidity and include the tongue flap or a radial forearm flap (Fig. 47.2). Fig. 47.2 Persistent oronasal fistula after sagittal fracture of the maxilla. (a) After repeated trials of primary closure. (b) Final closure with a tongue flap. The treatment of these types of mandibular fractures is based on the miniplating techniques developed by the group led by Champy9 in the 1970s. With the exception of the angle region, two monocortical fixed miniplates (four-hole or six-hole) are placed on the buccal surface of the mandible. Whereas one plate is fixed below the dental roots, the other one is fixed at the mandibular base to neutralize moments of torsion (Fig. 47.3). In the angle region, the muscle sling of the masseter and medial pterygoid muscles compresses the strains of the mandibular base. Therefore placement of a single plate running from the postmolar oblique line to the buccal molar region is adequate. If the principles of miniplate osteosynthesis are fulfilled, complications are rare. Unfavorable results such as plate exposure can arise when the intraoral incision is placed directly over the fixed titanium plates. Postoperative smoking and poor oral hygiene are cofactors that increase the risk of plate exposure. Particular attention must be paid to the mental nerve and the root of the lower canine in parasymphyseal fractures. Injuries of these anatomic structures from incorrect placement of screws and miniplates can easily be avoided. If plate exposure occurs, further infection of the region must be prevented. Strict oral hygiene must be maintained, including antiseptic mouthwashes, and the patient must be seen weekly in the maxillofacial outpatient clinic. Osteosynthesis material removal is delayed to at least 2 months to allow bony consolidation to be completed. The treatment of condylar fractures is a controversial topic. During the past decade, much effort has been made to improve the outcome of condylar fractures, but after critical consideration, many of the “new techniques” have been abandoned as fast as they have emerged. Taking all conflicting points into consideration, the surgeon has the choice of treating all cases conservatively or performing ORIF on the other. Various complications arise after the fracture and treatment of the condylar neck and head. Functional, aesthetic, and neurosensory deficits are common.10 Malocclusion, reduced mouth opening, and limited mandibular movement are often associated with the pterygoid lateral muscle pulling at the fractured and nonfractured fragments.1 Malocclusion also results because of the dislocation of the condylar process and subsequent reduction of ramus height. Osteonecrosis of the condyle might be an unfavorable result of traumatic or iatrogenic disruption of the blood supply to the small broken fragment. Surgery-associated problems include unfavorable scarring and facial nerve paralysis, mostly of the marginal mandibular branch, after use of an extraoral approach for ORIF. In addition, parotid fistulas and sequential infections have been described after a transcutaneous transparotid approach to the fractured condylar process. Scarring and subsequent stenosis of the auditory canal is also a problem that arises after ORIF of condylar head fractures through a retroauricular approach.10 Fig 47.3 Management of mandibular fractures. (a,b) Radiologic diagnostics are performed in two planes with panoramic and mandible posteroanterior radiographs. (c) Maxillomandibular fixation with screws and wires. (d) Open reduction and internal fixation with miniplates considering the anatomy. The technique of the anatomic repositioning of the condylar head fragments with trapezoid plates and successive definitive screw fixation to the stable mandible can result in the dislocation of osteosynthesis material. A via falsa of the inserted screw with significant harm to surrounding structures can occur. Although bleeding from the external auditory meatus is common after posterior dislocation of the condylar head, the penetration of the fractured condyle to the middle cranial fossa might, in rare cases, result in life-threatening infections and complications.11 Modern diagnostics of condylar process fractures should not rely only on clinical parameters and plain radiographs such as panoramic and mandible posteroanterior radiography. Mandible posteroanterior radiographs might provide a hint to the grade of dislocation of the fractured segment. For an exact classification of the segment and determination of the treatment concept, a further investigation with a three-dimensional technique (computed tomography [CT], cone beam computed tomography [CBCT]) is required. Exact and reliable control of the post-therapeutic effect on the posttraumatic state can only be achieved by CT and CBCT. The condylar fracture classifications of Spiessl et al.12 and Loukota et al.13 are helpful in determining whether the fracture should be done operatively and which surgical approach is the most suitable. The classification by Spiessl et al.12 (Fig. 47.4) suggests that ORIF is definitely indicated for healthy adults with type IV and type V fractures (Box 47.1). Luxation of the condylar head out of the TMJ socket is associated with a massive loss of vertical height and nonocclusion and, in bilateral luxations, with the development of an iatrogenic malpositioning of an adjusting screw and retral position of the mandible. Therefore the repositioning of the condylar process and the securing of this position by osteosynthesis is essential (Fig. 47.5a). The classification by Spiessl et al.12 does not differentiate between the severity of dislocation in type II and type III fractures. Dislocated fractures with a deviation of the condylar process of less than 30 degrees can be treated by maxillomandibular fixation and early functional therapy (Fig. 47.5b). This suggestion includes, in particular, unilateral cases, cases without loss of vertical height, and posttraumatic normo-occlusion. Wired arch bars for maxillomandibular fixation should be used in all cases with slight dislocation. In type I and type VI fractures without dislocation, I recommend four bone screws be placed between the roots of the canines and the first premolar carefully avoiding violation of the teeth or their roots. During the first postoperative week, maxillomandibular fixation must be ensured by rigid elastics (type III and IV), after which soft elastics (type VI to VIII) are indicated for another 3 weeks. Soft elastics should allow mouth opening and alleviate functional therapy. Rigid maxillomandibular fixation should be limited to 2 weeks, especially in younger patients, to prevent bony ankylosis of the TMJ. Radiographic observations after maxillomandibular fixation are essential to detect spontaneous dislocation during manipulation at an early stage. If this occurs, secondary ORIF is necessary. Fig. 47.4 Fracture types of the mandibular condyle as classified by Spiessl et al, with indications for open reduction and internal fixation marked in pink. Open reduction and internal fixation (ORIF) is recommended in mandibular condyle fractures with the following characteristics: • Luxated condylar fragment • Dislocation of the condyle of more than 30 degrees • Massive loss of vertical height Exceptions to the algorithm can/must be: • Posttraumatic normo-occlusion • Multimorbid patients with potential life-threatening risk during narcosis • Children younger than 12 years with a high potential of condylar remodeling • ORIF is indicated (even in slight dislocations) in*: Fig. 47.5 Indications for open reduction and internal fixation in fractures of the mandibular condyle. (a) Loss of vertical ramus height. (b) Dislocation of the condylar fragment of more than 30 degrees. Because of the earlier mentioned risks of ORIF in condylar head fractures (condylar head resorption, stenosis of the auditory canal, facial paralysis, and dislocation of osteosynthesis material), I recommend closed reduction with functional therapy in such cases. If primary therapy results in nonocclusion, I recommend orthodontic therapy followed by secondary orthognathic surgery after several months. Loss of vertical height can be corrected by vertical ramus osteotomy. Loukota et al.13 published a new classification of condylar fractures in 2005. They defined an anatomic A-line that crosses the most inferior point of the semilunar incisure of the mandible. The A-line starts as a perpendicular line to a tangent touching the most posterior points of the ramus and the condylar head13 (Fig. 47.6). To define the surgical approach, The A-line is an extremely helpful tool for determining the surgical approach (Fig 47.7). Although numerous approaches to the mandibular condyle have been developed, I rely on three main approaches depending on the anatomic position of the fracture with regard to the A-line. Condylar base fractures located inferior to the A-line are reduced via an intraoral approach (Fig. 47.7a), condylar base fractures running through the A-line are treated by a retromandibular approach (Fig. 47.7b), and condylar neck fractures superior to the A-line are reduced via a rhytidectomy-transparotid approach (Fig. 47.7c). The latter approach can be extended as a preauricular incision superior to the temporal region if the condylar head region must be reached (Fig. 47.7d). Fig. 47.6 Anatomic relationship in fractures of the condylar process. The A-line is a perpendicular line to the mandibular ramus tangent running through the inferior part of the incisure of the mandible. Fig. 47.7 Recommendation for the surgical approach with respect to the anatomic location of the condylar fracture. When approaching a condylar base fracture transorally, the overview to the backside of the ascending ramus is reduced. Nevertheless, correct repositioning of the fragments is essential, and hooks and retractors are helpful. However, iatrogenic injuries caused by pulling forces to the retromandibular vein and the accompanying marginal mandibular branch of the facial nerve must be avoided. In the early 2000s, the technique of endoscopic revision of condylar fractures via a transoral approach was commonly cited in the literature.14,15 However, four main complications are common with this technique: 1. Arterial hemorrhage 2. Facial nerve injury 3. Nonunion 4. Partial condylar reabsorption After critical analysis of their results, Arcuri et al.16 believe that this is not an ideal approach for a subcondylar fracture but might be an alternative procedure in selected cases. With the retromandibular approach (Fig. 47.8), the surgeon must pay particular attention not to injure the marginal mandibular branch of the facial nerve. Therefore it is useful to prepare the retromandibular vein after skin incision (see Fig. 47.8b) and to visualize the nerve (see Fig. 47.8c). The periosteum is cut anterior to the marginal mandibular branch, and the fracture is exposed (see Fig. 47.8d). The vestibular surface and the posterior rim of the ramus are prepared to obtain a complete overview of the fractured bone. Distraction of the anterior mandible is commonly necessary to reduce the dislocated fragments anatomically. The algorithm recommends a rhytidectomy anteroparotid-transparotid approach for condylar neck fractures. To prevent complications involving the facial nerve, a strictly subcutaneous preparation is necessary after skin incision. The capsula of the parotid gland is either saved when carrying out an anteroparotid approach or dissected horizontally when a transparotid approach is used. When the anteroparotid approach is used, dissection is carried out subcutaneously until the masseter muscle is reached in front of the gland and until the overlying nerve branches have become obvious. Attention must be paid to leaving the excretory duct of the gland intact. The parotid gland is then retracted backward, and the masseter muscle is cut horizontally between the two nerve branches. The fracture can be exposed and anatomically reduced. After osteosynthesis, meticulous control of hemorrhage is essential. Reconnection of the masseter muscle with 3–0 or 4–0 resorbable suture is also mandatory to restore its function. A suction drain is inserted before skin closure to prevent hematoma and hematoma-induced facial nerve palsy. Cutaneous closure is performed with 4–0 or 5–0 nonresorbable sutures to prevent scarring. The transparotid approach involves cutting the parotid capsule parallel to the nerve branches. Nerve branches must be detected by an electrostimulation device. The incision of the capsule is marked with sutures to visualize it later. After dissection of the gland and the masseter muscle, a more direct view of the fracture becomes visible than via the anteroparotid approach. However, the masseter muscle must be reattached and the capsule closed tightly after osteosynthesis. Tight capsular closure is essential to prevent salivary fistulas that might occur in about 1% of the cases.17 Treatment of salivary fistulas or sialoceles can be either carried out surgically by reevaluation of the parotid or conservatively. Acceptable conservative regimens include, as a first step, compression bandaging and drainage and, as a second step, the insertion of a feeding tube for 8 days and additional administration of antisialogogs.18 A single injection of botulinum toxin type A to the parotid gland has also been described as a promising therapy.19 Fig. 47.8 The retromandibular approach for a condylar base fracture. (a) Preoperative marking of the anatomic landmarks and incision. (b) Preparation of the retromandibular vein. (c) Exposure of the marginal mandibular branch of the facial nerve anterior to the retromandibular vein. (d) Visualization of the fracture. Fig. 47.9 Fatigue of osteosynthesis material and consecutive plate fractures in both condylar regions. Fig. 47.10 Correct angle of 30 degrees between two 2-mm miniplates in a condylar base fracture. (a) Intraoperative view after open reduction and internal fixation. (b) Postoperative control using cone beam computed tomography. Osteosynthesis is one of the most important, if not the key procedure in the surgical treatment of condylar fractures. Many osteosynthesis systems are available. Special osteosynthesis plates and screws have been developed to fulfill the requirements of the mandibular condyle (e.g., lag screws, triangular plates, locking plates, resorbable plates). The system must fit the usually small condylar fragments, be adaptable via the restricted approach, and withstand bite forces (Fig. 47.9). The correct placement of the osteosynthesis material into the condyle process and the mandible has been the matter of myriad investigations. Tensile and compression forces to the mandible and its condylar process have been measured by photoelastic analysis, three-dimensional biomechanical simulation models, and finite element models.20–22 The results of these investigations stress that two-plate fixation with 2-mm four-hole miniplates is superior to all other stabilization techniques.22,23 Meyer and colleagues24 states that “more and more authors advocate the use of two miniplates. The first is placed in the axis of the condylar neck as usual, and the second is placed obliquely under the mandibular notch.”24 In my own experience and in accordance with Meyer,24 two miniplates are needed. After anatomic reduction of the fracture, the first four-hole miniplate is placed in the axial direction of the condylar neck. With gracile condylar necks, particular attention should be paid to ensure that the first plate is placed posteriorly enough for the second to be positioned anteriorly. Monocortical screws of 5 mm or 6 mm are used to fix the plate. After this maneuver, a control of the occlusion is recommended. If the occlusion is correct, the second plate is placed (according to the natural strains) 30 degrees in an anterior direction to the first, and all screws are drilled in (Fig. 47.10). The gold standard for postoperative control is three-dimensional radiographic observation by CT or CBCT. Postoperative radiography is essential, not only for forensic reasons. Exact and detailed documentation of the pretreatment and post-treatment status can be of high value if complications—such as malocclusion; mastication pain; or nearthrosis, pseudarthrosis, or ankylosis—arise. Secondary dislocations of the nonoperated site might occur, especially in bilateral condylar fractures with unilateral conservative treatment. Distraction maneuvers during anatomical reduction can often cause these dislocations. In consequence, secondary corrections with ORIF have to be performed. Comminuted fractures occur after high-velocity trauma or shotgun injuries. They are characterized by bone that is crushed into a number of smaller fragments. For this reason, anatomic repositioning can be extremely difficult. Osteosynthesis is hampered by the lack of fixation options for the small bony segments. Because of the trauma mechanism, comminuted fractures are often associated with remarkable injuries to the neighboring tissues, with lacerations of the gingiva and facial skin or even the loss of soft tissue with subsequent defects. The prevalence of fractured, loosened, or knocked-out teeth in these types of injuries is high. Foreign bodies or bullets penetrate soft tissue and bone. In addition to the difficulties of anatomic repositioning and stabilization of the bony fragments, several complications can arise with this type of fracture: • Discontinuity of bone • Infection, mainly as abscesses, cellulitis, or osteomyelitis because of the following: • Nonunion or malocclusion • Nerve injuries The discontinuity of bone results primarily after traumatic loss of a bone fragment or secondarily because of infection and necrosis of a segment. In extended comminuted fractures, a step-by-step approach is recommended to prevent the previously mentioned complications and unfavorable outcomes. First, wounds are cleansed with polyhexanide 0.4% or Ringer’s lactate solution via a syringe; then the surgeon performs a meticulous search for foreign material and tooth fragments. Foreign material, dental fragments, and teeth with vertical fractures and pulp exposure are removed. Teeth in malposition are manually replaced into their sockets without touching the root region. These teeth are fixed with interdental titanium-composite splints for stabilization. If occlusion is reproducible, maxillomandibular fixation is performed, and intraoral soft tissue is closed if necessary. Thereafter the mandible is (if possible) stabilized in occlusion, and the fracture is manually reduced via an extraoral approach. The separate fragments are first allocated and fixed with miniplates and screws. Small fragments that are impractical to fix are removed to prevent dislocation, infection, and necrosis. Subsequently, a load-bearing reconstruction plate is placed on the mandibular base to maintain the mandibular block, particularly when there is a discontinuity of the bone (Fig. 47.11a–c). If bone segments are missing and no obvious signs of infection (e.g., contamination with foreign material) are apparent, I recommend immediate bone augmentation with autologous transplants from the iliac crest. Preconditions for immediate bone augmentation are that the transplants can be fixed effectively and that sufficient soft tissue closure can be achieved. Intravenous antibiotics (amoxicillin and clavulanic acid) are administered three times daily for 5 days to prevent transplant infection. If the preconditions for primary augmentation are inappropriate, the augmentation is performed in a second operation after wound healing is complete. Massive bone loss requires bone augmentation and jaw reconstruction with microvascular transplants. To counteract the effect of the lack of bone coverage, osteocutaneous grafts are the transplants of choice. Modern three-dimensional planning tools can anticipate the amount of bone loss via CT and design custom-made bony transplants virtually. Corresponding cutting guides for bony osteotomy of the recipient and of the donor site are then manufactured by industrial partners (see Fig. 47.11b–f). As previously mentioned, antibiotic therapy is necessary for 5 to 7 days for comminuted fractures. Bone necrosis resulting from small fragments can be avoided if surgical therapy is carried out as described. Finding and removing bullets and splinters can be challenging; intraoperative navigation is a helpful tool for simplifying the retrieval of foreign materials. Plate exposure and infection typically result from the lack of soft tissue coverage of the bone and osteosynthesis material. Effective cleansing and appropriate care of the exposed plate might prolong the time until removal is necessary. Early removal of plates is possible from 6 weeks after osteosynthesis, often with no compromise to the result. If denuded bone cannot be covered adequately, pedicled soft tissue grafts are harvested to cover the hard tissue. Curettage and planning of bony edges are essential; in complex cases, adjacent teeth are extracted to enhance soft tissue coverage. Nonunion typically results from infection or a lack of bony stabilization. Pseudarthrosis is a possible result. Two strategies are available: 1. If pseudarthrosis is stable and the patient appears satisfied with the situation, no further surgery is recommended. 2. If major mobility occurs between the fragments, restabilization with a taller osteosynthesis plate and a bone graft is indicated.
47
Fractures of the Jaws
Anatomy of the Jaws and Types of Fractures
Aims of Jaw Fracture Reconstruction
Unfavorable Results and Complications in Jaw Fracture Reconstruction
Therapeutic Principles
Maxilla Fractures
Le Fort I Fracture
Malposition, Nonocclusion, and Change of Facial Profile
Avoidance and Correction
 Malposition and nonocclusion
Malposition and nonocclusion
 Facial profile changes
Facial profile changes
 Transverse malposition and nonocclusion
Transverse malposition and nonocclusion
 Transverse expansion of maxilla
Transverse expansion of maxilla
 Laceration of palatal soft tissue
Laceration of palatal soft tissue
 Oronasal communication
Oronasal communication
 Infection
Infection
 Bone graft loss
Bone graft loss
 Nonunion
Nonunion
 Persistent infection
Persistent infection
 Movable fractured bone segments
Movable fractured bone segments
 Necrosis
Necrosis
 Infection of surrounding soft tissue
Infection of surrounding soft tissue
 Soft tissue shortage
Soft tissue shortage
 Salivary fistula
Salivary fistula
 Infection, pain, and scarring leading to secondary surgery
Infection, pain, and scarring leading to secondary surgery
Sagittal Fractures of the Maxilla
Avoiding Complications and Surgical Solutions
Mandibular Fractures
Fractures of the Mandibular Body, Angle, and Symphysis
Avoiding Complications
Managing Complications
Condylar Process Fractures
Unfavorable Results in Condylar Process Fracture Treatment
Algorithm for Avoiding Complications
Diagnostics
Treatment
 Patients with alcohol abuse
Patients with alcohol abuse
 Patients with epilepsy
Patients with epilepsy
Surgical Approach
Osteosynthesis
Comminuted Fractures
Avoiding Complications
 Contaminated foreign bodies such as bullets or splinters
Contaminated foreign bodies such as bullets or splinters
 Inadequate soft tissue closure over denuded bone
Inadequate soft tissue closure over denuded bone
 Loosened and movable bone fragments
Loosened and movable bone fragments
 Loosened or dislocated teeth
Loosened or dislocated teeth
 Absent or insufficient antibiotic therapy
Absent or insufficient antibiotic therapy
Anatomic Repositioning, Osteosynthesis, and Discontinuity of Bone
Infection
Nonunion and Malocclusion
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine