8 Fractures and dislocations of the wrist and distal radius
Synopsis
 The treatment of scaphoid fractures requires an understanding of the vascular anatomy and judicious treatment based on the fracture pattern in order to assure proper healing.
The treatment of scaphoid fractures requires an understanding of the vascular anatomy and judicious treatment based on the fracture pattern in order to assure proper healing.
 The dissociation of the scaphoid and lunate bones breaks the link in the proximal carpal row, causing a predictable pattern of carpal bone misalignment that has major consequences for the management of acute and chronic conditions.
The dissociation of the scaphoid and lunate bones breaks the link in the proximal carpal row, causing a predictable pattern of carpal bone misalignment that has major consequences for the management of acute and chronic conditions.
 The dislocation of carpal bones requires a keen eye to determine the instability pattern on wrist radiographs. This is necessary in order to diagnose and treat injury patterns associated with this condition.
The dislocation of carpal bones requires a keen eye to determine the instability pattern on wrist radiographs. This is necessary in order to diagnose and treat injury patterns associated with this condition.
 Understanding the treatment of wrist injuries requires the appreciation of carpal bone alignment seen in the AP, oblique, and lateral X-ray views. Subtleties that may provide clues for ligament disruption may not always be easy to discern on the radiograph.
Understanding the treatment of wrist injuries requires the appreciation of carpal bone alignment seen in the AP, oblique, and lateral X-ray views. Subtleties that may provide clues for ligament disruption may not always be easy to discern on the radiograph.
 The treatment of distal radius fractures (DRFs) challenges the surgeon to apply appropriate fixation techniques to not only restore normal radius anatomy, but also to recreate the normal architecture between the radius and the carpal bones, as well as between the radius and the ulna.
The treatment of distal radius fractures (DRFs) challenges the surgeon to apply appropriate fixation techniques to not only restore normal radius anatomy, but also to recreate the normal architecture between the radius and the carpal bones, as well as between the radius and the ulna.
 The treatment of DRFs now emphasizes more aggressive surgical treatment in order to restore the anatomy and promote early functional use of the hand.
The treatment of DRFs now emphasizes more aggressive surgical treatment in order to restore the anatomy and promote early functional use of the hand.
 Fractures and dislocations of the wrist and distal radius consist of a fascinating array of injury patterns and kinematic complexities that challenge even the most seasoned physician.
Fractures and dislocations of the wrist and distal radius consist of a fascinating array of injury patterns and kinematic complexities that challenge even the most seasoned physician.
Introduction
The epidemiology of wrist fractures has been investigated in detail. Nearly 1.5 million hand and wrist fractures are estimated to occur in the United States, annually.1 These account for 1.5% of all emergency department visits. Of these, approximately 208 000 are carpal fractures. The scaphoid bone is the carpal bone most commonly fractured; it accounts for 60–85% of carpal fractures.2 Incidence estimates range from 4.3/10 000 person-years in Norway3 to 12.1/10 000 person-years in the US military population.4 The highest incidence is found in the 20–24-year-old age group.4
Distal radius fractures are the most common upper extremity fracture; the annual incidence is estimated at 643 000 fractures per year in the United States.1 When the incidence is examined by age, there are two distinct peaks identified (Fig. 8.1). The greatest “spike” on the chart is in the 5–14-year-old group (55.7/10 000 person-years), and there is an additional peak in the elderly 75–84-year-old group (35.2/10 000 person-years).
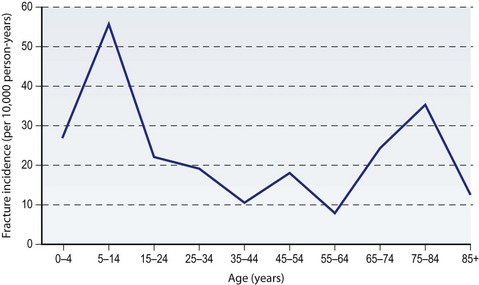
Fig. 8.1 Age-related variation in radius/ulna fracture incidence.
(Data from Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg (Am) 2001; 26(5):908–915.)
Although a common injury, these fractures should never be treated casually. There is significant potential for patient disability if these injuries are not managed with great care and expertise. Khan and Giddins’ review of hand and wrist surgery negligence claims in the UK from 1995–2001 revealed that wrist fracture was the most common condition in which negligence was alleged, comprising 48% of claims.5
History
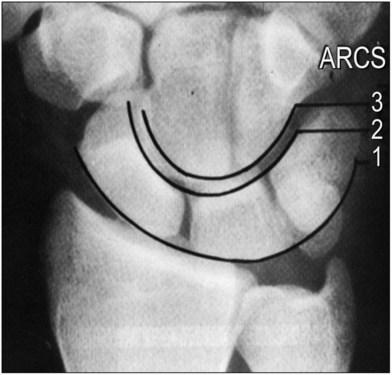
The carpal bones are named for their shapes. For example, the scaphoid resembles a boat, whereas the lunate resembles the crescent moon. However, these bones were not described until the 1500s, when Andreas Vesalius first identified the eight carpal bones. Before then, drawings of the hand connected the metacarpals directly to the distal radius, with no mention of wrist anatomy. The names of the carpal bones were not solidified until 1955 when Nomina Anatomica established the official nomenclature for the carpal bones that we use today (Fig. 8.2).6 Perhaps more useful than nomenclature are the many classification systems that were used to organize the wrist anatomy into discreet packages. The earliest classification separates the wrist joint into two rows, consisting of the distal carpal row and the proximal carpal row. The carpal anatomy is not only distinguishable by rows, but also separated by columnar divisions. Particularly important is the alignment of the carpal bones. Gilula’s lines – the arcs formed by (1) the proximal and (2) the distal articular surface of the proximal row of carpal bones, as well as (3) the proximal articular surface of the distal row of carpal bones – are used to determine carpal alignment (Fig. 8.3). Increased joint space or deviation of carpal bones from these lines is indicative of wrist instability.7 It is important to note that because of the complex arrangement of the eight bones in the wrist, the pisiform is sometimes considered a sesamoid that is not part of the carpal bones in some classification systems.
The treatment of DRFs is privy to a fascinating 200-year experience. As is often paraphrased from Colles (the Irish surgeon who recognized the common patterns of extra-articular DRFs in the elderly without the assistance of X-rays), even patients treated with simple external anatomic reduction, “have all recovered without the smallest defect or deformity of the limb.”8 Though there is some truth to this 200-year-old statement, the expectations for recovery at that time were quite low because the technology to restore anatomic reduction was unavailable. Nevertheless, it is still often assumed that elderly patients with DRFs will have no functional limitations even with severe malalignments of the distal radius. However in recent years it has been recognized that restoration of the anatomic alignment of the distal radius is more likely to achieve better outcomes than less precise anatomic reduction methods. The improvement in internal fixation techniques has been heavily promoted by AO (Arbeitsgemeinschaft fur Osteosynthesefragen or Association for the Study of Internal Fixation, a Swiss organization started in the late 1950s for promoting rigid internal fixation techniques for fractures). These treatment options include the use of K-wires, external fixation, and more recently, a variety of implant technologies that are either placed dorsally or volarly on the radius for even more elegant fragment-specific fixations, where small implants are used to capture fractured columns within the distal radius for assured anatomic reduction. The most important advancement in the treatment of DRFs is the use of volar locking plating techniques, for which low profile plates are placed over the volar distal radius in order to treat a variety of extra-articular and intra-articular fractures regardless of whether the fracture occurs volarly or dorsally.
Understanding the treatment of the wrist as well as the distal radius, also requires one to be familiar with a variety of eponyms. Although many textbooks discourage the use of eponyms, the eponyms for DRFs display a clear image of predictable injury patterns to convey precise information regarding the type of injury sustained. The major eponyms for distal radius fractures are: dorsal and volar Barton’s fractures (a shearing type fracture involving the a volar or dorsal fragment of the articular surface) (Fig. 8.4A); Chauffeur fractures (a fracture involving the radial styloid); Colles fractures (the most common fracture pattern in the elderly in which the fracture fragment is displaced dorsally) (Fig. 8.4B); Galeazzi fractures (a mid-shaft radius fracture associated with distal radioulnar joint disruption) (Fig. 8.4C); and Smith fractures (also called the reverse Colles in which the fracture fragment is displaced volarly). For some cases, these eponyms may help in selecting a treatment modality.9
Basic science/disease process
Anatomy
Normal anatomy of the wrist is covered in detail in Volume VI, Section 1, Chapter 1 of this textbook. However, there are a few points that merit emphasis in this chapter with regard to these injuries.
The vascularity of the scaphoid bone bears particular consideration. The scaphoid bone has a single dominant vascular pedicle that enters from the distal pole of the bone. Therefore, the proximal pole relies wholly on the intramedullary blood supply for survival. It is for this reason that proximal pole fractures typically take longer to heal, and have increased incidence of nonunion. Furthermore, in cases of nonunion, the proximal pole is susceptible to avascular necrosis, which further complicates these injuries.10,11
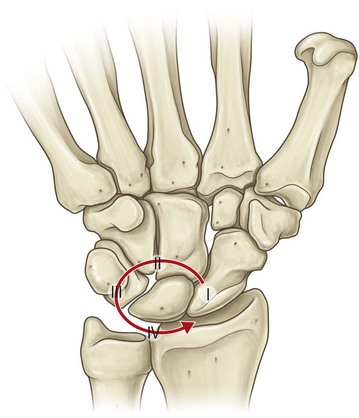
The strength of the wrist ligaments helps determine the injury patterns observed. For example, the very strong short radiolunate ligament tends to resist lunate dislocation, retaining the lunate in its fossa on the distal radius in all but the most severe traumas. Instead, the surrounding carpal bones typically dislocate away from the lunate. This perilunate pattern of injury (Fig. 8.5) involves: (1) rupture of the scapholunate interosseous ligament; (2) capsular disruption through the space of Poirier, an area of inherent weakness of the volar capsule between the lunate and capitate, and (3) rupture of the lunotriquetral interosseous ligament. If the dislocated carpus rebounds, then the capitate will settle into the lunate fossa, and the lunate rotates volarly, hinged on the short radiolunate ligament.12,13
The extensor pollicis longus (EPL) is the tendon most likely to rupture after a DRF. The etiology of this appears to be related to interruption of the tendon’s nutritional supply, leading to attritional rupture. This most commonly occurs at Lister tubercle where there is a natural watershed area of this tendon’s intrinsic blood supply. If the extrinsic (diffusion-mediated) nutritional supply is also interrupted by fracture callus, fracture displacement, or swelling from edema or hematoma, rupture of the EPL can occur.14
Biomechanics
The biomechanics of the hand and wrist were reviewed in Volume VI, Section 1, Chapter 1, but there are a few points to revisit here.
Disruption of the normal linkages between the bones of the wrist – whether due to ligamentous rupture or fracture – can lead to carpal instability. The concept of carpal instability has evolved rapidly over the past 50 years, as we have learned more about the ways in which the wrist bones move (kinematics) and transfer a load (kinetics). In the modern era, instability has a very specific definition; a wrist is unstable if it is unable to transfer functional loads without sudden changes in stress on the articular cartilage and if it is unable to maintain motion throughout its range without sudden alterations of intercarpal alignment.15
Carpal instability has been thoughtfully classified into four major patterns (Table 8.1). Carpal instability dissociative (CID) occurs when there is a disruption within or between the bones of the same carpal row. Carpal instability non-dissociative (CIND) refers to a disruption between the distal radius and the proximal carpal row, or between the proximal and distal carpal rows. When a combination of elements of both CID and CIND exist, it is referred to as carpal instability complex (CIC). Finally, when the instability is an adaptive response to a problem proximal or distal to the wrist itself, it is called carpal instability adaptive (CIA).16
Table 8.1 Patterns of carpal instability
| Pattern | Definition | Example(s) |
|---|---|---|
| Carpal instability dissociative (CID) | Disruption within or between bones of the same carpal row | Scapholunate dissociation; Scaphoid nonunion |
| Carpal instability nondissociative (CIND) | Disruption at the radiocarpal or midcarpal joints, with intact proximal and distal rows | Midcarpal instability |
| Carpal instability complex (CIC) | Derangement both within and between carpal rows (CID plus CIND) | Perilunate dislocation with ulnar translation |
| Carpal instability adaptive (CIA) | Instability due to injury proximal or distal to wrist | Distal radius malunion |
Source: Data from Gilula LA, Mann FA, Dobyns JH, et al. Wrist: terminology and definitions. J Bone Joint Surg Am 2002;84-A(Suppl 1):1–73.
Because of the scaphoid’s natural tendency to flex when loaded, delayed treatment of comminuted fractures of the scaphoid waist tend to result in the so-called “humpback deformity” (Fig. 8.6). This term describes the shape of the scaphoid as seen on lateral tomograms, reflecting malunion of the bone with an abnormally acute angle between the proximal and distal poles of the scaphoid.17
Diagnosis/patient presentation
Physical examination
Before assessing the range of motion or performing any provocative testing, it is important to review the radiographs of the extremity to rule out any unstable fractures that might be displaced or otherwise worsened by vigorous physical examination. While assessing the patient’s active and passive range of motion, palpation over the joints being moved can yield other useful information about crepitus, clicks, or clunks in the wrist. A complete examination should also include assessment of grip strength, pinch strength, and sensibility. It is particularly important to detect median neuropathy in wrist injury patients, because acute carpal tunnel syndrome may require treatment.18 Provocative testing of specific intrinsic ligaments of the wrist can be valuable in reaching a diagnosis, but should be conducted with caution when unstable fractures are present to avoid unwanted fracture displacement.
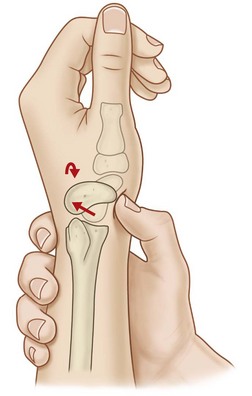
The Watson scaphoid shift test stresses the scapholunate ligament to detect injury or instability (Fig. 8.7). The examiner applies pressure (typically with the thumb) over the distal scaphoid tubercle, while moving the patient’s wrist from ulnar to radial deviation.19 In ulnar deviation the scaphoid is extended, whereas in radial deviation it is flexed. Thus, in the intact wrist, the scaphoid’s ligamentous attachments resist subluxation during this maneuver. However, in cases of scapholunate dissociation, the scaphoid may be forced dorsally out of the scaphoid fossa into a painful position for the patient. Upon releasing pressure, a clunk may be heard indicating the self-reduction of the scaphoid back over the dorsal rim of the radius. A painful Watson test in the absence of an obvious clunk may be a sign of scapholunate ligament damage without complete disruption of the ligament.
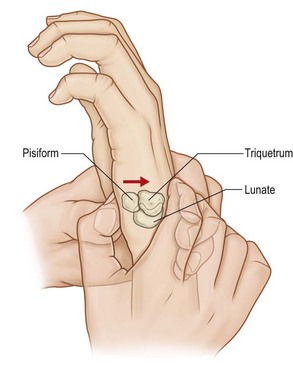
The lunotriquetral interosseous ligament can be assessed by the Kleinman shear test (Fig. 8.8). The examiner grasps the patient’s wrist in one hand, specifically applying stabilizing pressure over the lunate, which is palpable dorsally just beneath the fourth extensor compartment tendons. With the other hand, the examiner applies dorsally directed pressure over the pisiform, which applies a shear force directed across the lunotriquetral articulation. Laxity can be assessed by further grasping the pisiform/triquetral unit and moving it both palmarly and dorsally in a “shucking” type maneuver. This latter is referred to as the lunotriquetral ballottement test.20 Pain and/or instability may indicate injury or disruption of the lunotriquetral ligament.
Diagnostic tests
At a minimum, assessment of wrist injuries should include four radiographs: posteroanterior (PA), oblique, lateral, and PA ulnar deviation. The ulnar deviation view is particularly important in detecting scaphoid injuries. Another helpful view for detecting dynamic instability of the scapholunate ligament is the clenched fist view. When making a tight fist, load is placed across the wrist, and the capitate is driven toward the scapholunate articulation, which will make scapholunate ligament laxity or rupture more evident. To increase the accuracy of the diagnosis, both anteroposterior (AP) and PA stress views should be considered.21
Cross-sectional imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI) are also used routinely to investigate wrist injuries. CT is an X-ray-based modality, and as such it is best for assessing complex fracture-dislocation patterns. CT is also better than MRI at determining osseous healing across a fracture site. On the other hand, MRI is the preferred modality for assessing nonosseous structures. MRI technology continues to evolve, and modern machines can detect even very small ligamentous injuries.22 When the modalities of MRI and arthrography are combined, even small perforations in the interosseous ligaments can be detected.
The bones of the wrist are linked by a complex system of intrinsic and extrinsic ligaments (Fig. 8.9). The type of injury sustained in patients presenting with wrist pain may be discerned by soliciting a well defined history. For example, a patient who works with heavy machinery who received a torque-type injury several months ago and continues to have wrist pain most likely sustained some type of ligamentous injury to the wrist. An X-ray should be able to determine if this ligamentous injury is between the carpal bones, and if it is typical of a dorsal intercalated segment instability (DISI) or volar intercalated segment instability (VISI) deformity (Fig. 8.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree