CHAPTER 77 Fractional resurfacing
History
Non-ablative fractional photothermolysis was first introduced in 2005 with the introduction of the 1550-nm erbium-doped fiber laser (Reliant Technologies, Mountain View, CA). Initially the laser was approved for the soft tissue coagulation application, based largely on early studies of forearm tissue. In 2005 Khan et al. reported on the use of the first fractional resurfacing device, a 1550-nm erbium-doped fiber prototype laser system that produced microscopic columns of thermal injury surrounded by intact tissue using a handpiece that scanned across the skin up to 8 cm/second while delivering the microarray pattern to the skin. These microscopic treatment zones (MTZs) range in diameter from 70 to 100 micrometer in diameter and 250 to 800 micrometer in depth and are produced by varying the depth of the focused beam. Tissue in these coagulated zones is not vaporized and the epidermis and stratum corneum are left intact leaving the skin erythematous, edematous, but without evidence of wounding. The device is FDA cleared for the treatment of periorbital rhytids, pigmentary alteration, melasma, skin resurfacing, and surgical scars.
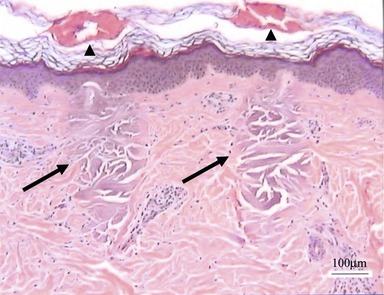
The handpiece of the fractionated laser makes direct contact with the skin’s surface and uses an intelligent optical tracking system to deliver an even array of MTZs. These are columns of tissue coagulation that show no loss in the integrity of the overlying stratum corneum (Fig. 77.1). The incipient wound healing cascade and inflammatory response in which heat shock protein-70 is a central player, initiates a number of incompletely understood events that leads to increase in collagen synthesis and collagen reorganization. Healing also involves the extrusion of damaged epidermal components, termed microepidermal necrotic debris (MEND), which clinically could be observed as a superficial exfoliation following treatment that imparts a fine rough sand paper-like feel to the skin and is associated with a mild bronzing color of the skin in the areas of treatment. This clinically translates into the observed improvement in photodamage, including softening of rhytids, tightening of pore ostia, improvement in dyschromia, and a general textural smoothening of the skin.
Physical evaluation
The cosmetic consultation visit should focus on the following:
• Complete past medical and surgical procedures including complication in the postprocedural periods.
• History of hypertrophic scarring and/or keloid formation. While there is a low risk of scarring from fractional resurfacing, a positive history of hypertrophic scarring and/or keloid formation is a marker of a perturbed wounding response and signal that caution should be exercised in treating these patients. Closer follow-up and possibly less aggressive initial treatments should be undertaken until an assessment of an individual patient’s response to therapy can be made.
• History of herpes labialis and/or HSV infections elsewhere, use of antivirals and antibiotics in the past, and allergies to these are significant. Patients with active bacterial and viral infections should delay fractional resurfacing treatments until these issues have resolved. Routine use of prophylactic antivirals is recommended for three days starting on the day of treatment.
• History of isotretinoin use over last 6 months. These patients should be excluded from treatment because of a theoretical increased risk of scarring.
• History of smoking. Patients who smoke generally heal less favorably.
• Plans for UV exposure should be gauged before the procedure as UV avoidance is necessary immediately following treatments and during the healing period.
• Thorough physical exam noting scars, dyschromia, rhytids, and skin phototype are important considerations in selection of treatment settings for particular applications.
• Photography is useful for patient feedback and part of the medical record for later reference.