Forequarter Amputation
Keila E. Torres
Kelly K. Hunt
Raphael E. Pollock
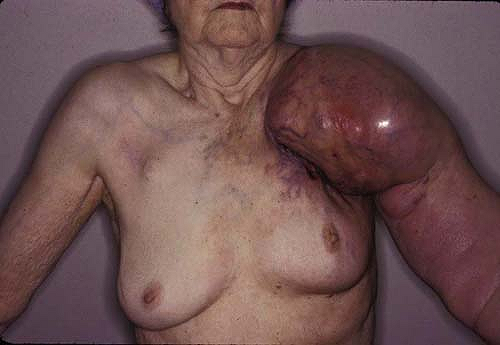
Amputation is one of the most ancient of all surgical procedures. Because of the lack of hemostatic techniques and antibiotic therapy, amputation was previously associated with a high mortality rate. The earliest report on the use of surgical forequarter amputation, or interscapulothoracic amputation, was published by Cuming in 1829 (1). Unfortunately, the patient died of gangrene a few days following the procedure. Because of the advances in regional and systemic therapies, radical amputation procedures are rarely performed. Forequarter amputation is performed almost exclusively for tumors of the shoulder girdle or surrounding soft tissues that invade the glenohumeral joint, the brachial plexus, or the axillary vasculature, making limb salvage or shoulder disarticulation unfeasible. This radical operation has been selectively utilized in the treatment of recurrent breast cancer, specifically when there is disease in the axilla (2). Recurrent tumor in the axilla with invasion into the brachial plexus and axillary vessels can lead to significant morbidity secondary to pain, lymphedema, limb dysfunction, and ulceration. In some instances, palliative forequarter amputation has provided effective pain relief for selected patients with unresectable metastatic disease to the axilla and shoulder girdle in whom radiation therapy and/or chemotherapy have not been effective (3).
Forequarter amputation indications are as follows:
Detailed clinical and pathologic data should be obtained in the planning phase. A core needle biopsy or incisional biopsy is recommended to confirm the diagnosis prior to any surgical intervention (4). The placement of the biopsy site should be chosen carefully, as it will need to be included in the formal resection. High-quality, contrast-enhanced computed tomography (CT) scanning can define all necessary anatomical details that will be
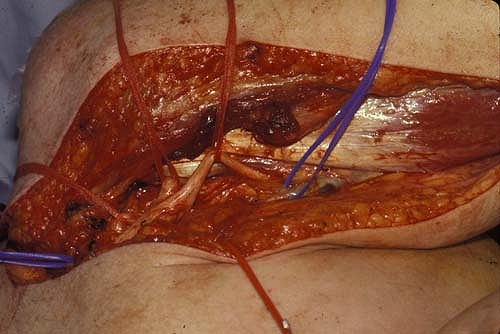
important in determining resectability (5,6). Magnetic resonance imaging (MRI) has the advantage of providing a more detailed assessment of individual muscle involvement and extent of brachial plexus involvement in selected patients (6). In equivocal cases a local exploration with intra-operative biopsies may be needed (Fig. 23.3).
important in determining resectability (5,6). Magnetic resonance imaging (MRI) has the advantage of providing a more detailed assessment of individual muscle involvement and extent of brachial plexus involvement in selected patients (6). In equivocal cases a local exploration with intra-operative biopsies may be needed (Fig. 23.3).
The nutritional status and immunocompetence of the patient should be assessed prior to operative intervention. Malnourished or immunocompromised patients will have markedly increased rates of perioperative complications that may prevent a successful recovery. The forequarter amputation is a radical procedure that will result in a hypermetabolic state postoperatively. Significant medical comorbidities or any active infection should be addressed prior to surgery. Depending on the extent of the tumor,
this procedure can involve significant blood loss and plans for perioperative transfusion should be made.
this procedure can involve significant blood loss and plans for perioperative transfusion should be made.
The need for additional skin and soft-tissue coverage of the amputation site should be considered preoperatively. When the tumor involves a considerable portion of the medial aspect of the axillary skin and soft tissue, the resection defect following forequarter amputation will often necessitate the use of split thickness skin grafts or myocutaneous flaps for wound closure. A fasciocutaneous deltoid flap can be utilized when a proximal but medial tumor necessitates more skin and soft-tissue resection near the chest wall. If the resection necessitates removal of more than two ribs, coverage of the defect and stabilization of the chest wall will be needed and consultation with a plastic and reconstructive surgeon should be obtained.
Preoperative assessment includes:
biopsy to confirm diagnosis,
proper imaging of the proximal vasculature and neural plexus for surgical planning, and
optimization of the patient’s medical and nutritional status.
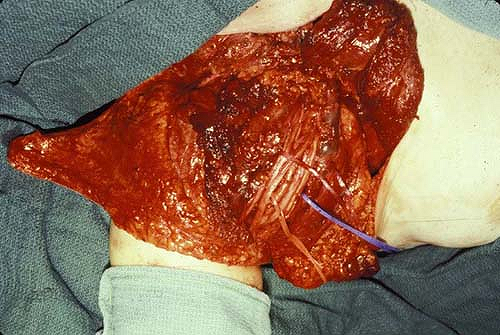
Forequarter amputation removes the entire upper extremity in the interval between the scapula and the chest wall (7,8,9). Resection of the chest wall may also be required (Fig. 23.4).
Three approaches to the forequarter amputation have been described:
Anterior approach (Berger)
Posterior approach (Littlewood)
Combination of the anterior and posterior approaches
Positioning
The patient should be placed in a lateral decubitus position with the affected side up and secured to the operating table at several points. The affected shoulder, axillary region, and upper extremity should be prepped with sterile solution and draped with a
wide operative field. The upper extremity should be prepped free and covered with a stocking so that it can be manipulated to facilitate exposure during the procedure.
wide operative field. The upper extremity should be prepped free and covered with a stocking so that it can be manipulated to facilitate exposure during the procedure.
Operative Technique for the Posterior Approach
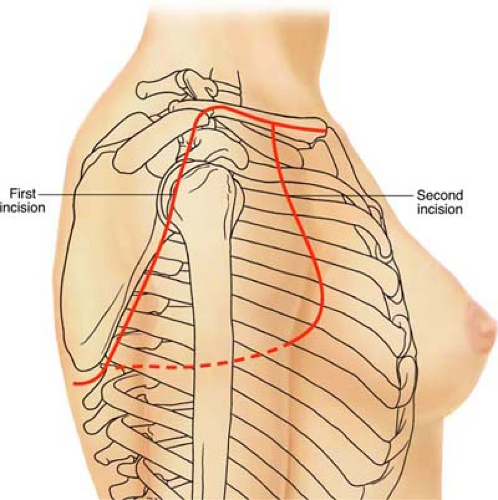
The posterior approach to the forequarter amputation requires two incisions: one posterior (cervicoscapular) and one anterior (pectoroaxillary) (Fig. 23.5). If a fasciocutaneous
deltoid flap is required for closure of the wound, the incision will extend out over the shoulder following the outline of the deltoid muscle just distal to its insertion on the humerus (Fig. 23.6).
deltoid flap is required for closure of the wound, the incision will extend out over the shoulder following the outline of the deltoid muscle just distal to its insertion on the humerus (Fig. 23.6).
The posterior incision is initiated at the medial end of the clavicle and extended laterally for the entire length of the bone. The incision is then extended to the acromion and the lateral border of the scapula to the inferior angle of the scapula.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree