7 Forehead rejuvenation
Synopsis
 Detailed knowledge of forehead anatomy is the basis for rejuvenation strategies of the forehead region.
Detailed knowledge of forehead anatomy is the basis for rejuvenation strategies of the forehead region.
 Eyebrow position is the net result of forces which depress the brow, forces which raise the brow and the structures which tether the eyebrow in place.
Eyebrow position is the net result of forces which depress the brow, forces which raise the brow and the structures which tether the eyebrow in place.
 Brow depression is caused by glabellar frown muscles, the orbicularis and gravity. Frontalis is the only effective brow elevator.
Brow depression is caused by glabellar frown muscles, the orbicularis and gravity. Frontalis is the only effective brow elevator.
 Attractiveness of the periorbital region is intimately related to eyebrow shape and eyebrow position as it relates to the upper eyelid and the upper lid sulcus.
Attractiveness of the periorbital region is intimately related to eyebrow shape and eyebrow position as it relates to the upper eyelid and the upper lid sulcus.
 Aging causes enlargement of the orbital aperture as well as changes in eyebrow shape. In a subset of individuals there is ptosis of the entire forehead complex.
Aging causes enlargement of the orbital aperture as well as changes in eyebrow shape. In a subset of individuals there is ptosis of the entire forehead complex.
 Key elements of forehead rejuvenation are the attenuation of frown muscle action and the repositioning of ptotic eyebrow elements. The lateral eyebrow is often the only portion requiring elevation.
Key elements of forehead rejuvenation are the attenuation of frown muscle action and the repositioning of ptotic eyebrow elements. The lateral eyebrow is often the only portion requiring elevation.
 Forehead rejuvenation can be accomplished using a combination of surgical and non-surgical techniques.
Forehead rejuvenation can be accomplished using a combination of surgical and non-surgical techniques.
 If surgical elevation of the brow complex fails early, it is usually due to lack of soft tissue release. If it fails late, is usually due to failure of fixation.
If surgical elevation of the brow complex fails early, it is usually due to lack of soft tissue release. If it fails late, is usually due to failure of fixation.
 Many methods of soft tissue fixation and bony fixation have been proven effective in maintaining the position of the surgically elevated brow.
Many methods of soft tissue fixation and bony fixation have been proven effective in maintaining the position of the surgically elevated brow.
Introduction
In the younger individual, aesthetic alteration of the forehead is generally limited to the nonsurgical alleviation of glabellar frown lines and lateral orbital wrinkles. These issues are discussed in Chapters 3 and 4. Occasionally, surgery is indicated to change the basic shape of a youthful eyebrow. In the older individual, the forehead typically becomes ptotic laterally, while in the orbit, there is a relative loss of orbital fat together with an accumulation of loose eyelid skin. Understanding the interplay between these complex anatomical changes is critical in choosing an appropriate surgical strategy to rejuvenate the upper third of the face.
History
The history of aesthetic brow surgery was thoroughly reviewed by Paul in 2001.1
The first description of brow elevation surgery was a publication by the French surgeon Passot in 1919.2 His technique involved the removal of multiple small skin ellipses, positioning scars in the forehead crease lines and at the frontal hairline. In 1926, Hunt described what appears to have been a full anterior hairline incision for brow lifting access.3 In 1931, Lexer published a combined forehead and open brow lift with a hairline incision,4 and in 1933, Claoue published a similar extensive approach.5 Interestingly, forehead lifting then fell into disfavor for several decades until 1962 when Gonzalez-Ulloa published in the English literature an open coronal brow lift combined with facelift.6 Shortly thereafter, in Brazil, Vinas presented (1965)7 and subsequently described (1976)8 his advanced concepts of brow elevation. He suggested making a concerted effort to elevate the lateral portion of the brow. He also described a local method of direct brow lifting for certain patients. In 1984, Papillon and colleagues presented a subcutaneous dissection plane from the anterior hairline approach.9 In 1989, Paul described a transblepharoplasty approach.10
The original description of endoscopic brow lifting is attributed to two surgeons, Isse and Vasconez, both of whom presented their method at different venues in 1992.11,12 The first publication of this method was by Chajchir in 1993.13
In 1996, Knize published his “limited incision forehead lift”,14 using a short temple incision without endoscopic assist.
By 2003, a reduction in the number of endoscopic brow lifts being done was documented due to uncertainty over the stability of endoscopic brow lifting.15 In the first part of the 21st century, other methods appeared to deal with lateral brow relapse.16 Numerous reports demonstrated the success of endoscopic brow lifting using measurements from the brow to the pupil.17–21
Anatomy
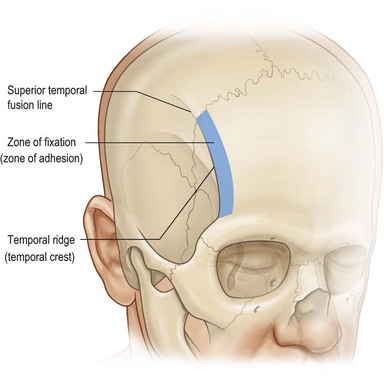
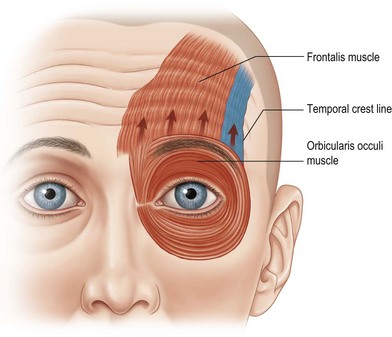
The frontal bone is crossed laterally by a curved ridge called the temporal crest (also called the temporal ridge or the superior temporal fusion line of the skull). This is a palpable landmark which separates the temporal fossa and the origin of the temporalis muscle from the forehead portion of the frontal bone (Fig. 7.1). It also marks a change in nomenclature as tissue planes transition from lateral to medial. The deep temporal fascia covering the temporalis muscle attaches along the temporal ridge and continues medially as the periosteum which covers the frontal bone. Similarly, the superficial temporal fascia (also known as the temporal parietal fascia) continues medially as the galea aponeurotica which encompasses the frontalis muscle.
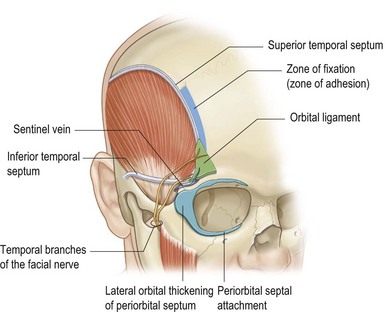
The surgical significance of the temporal crest line is that all fascial layers are tethered to bone in a band approximately 5 mm wide immediately medial to the palpable ridge. This has been called the zone of fixation.22,23 Where this zone approaches the orbital rim at its inferior end, the fascial attachment widens and becomes more dense, forming the orbital ligament (Fig. 7.2). All fascial attachments in this region must be released from bone when a full thickness forehead flap is being repositioned.
Some fascial structures in this area have been named by different authors, generating some confusion. The superior temporal septum24 and the zone of adhesion16 are alternate terms used to describe the zone of fixation. The temporal ligamentous adhesion24 describes the lower portion of the zone of fixation and the orbital ligament. The inferior temporal septum24 and the orbicularis-temporal ligament25 both describe the criss-crossing white fibers which loosely attach the superficial to the deep temporal fascia.
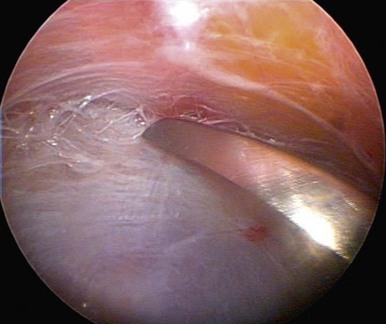
The inferior temporal septum is a useful landmark during endoscopic dissection from above, because it separates the safe upper zone containing no vital structures from the lower zone where facial nerve branches travel in the cavity’s roof. The medial zygomatic temporal vein (sentinel vein) is also present in this lower zone, adjacent to the lateral orbital rim. The temporal branches pass immediately superior to this vein (Figs 7.3, 7.4).
Galea
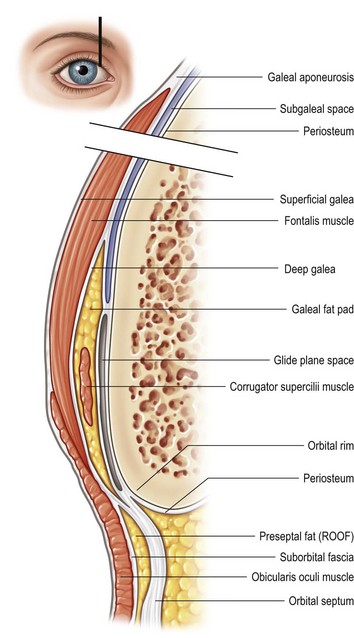
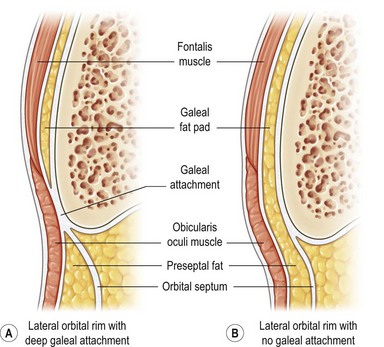
Knize has described galeal anatomy in detail.26 In the forehead, the galea aponeurotica splits into a superficial and deep layer encompassing the frontalis muscle (Fig. 7.5). Inferiorly, the deep galea layer separates further into three separate layers: one layer immediately deep to the frontalis forming the roof of the galeal fat pad, a second layer forming the floor of the galeal fat pad but not adherent to bone, and a third layer adherent to periosteum. The two deepest layers define the glide plane space between the galeal fat pad and the skull. Inferiorly, the septum orbitale divides orbital fat from PreSeptal fat (also known as retro orbicularis oculi fat or ROOF).
When the eyebrow is raised by frontalis contraction, the soft tissue slides over the glide plane space. The galeal fat pad extends across the entire width of the lower 2 cm of the forehead; medially it surrounds the supra orbital and supra trochlear nerves as well as portions of the frown musculature. The galeal fat pad is separated from the preseptal fat (ROOF) by a reflected layer of galea. Laterally, this separation is thought to be variable, with some individuals having a continuous layer of fat from galeal fat pad to the preseptal fat (Fig. 7.6).26
Muscle
Eyebrow level is the result of a balance between the muscular forces which elevate the brow, the muscular forces which depress the brow, and the universal depressor: gravity (Fig. 7.7).
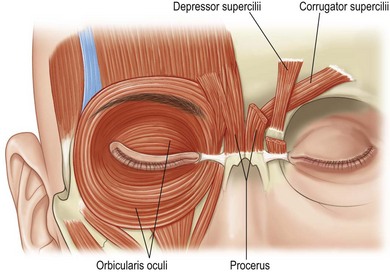
Brow depressors in the glabella originate from bone medially, inserting into soft tissue. The procerus runs vertically, the depressor supercilii and orbiculars run obliquely, and the corrugator mostly runs transversely. The transverse corrugator supercilii is the largest and most powerful of these muscles. It originates from the orbital rim at its most supero-medial corner, with the large transverse head later passing through galeal fat becoming progressively more superficial until it interdigitates with the orbicularis and frontalis at a skin dimple which is visible when the patient frowns.27
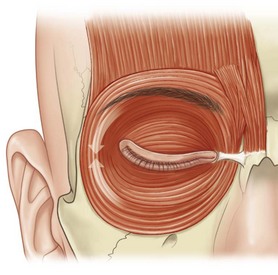
The orbicularis encircles the orbit acting like a sphincter. Medially and laterally the orbicularis fibers run vertically and act to depress brow level. Laterally, orbicularis is the only muscle which depresses brow position (Figs 7.8, 7.9).
Sensory nerves
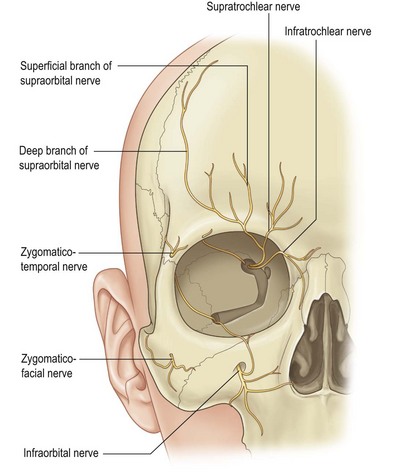
Innervation to the upper periorbita is supplied by the supraorbita and supratrochlear nerves, as well as two lesser nerves, the infratrochlear, and zygomaticotemporal (Fig. 7.10).
The supraorbital nerve exits the superior orbit either through a notch in the rim, or through a foramen superior to the rim. Much variation occurs with foramina present about 20% of the time.28 The location of the notch or foramen is between 16 and 42 mm from the midline, with a mean of 25 mm. A useful landmark for this is a palpable notch, or failing that, the mid-papillary line. When a foramen is present, it has been found as far as 19 mm above the rim. Because of such variation, blind dissection from above should be discontinued at least 2 cm above the orbital rim.
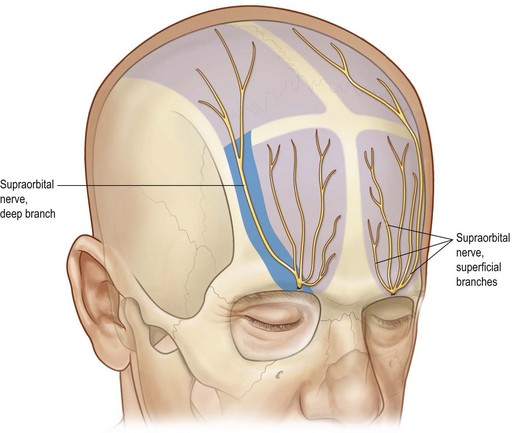
It is a double branch approximately 60% of the time.29 An important fact during endoscopic brow lifting is that the deep branch runs in a 1 cm wide band, which is between 5 mm and 15 mm medial to the palpable temporal ridge (Fig. 7.11).
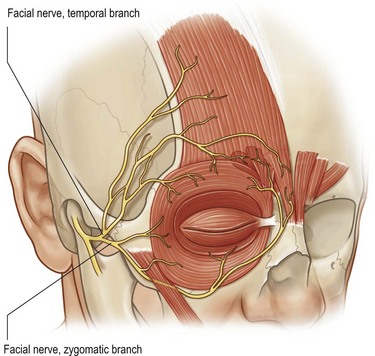
Motor nerves
The temporal branch of the facial nerve is the only motor nerve of concern in this area. Loss of this branch would result in a brow ptosis and asymmetry due to impaired frontalis action (Fig. 7.12). The anatomy of this nerve has been well described.30–33
The temporal branch enters the temporal fossa as multiple (2–4) fine branches which lie on the periosteum of the middle third of the zygomatic arch. Between 1.5 cm and 3.0 cm above the arch, these branches become more superficial, entering the superficial temporal fascia (temporoparietal fascia), traveling on to innervate the frontalis, superior orbicularis and glabellar muscles.34
1. The middle third of the palpable zygomatic arch
2. 1.5 cm lateral to the tail of the eyebrow
3. Parallel and adjacent to the inferior temporal septum
4. Immediately superior to the sentinel vein (medial zygomaticotemporal vein).
Patient presentation
Forehead aging
Historically, the visible signs of forehead aging have been described in two ways. First, and most obvious are the furrows caused by the repetitive action of underlying muscles: transverse lines are due to the eyebrow lifting action of the frontalis, while glabellar frown lines are due to the corrugator, depressor supercilii, and the procerus. The corrugator, being the most transverse of these muscles causes vertical frown lines, the depressor supercilii, being oblique, causes oblique folds which cut across the orbital rim, and the vertically running procerus causes transverse lines at the radix (Figs 7.13, 7.14).
Second, it has been assumed that the forehead/eyebrow complex becomes ptotic with age, encroaching on the orbit, causing a pseudo-excess of upper eyelid skin. While consistent with the age-related ptosis of most other body parts, the facts are not so clear. Some studies actually suggest that eyebrows may rise with age, at least in the medial and central portions (Figs 7.15, 7.16).35–37
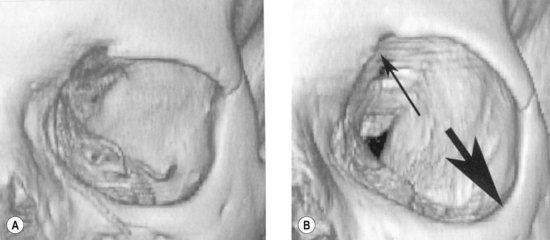
A final factor is the shape of the orbital aperture which appears to enlarge with age, the superomedial brow rising, and the inferolateral orbital rim dropping and receeding.38,39 This could contribute to a rising medial brow, because of soft tissue attachment and the soft tissue support provided by the trunk of the supraorbital nerve (Fig. 7.17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree