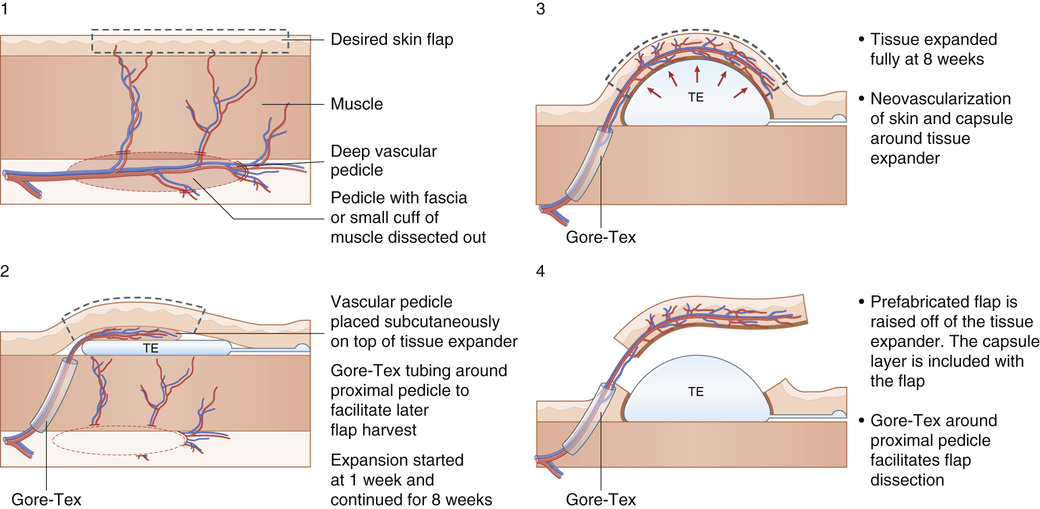
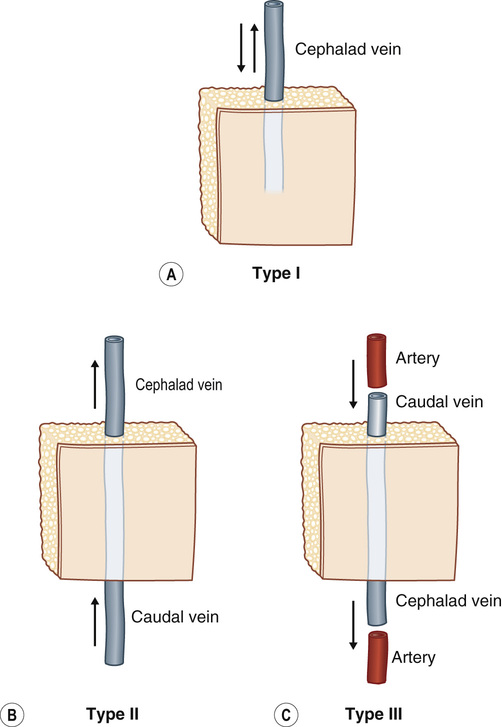
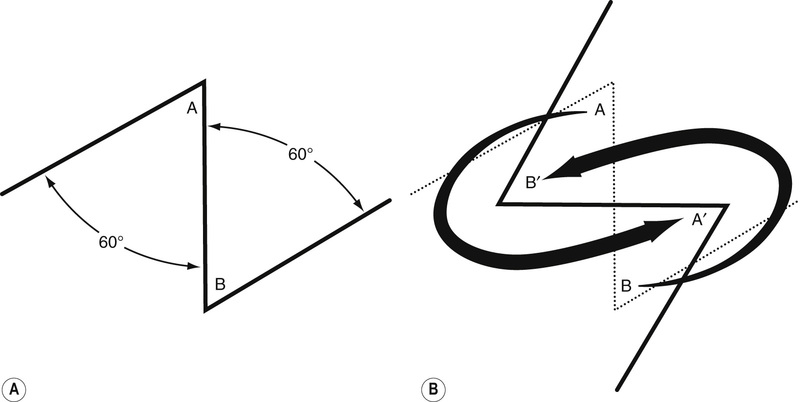
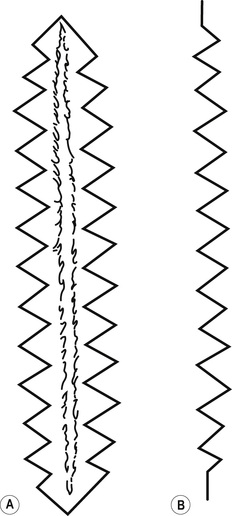
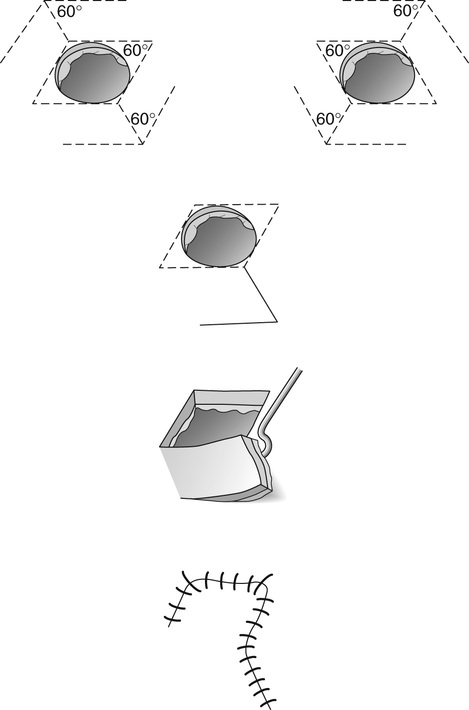
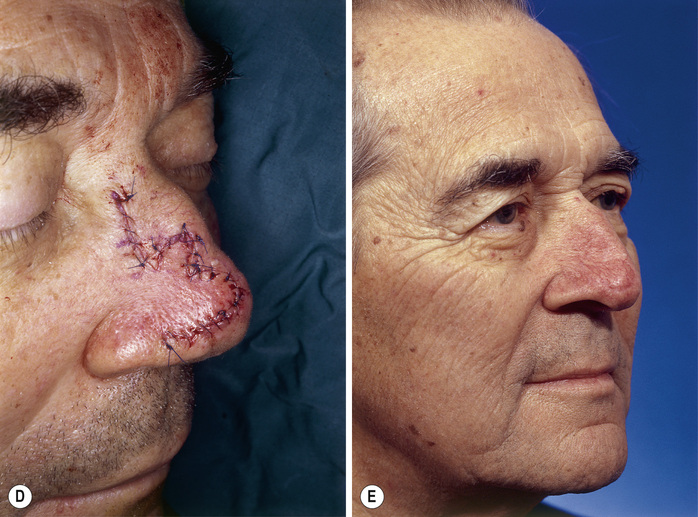
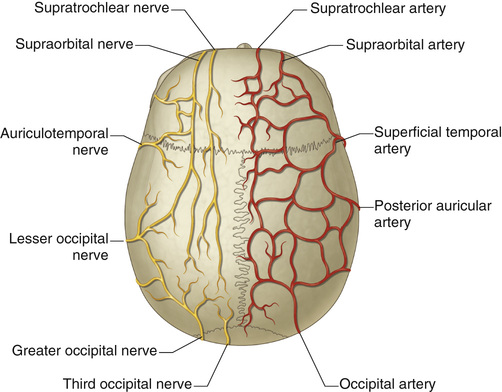
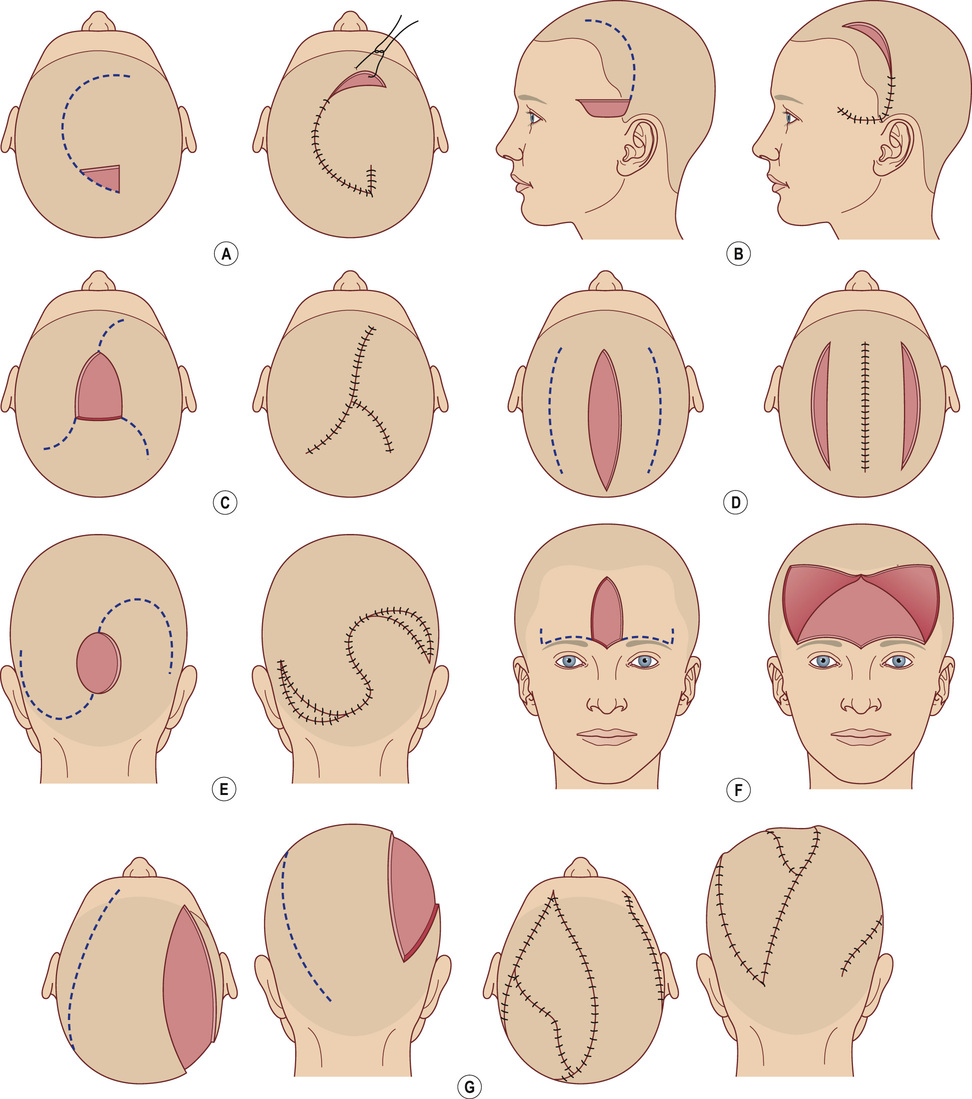
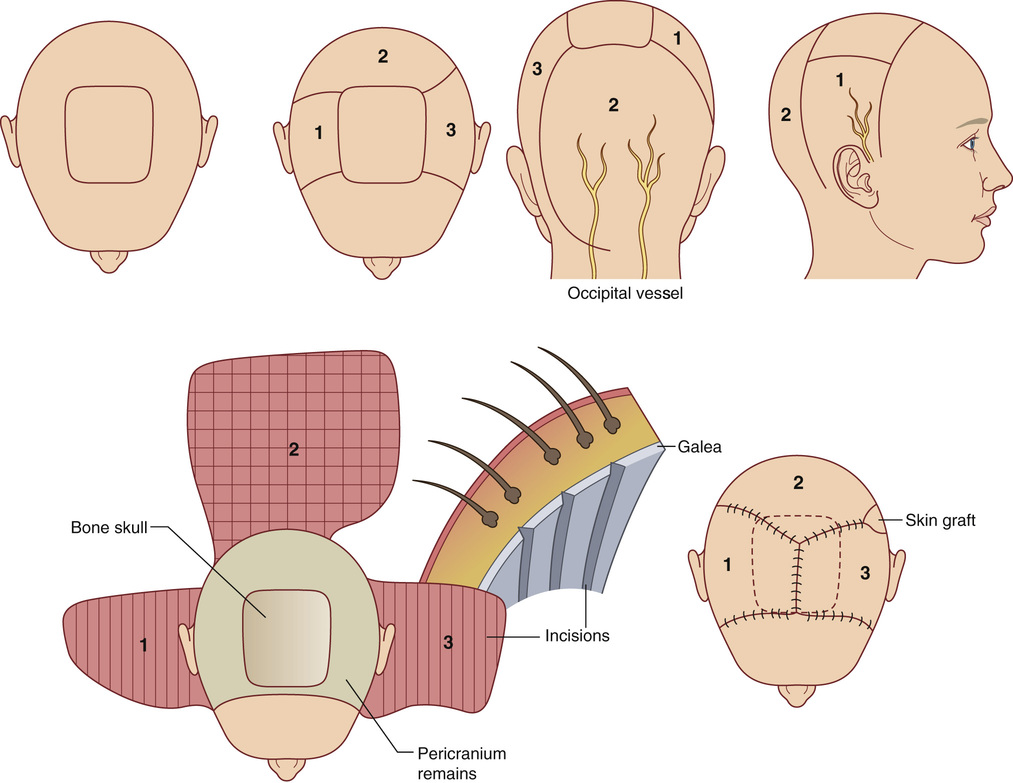
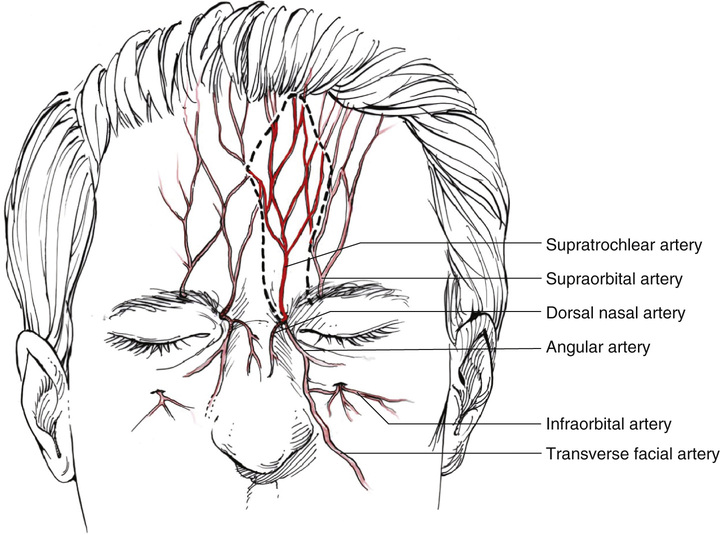
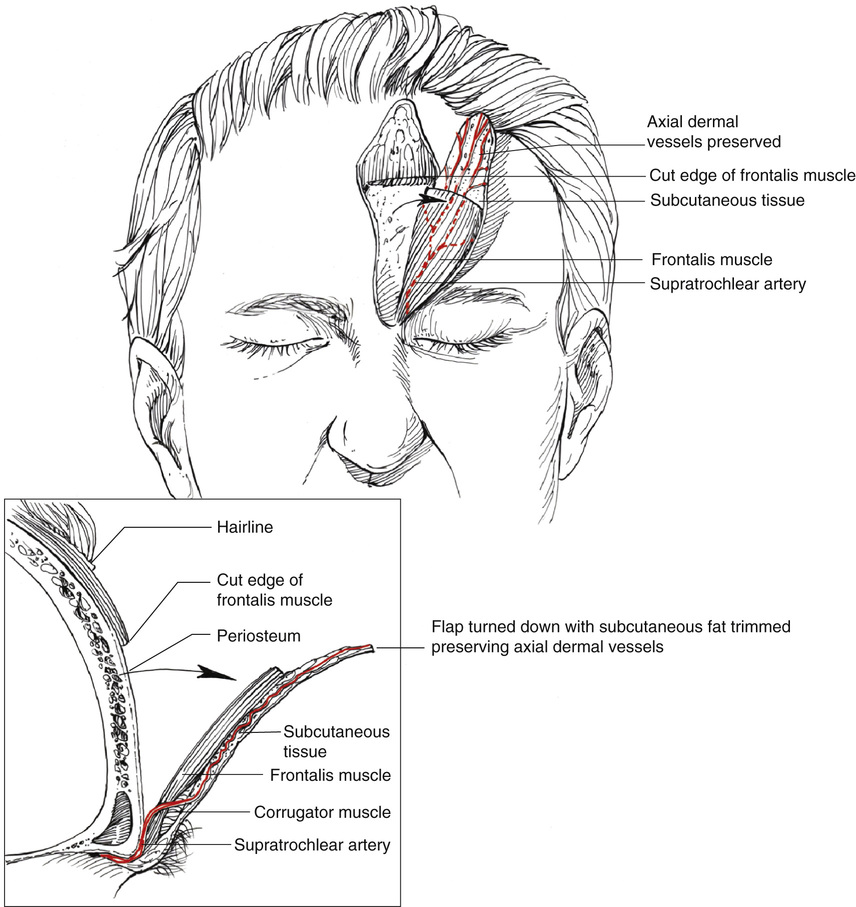
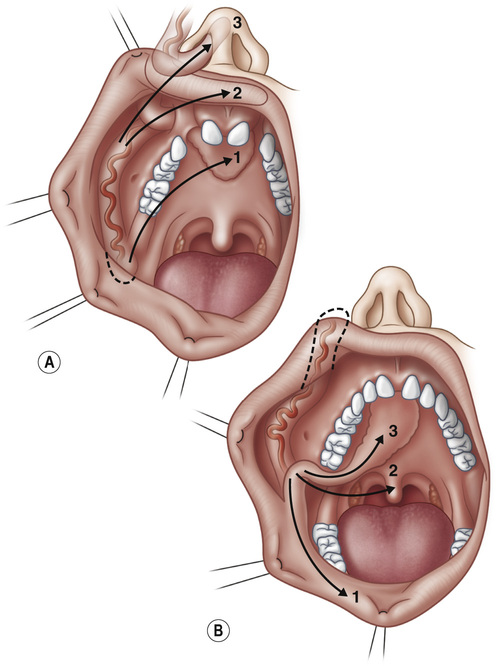
7. Prefabricated flap (see Figure 25.1): A flap that is created by introducing a vascular pedicle to a desired donor site that on its own does not possess an axial blood supply. This induces vascularization of the donor site from the pedicle before transfer. 8. Tubed flap: A flap that is rolled on itself to serve as a conduit 9. Reverse flow flap: A flap that is supplied through retrograde flow 10. Venous flap (see Figure 25.2): A flap of skin, subcutaneous, tissue, and a venous plexus, whereby the inflow and outflow of the flap is through veins. 1. Z plasty: Useful for increasing length along a central limb • Degree of angles dictates the amount gained in length ▪ 30 degree angle leads to a 25% gain ▪ 45 degree: angle leads to a 50% gain ▪ 60 degree angle leads to a 75% gain ▪ 75 degree angle leads to a 100% gain ▪ 90 degree angle leads to a 120% gain (see Figure 25.4) 2. W plasty: Useful for scars that cross the relaxed skin tension lines • Requires undermining and removal of “healthy” surrounding tissue for closure (see Figure 25.5) 3. Rhomboid flaps: A rotation flap based on a rhomboid skin design that allows closure of the donor site primarily (see Figure 25.6) 4. Bilobed flaps (see Figure 25.7): A double transposition flap that allows for movement of skin over a longer distance than possible with a single transposition flap • Useful for reconstruction of defects within the face and nose 1. Scalp flaps: Highly redundant blood supply allows for multiflap variations based off of a vascular pedicle. • Vascular supply (see Figure 25.8): Supratrochlear a. and supraorbital a. (anterior scalp); superficial temporal a. (temporal scalp); posterior auricular a. (parietal scalp); occipital a. (occipital scalp) • Primary closure often possible for defects <3 cm in diameter ▪ May require galeal scoring to enhance tissue stretch • Scalp rotation flaps (e.g., orticochea) are useful for defects with a maximum diameter of 6 cm or <50% total surface area (TSA). ▪ In some instances, the donor site from the rotation can be skin grafting as long as the pericranium is not violated during flap elevation (see Figures 25.9 and 25.10). • Vascular supply: Supratrochlear a. • Disadvantages: Requires multiple stages; if flap extends into hair-bearing region, can get persistent hair growth after transfer (see Figures 25.11 and 25.12) 3. Temporoparietal fascia (TPF) flap • Vascular supply: Superficial temporal a. • Advantages: Thin flap, pliable • Useful for coverage of tendons, exposed joints, or in areas where a thin fascial flap is desired 4. Facial artery musculomucosal (FAMM) flap • Dissection includes buccinators muscle • Can be used for oronasal defects of the palate, alveolus, and nasal septum (see Figure 25.13)
Flaps and Microsurgery
Flap Definitions
Common Local Flaps
Common Flaps of the Head and Neck
Flaps and Microsurgery
Chapter 25