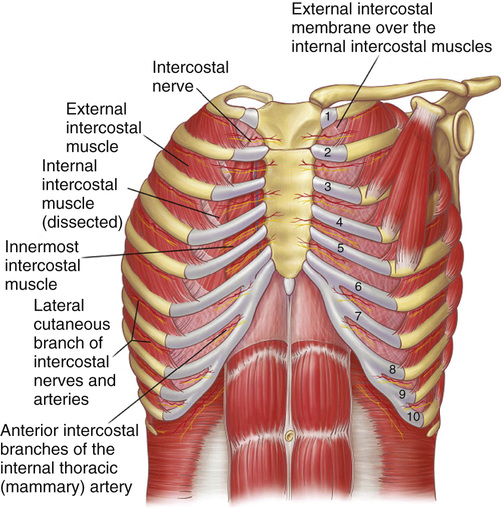
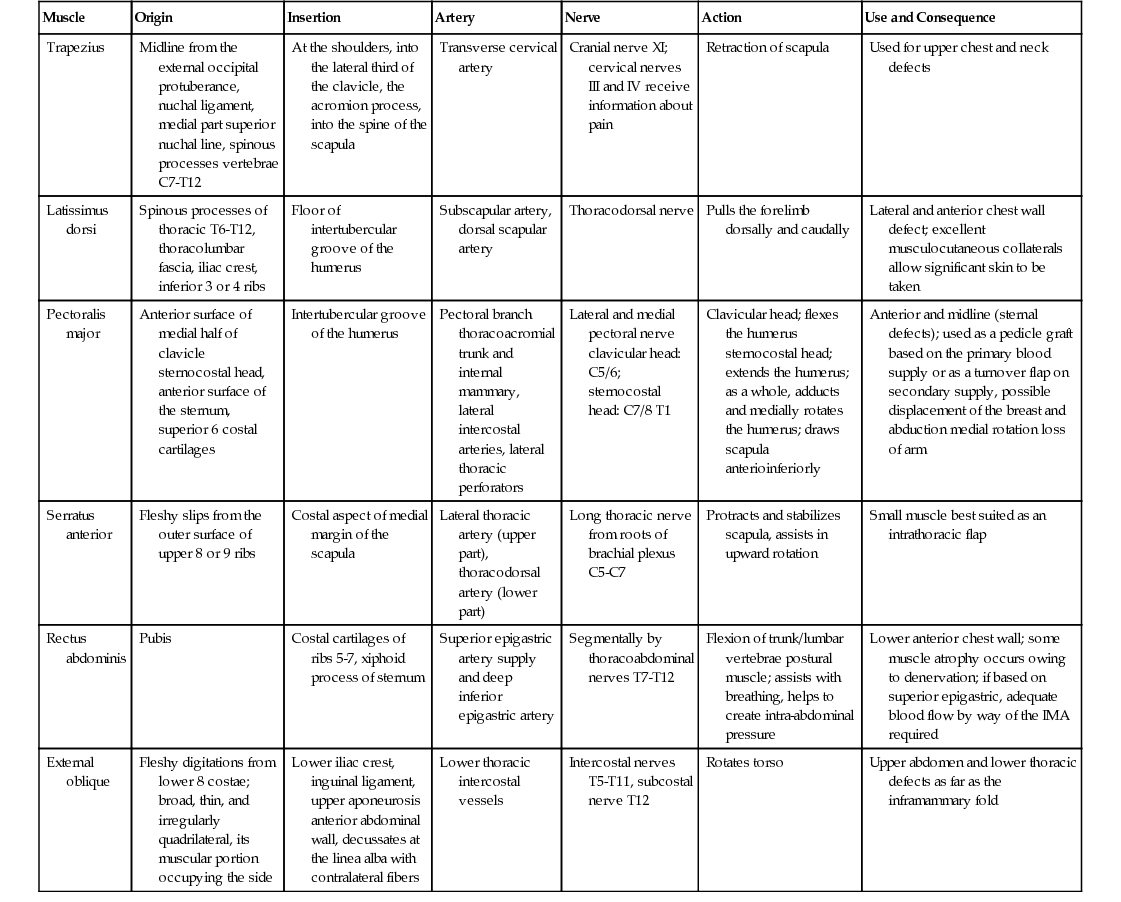
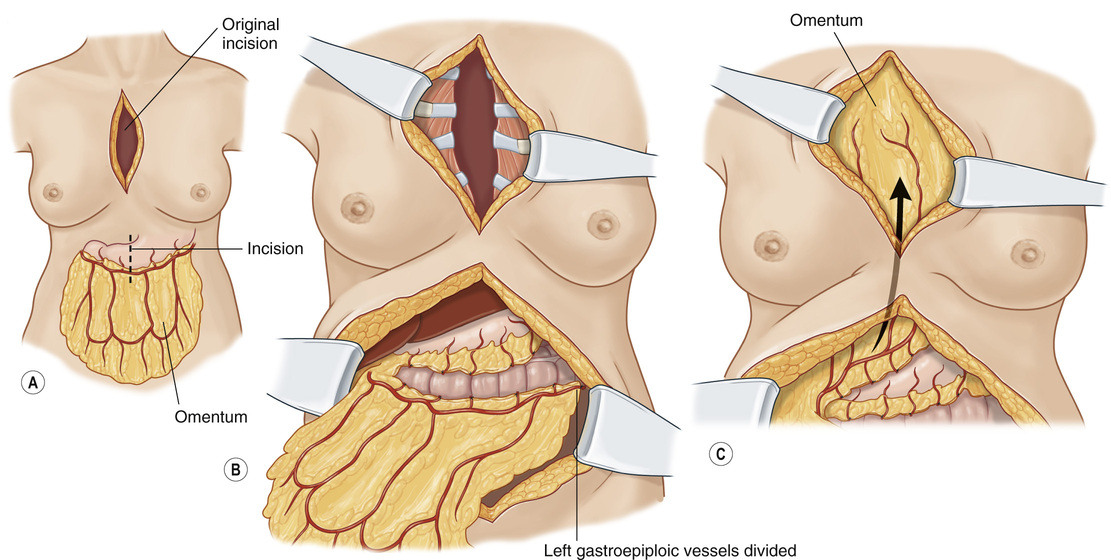
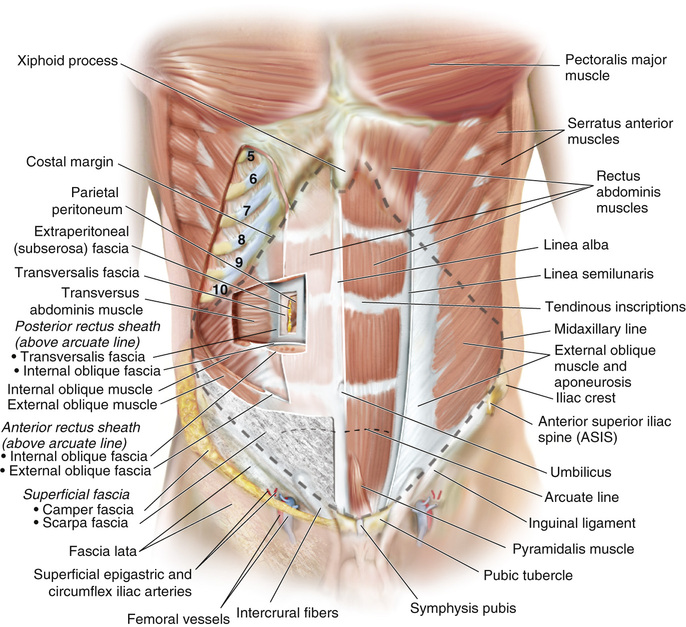
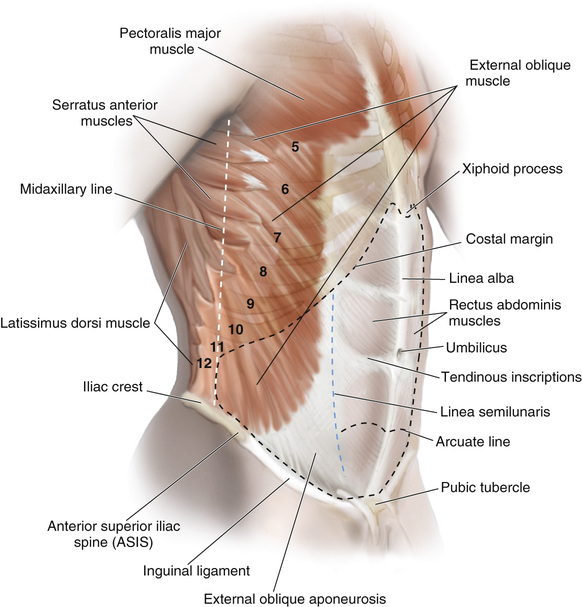
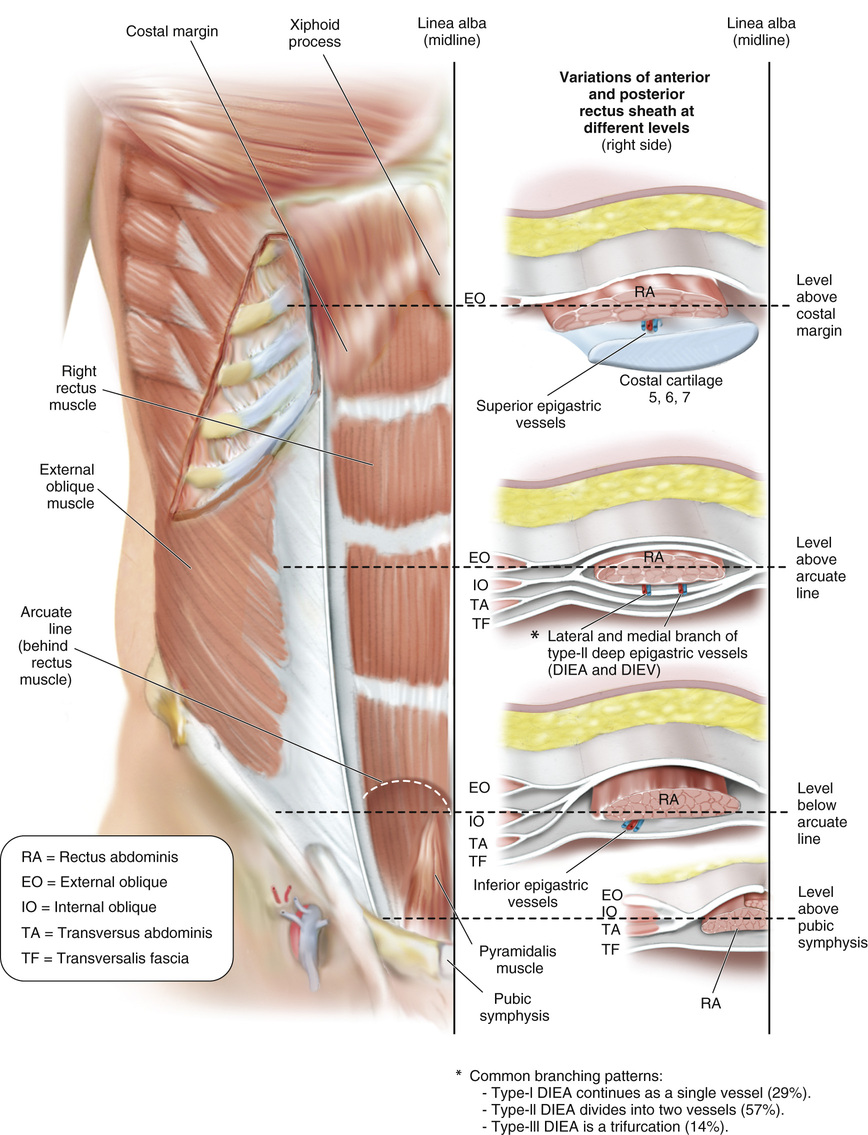
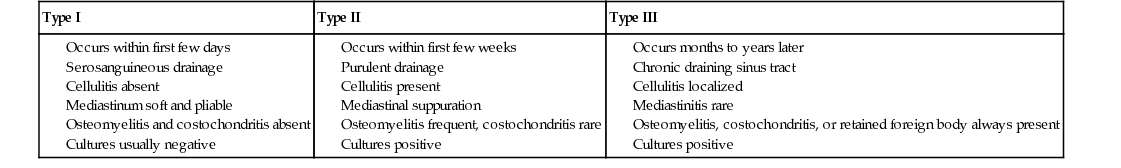
1. The chest wall is composed of a bony shell that protects critical structures (e.g., heart, lungs, liver, kidneys) with a muscular component that assists with respiration as well as stabilization and motion of the upper extremities (see Figure 11.1). 2. There are 12 paired ribs that make up the bony framework of the chest wall. 3. The sternum contains three bony parts. ● The manubrium articulates with the first ribs and clavicles. ● The body articulates with ribs 2 to 7. ● The xiphoid process is insignificant. ● Intercostal muscles (external, internal, innermost m.) run between ribs, contain neurovascular bundles, and function to increase chest wall volume during inspiration. ■ The neurovascular bundles run between the internal intercostal muscles and the innermost intercostal muscles, just inferior to each rib (see Table 11.1). 2. Chest wall defects following tumor extirpation often result in large segmental composite defects. ● In general, stabilization of the chest wall, in addition to soft-tissue coverage, is required in defects >5 cm or more than 2 to 3 contiguous ribs. ■ Larger posterior rib defects may be tolerated because of the scapula. 3. Mediastinitis following sternotomy is reported to occur in 0.25% to 5% of cases. ● Risk factors include diabetes, bilateral internal mammary artery (IMA) harvest, and obesity. 4. Pairolero and Arnold classified sternal wound infections into three types (see Table 11.2). Table 11.2 Classification of Infected Sternotomy Wounds Osteomyelitis and costochondritis absent Osteomyelitis frequent, costochondritis rare Osteomyelitis, costochondritis, or retained foreign body always present 5. Reconstruction of sternal wounds largely depends on the type of infection, degree of purulence, and presence of bone and/or cartilage infection or necrosis. 6. Common flaps for reconstruction of sternal wounds include ■ Vascular supply: Thoracoacromial artery (major), IMA perforators (minor, segmental) ■ Limited coverage of inferior sternal wounds ■ Muscle can be disinserted to allow for additional reach. ■ Vascular supply: Superior and inferior epigastric a. ■ Useful for coverage of inferior sternal wounds ■ Vascular supply: Thoracodorsal a. (major), lumbar perforators (minor, segmental) ■ Useful for lateral chest wall defects ● Omentum ■ Vascular supply: Gastroepiploic artery (major), short gastrics (minor) ■ Useful for large sternal wounds ■ Requires laparotomy and tunneling of flap through the diaphragm or extrathoracic ■ Requires skin graft (see Figure 11.2) 1. The abdominal wall is a hexagonal-shaped structure that functions to ● Protect critical intra-abdominal structures ● Stabilize the pelvis during walking, running, and jumping ● Increase intra-abdominal pressure (e.g., to assist with expiration and defecation) 3. Innervation: Nerves travel with the intercostal and lumbar arteries in the plane between the internal oblique (IO) and transversalis muscles. ● Sensory: Anterior branches of the T7 to L1 intercostal and subcostal nerves ● Motor: T7 to L2 intercostal nerves, iliohypogastric n., ilioinguinal n. ■ Origin: Pubic symphysis and pubic crest ■ Insertion: Anterior surfaces of 5th to 7th costal cartilages and xiphoid ■ Principle flexor of the abdomen, stabilizes pelvis, protects abdominal organs ■ Vascular supply: Segmental intercostal a., deep circumflex iliac a., iliolumbar a. ■ Insertion: Pubic crest; forms the inguinal ligament ● IO ■ Vascular supply: Intercostal a., circumflex iliac a., iliolumbar a. ■ Origin: Thoracolumbar fascia, iliac crest, inguinal ligament ■ Insertion: Inferior and posterior borders of ribs T10 to T12; pubic crest via the conjoint tendon ■ Vascular supply: Intercostal and subcostal a. ■ Origin: Iliac crest, inguinal ligament, inner surface of T6 to T12 costal cartilages ■ Insertion: Posterior rectus sheath (above arcuate line); pubic crest via the conjoint tendon 5. The rectus sheath is located in the midline of the abdominal wall and is formed via the aponeuroses of the abdominal musculature. The components of the anterior and posterior rectus sheath change according to position with respect to the arcuate line (located midway between the umbilicus and pubic symphysis). 6. The linea semilunaris or semilunar line marks the junction between the medial border of the external oblique muscle and lateral border of the rectus muscle where the anterior rectus fascia merges with the external oblique aponeurosis (see Figures 11.3–11.5).
Trunk Reconstruction and Pressure Sores
General Chest Wall Anatomy
Chest Wall Reconstruction
Type I
Type II
Type III
Abdominal Wall Anatomy
Trunk Reconstruction and Pressure Sores
Chapter 11