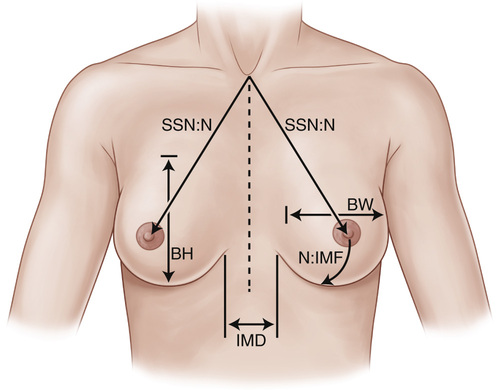
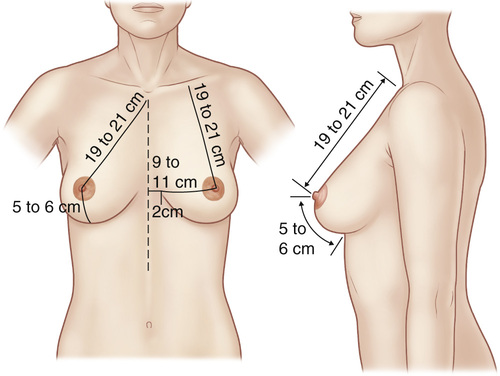
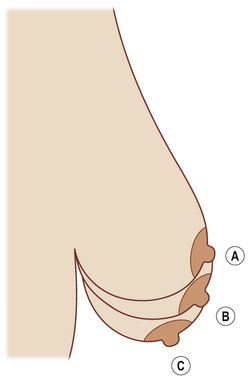
2. Indications 3. Contraindications: Similar for all esthetic surgery • Patient is being pushed into surgery by others or desires to please others. • Patient seeking esthetic breast surgery because of marital problems or familial disapproval • Patient who has been “doctor shopping” or has had multiple prior surgeries but is still dissatisfied 1. Macromastia signs and symptoms 2. Preoperative considerations • Postoperative nipple-areolar complex (NAC) perfusion and sensation ▪ Rates of breast-feeding in women after breast reduction surgery are similar to those of child-bearing women who have not had breast reduction surgery. ▪ Most important determinant of ability to breast-feed after breast reduction surgery is pedicle thickness ○ Pedicle type and reduction volume has no effect. ○ Impossible with free nipple grafting. • Breast measurements (see Figures 10.1 and 10.2) ▪ Sternal notch-to-nipple distance ▪ Many advocate for preoperative mammography before surgery with any breast masses, breast complaints, or at-risk women (>35-40 years old [yo]) whose mammogram is over 1 year old. ○ Risk of occult breast cancer occurrence in reduction specimen is extremely rare (reportedly 0.2%). ○ When found, cancer is often early stage or in situ carcinoma. 3. Techniques ▪ Can be used alone in select patients ▪ Contraindicated in patients with breast ptosis or who will likely require skin reduction ○ Rapid recovery and return to work ○ Minimal risk to nipple sensation/perfusion ○ Minimal risk to postoperative lactation ○ Unable to pathologically examine lipoaspirate ○ High risk of inadequate reduction ○ Skin contraction unpredictable, leading to excess skin ○ Unable to correct breast ptosis • Traditional reduction mammaplasty ▪ Combines a skin excision pattern with a pedicle to maintain nipple perfusion ○ Skin patterns include Wise pattern, keyhole, vertical, and no-vertical-scar techniques ○ Pedicle options include superior, medial, superomedial, inferior, lateral, and central pedicle ◆ The inferior pedicle can achieve significant volume reduction and reduce the vertical dimension of the breast. ➔ Can be used for all reductions, including moderate to severe reductions (>800 g) 4. Complications: Risk factors include obesity, reduction volume >1000 g, and smoking. • Scarring ▪ Long-term complication most associated with patient dissatisfaction ▪ Greatest risk factor for hematoma is hypotensive anesthesia ▪ Drains have not reduced the incidence of hematoma. ▪ Characteristic finding: Development of delayed, firm, and nontender masses • Skin loss and wound development (especially at the inferior T junction in Wise pattern reductions) ▪ Most common complication in obese patients with large reduction volume ▪ Risk factors: Smoking, elevated body mass index (BMI), and long pedicle ▪ Etiology ○ Intrinsic physiologic risk (obesity, smoking) ○ Excessive nipple-to-IMF distance/pedicle length and excessive sternal notch-to-nipple distance ○ Excessive tension on the closure ○ If immediately after reduction, pedicle exploration with release of tension ○ If pedicle release does not result in improvement, convert to free nipple graft ◆ Be sure to graft to well-vascularized tissue and not the compromised skin flap or pedicle. 2. Breast ptosis: Relationship of the NAC to the IMF and lower contour of the breast (see Figures 10.3 and 10.4) ▪ Grade I: NAC within 1 cm of the IMF and above the lower contour of the breast ▪ Grade II: NAC is 1-3 cm below the IMF but above the lower contour of the breast ▪ Grade III: NAC >3 cm below the IMF and at the lower contour of the breast ▪ Grade IV (pseudoptosis): NAC at the level of the IMF, but the majority of the breast volume has descended below the IMF ○ Increased nipple-to-IMF distance in setting of stable sternal notch-to-nipple distance
Noncancer Breast Surgery
General Information
Reduction Mammaplasty
Mastopexy
Noncancer Breast Surgery
Chapter 10