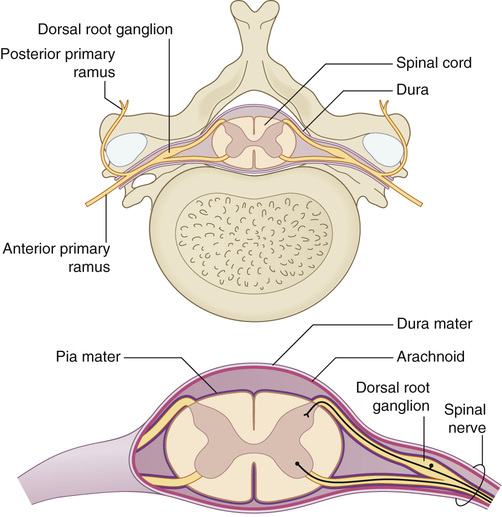
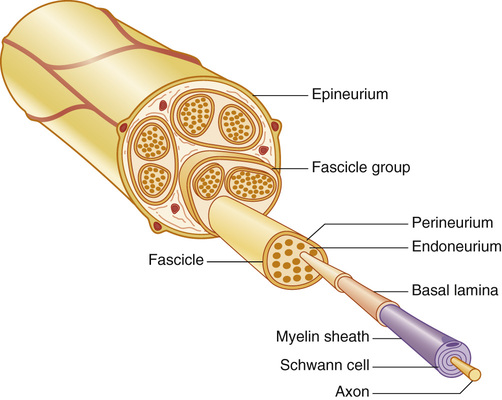
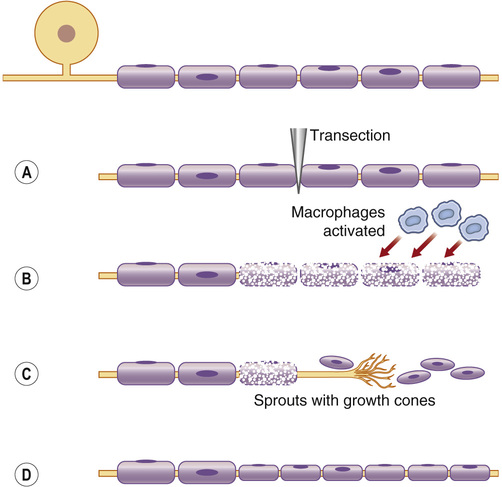
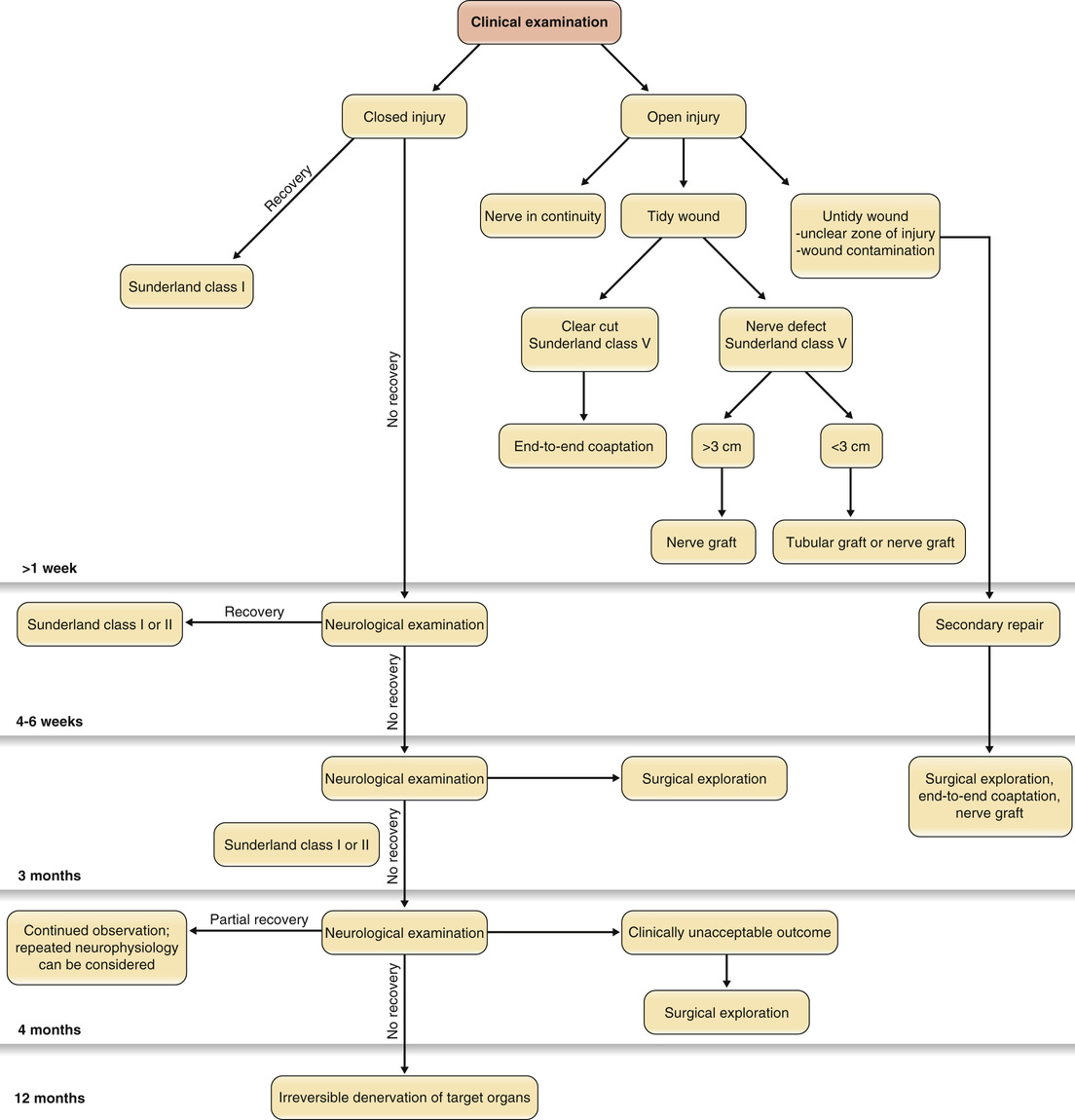
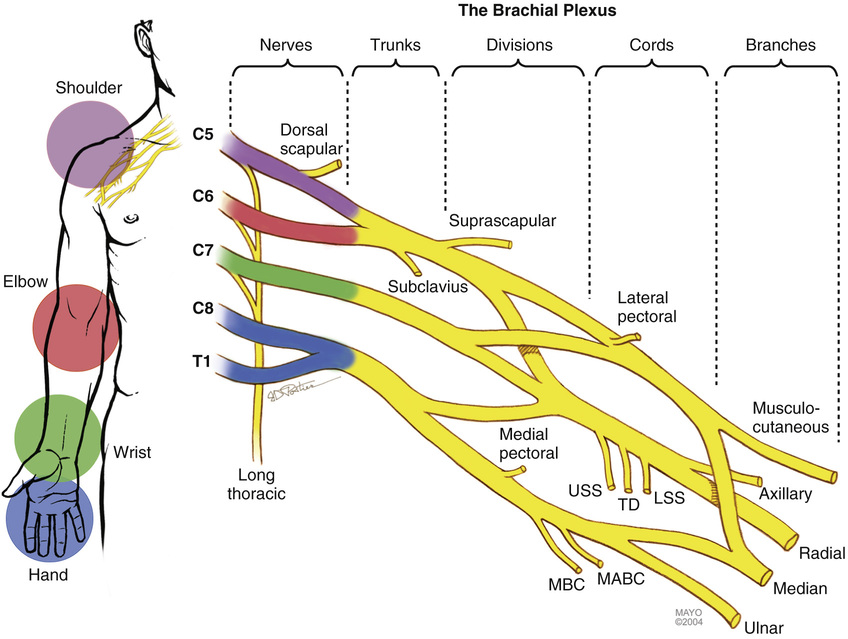
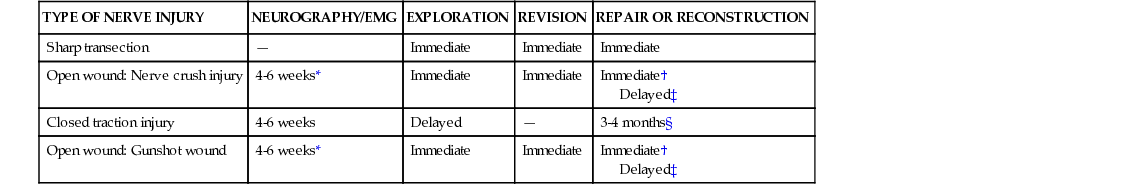
2. The anterior (ventral) and posterior (dorsal) nerve roots arise from rootlets on the spinal cord and merge into the spinal nerves (see Figure 12.1). 6. Bundled axon nerve fibers are surrounded by endoneurium and grouped with other neurons by a collagen layer called perineurium. This group of neurons is termed a fascicle. • Within a peripheral nerve, the fasicles are also imbedded in loose connective tissue composed of collagen and fibroblasts (the epineurium; see Figure 12.2). 7. The vascular supply of the nerve consists of segmental blood vessels that branch into several vascular plexuses along the epineurium and within the perineurium and endoneurium. • This redundancy allows nerve mobilization over extended lengths without disruption of blood supply. 1. Myelinated nerve fibers have high conduction velocity because the action potentials jump from node of Ranvier to node of Ranvier. 2. After nerve injury, the axons and myelin sheath in the distal segment degenerate (“Wallerian degeneration”), whereas the Schwann cells coordinate nerve repair and regeneration by up-regulating the production of neurotrophic factors and their receptors (see Figure 12.3). • Wallerian degeneration takes time after injury. • Motor and sensory function should be fully assessed. • Electromyography (EMG) assesses the motor component of a nerve only. • Nerve conduction studies (NCSs) assess sensory (sensory nerve action potentials [SNAPs]) and motor (compound motor action potentials [CMAPs]) components. ▪ Preganglionic injuries are associated with loss of sensation but show intact SNAPs and absent CMAPs. 1. Closed nerve injuries should be treated conservatively with observation for signs of recovery. • Consideration for electrophysiologic testing should be deferred until at least 4-6 weeks after injury, and many can wait until 3 months. ▪ If at 3 months there is no sign of recovery, nerve exploration is warranted. 2. Open nerve injuries should be explored immediately. • If the nerve is found to be in continuity, treat as above as if it were a closed injury. 3. Nerve repair can occur either immediately or after delay. ▪ Method of choice, especially if performed within 48 to 72 hours ▪ Technically easier than delayed repair ○ Less retraction of nerve ends ▪ Typically requires a nerve graft ▪ Impaired functional outcomes (see Table 12.1) Table 12.1 Differing Treatments for Different Types of Nerve Injury 4. Primary repair must occur without tension; otherwise, consider a nerve graft. • For nerve gaps <3 cm, nerve conduits (e.g., synthetic, vein) can be used. • For nerve gaps >3 cm, nerve grafts are recommended. ▪ Common donor grafts: Sural n., posterior interosseous n., lateral antebrachial cutaneous n. 5. Nonviable tissue must be resected until healthy fasicles are identified. 7. Nerve ends are commonly coapted with interrupted 9-0 or 10-0 nylon sutures. • Repair can occur at the epineurial or fasicular level. • Grouped fasicular repair is preferred for injuries to the ulnar n. at the wrist. 9. Nerve transfer is a newer technique that has primarily been used with proximal or brachial plexus injuries to provide a source of regenerating axons in close proximity to the end target and preserve motor end plates. • Nerve transfers are associated with minimal to no downgrade in donor function and provide better outcomes (see Box 12.1 and Figure 12.4). 1. Formed from the anterior primary rami of spinal nerves C5 to T1 4. The mixed spinal nerves travel between the anterior scalene m. and the middle scalene m. to form three trunks. 5. Beneath the clavicle, each trunk divides into anterior and posterior divisions. 6. Distal to the clavicle, the nerves exchange fibers to form cords. ▪ Formed from the anterior divisions of the upper and middle trunks ▪ Passes anterior to the subclavian artery ▪ Gives rise to the lateral cord contribution to the median n. and the musculocutaneous n. ▪ Formed from the anterior division of the lower trunk ▪ Passes anterior to the subclavian artery ▪ Gives rise to the medial cord contribution to the median n. and the ulnar n. ▪ Formed from the posterior divisions of all trunks ▪ Passes posterior to the subclavian artery ▪ Forms the axillary nerve and the radial nerve (see Figures 12.5 and 12.6)
Peripheral Nerve Injuries, Brachial Plexus, and Compression Neuropathies
General Nerve Anatomy
Nerve Physiology
Diagnosis of Nerve Injury
General Nerve Repair Principles
TYPE OF NERVE INJURY
NEUROGRAPHY/EMG
EXPLORATION
REVISION
REPAIR OR RECONSTRUCTION
Sharp transection
—
Immediate
Immediate
Immediate
Open wound: Nerve crush injury
4-6 weeks*
Immediate
Immediate
Immediate†
Delayed‡
Closed traction injury
4-6 weeks
Delayed
—
3-4 months§
Open wound: Gunshot wound
4-6 weeks*
Immediate
Immediate
Immediate†
Delayed‡
Brachial Plexus
Peripheral Nerve Injuries, Brachial Plexus, and Compression Neuropathies
Chapter 12