1. Keratocanthoma (see Figure 23.1)
• Benign tumor that behaves like a squamous cell carcinoma (SCC) and is difficult to differentiate histologically
• Characterized by rapid growth with a central crater/keratin plug
• Can spontaneously regress
• Treatment recommendation: Excision
2. Actinic keratosis (AK; also known as solar keratosis, senile keratosis; see Figure 23.2)
• Extremely common skin lesions reportedly affecting up to 12% of the population
• Benign, premalignant lesion that can progress to SCC
▪ Estimated rate of conversion to SCC is 13% to 20% over 10 years for lesions that are untreated.
• More than 80% occur on sun-exposed/sun-damaged areas such as the head, neck, and upper extremities (e.g., dorsal hand/forearm).
• Risk factors: Chronic sun exposure, increasing age, male gender, fair skin
• Characterized by a rough, erythematous papule with a white to yellowish scale or plaque
• Treatment: Cryosurgery, photodynamic therapy, medical treatment (e.g., topical or intralesional 5-fluorouracil [5FU], topical imiquimod)



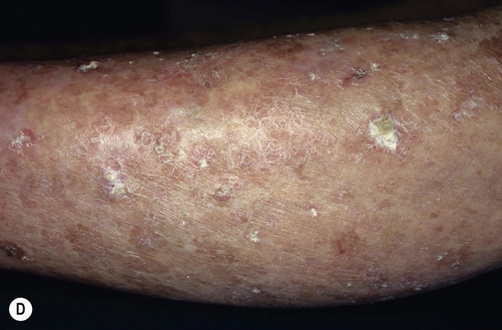
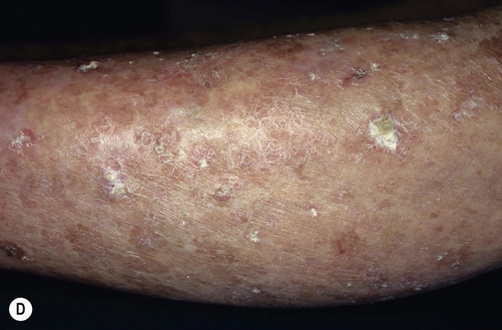
Figure 23.2 Actinic keratoses (AKs). A, Multiple AKs on the face of an elderly woman with fair complexion, blue eyes, and moderate-to-severe photodamage; the AKs vary in size from a few millimeters to >1 cm. On the left forehead, the red nodule with slight scale-crust represents a well-differentiated SCC. B, Pink-colored, atrophic AK with minimal scale on the forehead. C, Numerous hypertrophic AKs on the bald scalp with hypopigmentation at sites of previous treatment. D, Multiple large, hypertrophic AKs on the shin of an elderly woman; note the thick scale. (Reprinted from Bolognia, J.L., Jorizzo, J.L., Schaffer, J.V. [Eds.], 2012. Dermatology, 3rd ed. Elsevier, 1773–1793. B, Courtesy Iris Zalaudek, M.D.; D, Courtesy Jean L. Bolognia, M.D.) 3. Seborrheic keratosis (SK; also known as a senile wart) (see Figure 23.3)
• Benign skin growth originating from the basal and squamous cells of the epidermis
• Characterized by well-circumscribed, waxy lesions that are occasionally pigmented and have a “stuck-on” appearance
• Must be differentiated from AK, basal cell carcinoma (BCC), and melanoma
• Sudden appearance of multiple SKs can be a marker of internal malignancy.
• Treatment: Laser therapy, cryotherapy, electrosurgery, and excision
4. Nevus sebaceous (“nevus sebaceous of Jadassohn”) (see Figure 23.4)
• A benign hamartoma confined to the head and neck regions
• Can have malignant degeneration into BCC
• Characterized by a waxy, smooth or papillated, hairless, salmon-colored patch or thickening on the scalp that typically presents at birth
• Treatment: Excision
5. Juvenile melanoma (“Spitz nevus”; see Figure 23.5)
• Benign pigmented skin lesion typically found in children or young adults
• Difficult to distinguish from melanoma clinically and histologically
• Characterized by a red, pink, or brown papule or nodule with rapid growth
• Treatment: Complete excision with negative margins; if any concern for melanoma, obtain appropriate margins based on depth.

Figure 23.5 Spitz nevus. Red, dome-shaped papule on the ear of a child. (Reprinted from Bolognia, J.L., Jorizzo, J.L., Schaffer, J.V. [Eds.], 2012. Dermatology, 3rd ed. Elsevier, 1851–1883. Courtesy Ronald P. Rapini, M.D.) 6. Nevus of Ota (see Figure 23.6)
• Benign blue nevus that is present within the dermatome of the first and second branches of the trigeminal nerve
• Most commonly affects Asian females
• Bimodal distribution: Early infancy and early adolescence
• Caused by dermal proliferation of melanocytes
• Treatment: Laser (e.g., Q-switched ruby, alexandrite); dermabrasion, peels, or cryotherapy have also been used.

Figure 23.6 Nevus of Ota (oculodermal melanocytosis). Unilateral, bluish-gray discoloration of the face, which is either mottled or confluent. There is also involvement of the sclera. (Reprinted from Bolognia, J.L., Jorizzo, J.L., Schaffer, J.V. [Eds.], 2012. Dermatology, 3rd ed. Elsevier, 1851–1883.) 7. Nevus of Ito
• Often considered a subtype of nevus of Ota
• Occurs in the acromiodeltoid region.
• Treatment: Similar to nevus of Ota
8. Mongolian spot (also known as congenital dermal melanocytosis; see Figure 23.7)
• A common benign proliferative disorder that affects the majority of Native American, Asian, and Hispanic infants
• Caused by entrapment of melanocytes within the dermis during development
• Characterized by multiple bluish-gray spots or a large patch covering the lumbosacral region
• Lesions typically disappear by 10 years of age.
• Treatment: Observation because most disappear without treatment; lasers for severe cases.
9. Blue nevus
• Also caused by dermal melanocytosis
• Characterized by a well-circumscribed, firm, blue-pigmented nodule/papule
• Three subtypes: Common, cellular (can invade the subcutaneous tissue), and combined (combined with a pigmented nevus or a Spitz nevus)
• Treatment: Biopsy for suspicious lesions; simple excision (see Figure 23.8)

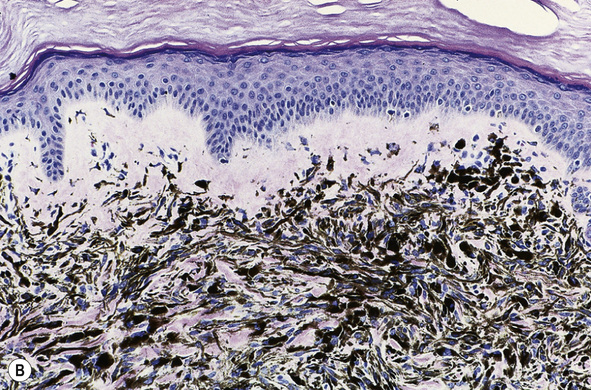
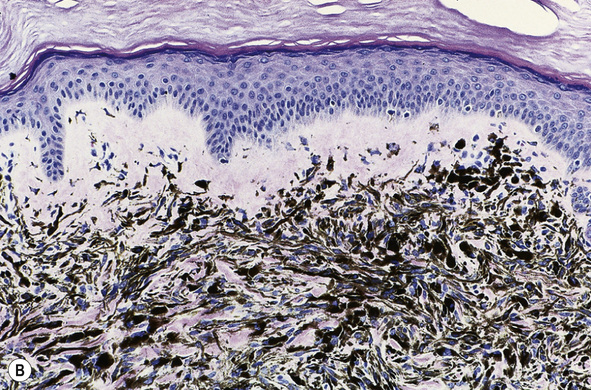
Figure 23.8 Common blue nevus. A, A well-circumscribed, blue, dome-shaped papule. B, Histologically, heavily pigmented, spindle-shaped melanocytes as well as melanophages are within the dermis; the melanocytes are denser than in dermal melanocytosis or nevus of Ota. (Reprinted from Bolognia, J.L., Jorizzo, J.L., Schaffer, J.V. [Eds.], 2012. Dermatology, 3rd ed. Elsevier, 1851–1883.)
Only gold members can continue reading.
Log In or
Register to continue
Related

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree