Introduction
The hand is in harm’s way. It is at the frontier of all work and contact with the environment. The fingertips, as a collective functional unit, bear the statistical brunt of such injuries. Hand injuries constitute the single most frequent surgical presentation in an average Emergency Department.
The hand is unique in its dual role as a considerable gatherer of information about the environment and also as an executor. Unlike the other major sensory organ, the eye, the hand is also able to act on the information gathered, constantly modifying action by feedback of sensation and proprioception. The gathering of information about the environment is especially developed in pulp and palmar digital skin, which is not to be regarded merely as skin covering, but as a specialized organ in its own right. The dense population of sensory end organs is housed in skin with specialized, mechanical properties. The skin is robust and yet deformable – the nail complex and the skeleton provide a fixed stop, against which the pulp and palmar skin complex are deformed – without such a rigid stop, one would obtain less meaningful information about the contour and texture of a held object or touched surface.
The esthetic importance of the hand is not to be underestimated and is an important consideration in all reconstruction. Irrespective of custom and attire, in virtually all societies, the hand is always on display (the hand is exposed even in societies where the face is concealed). The back of the hand, in particular, is a significant esthetic unit. In this regard, function and appearance are closely interlinked. The hand which behaves fluently and efficiently attracts little attention, even if it carries significant scar, or is missing anatomical parts. Smooth, healthy-looking skin cover, as well as fluid, natural behavior, form important aspects of social acceptability. Hand gestures reinforce facial expression and in some spheres, hand movement and posture constitute a very specific vocabulary, interpretable by those who converse in that language. Aside from the obvious example of signing for the deaf, the orchestra conductor’s hand gestures speak a clear language to musicians and culture-specific hand gestures convey meaning over distance beyond that possible through sound. Convention and social context convey specific messages with hand gestures – the extended index finger held vertically over the lips is universally interpreted as a request for quiet, for silence. It is also relevant that the hand is the most frequent acceptable point of contact; in most societies, the handshake is considered a permissible intrusion into personal space, and a permitted form of contact, irrespective of the difference in social standing of those shaking hands.
The hand is an integral part of one’s identity for any individual but specific professions imbue the hand with an additional importance. The musician, for instance, has a special relationship with the hand since this forms an integral part of his/her identity and “voice.” The same can be said of the craftsman or in sports that use the hand. Although these aspects form an important element of management, one must not overrate the contribution of profession to the decision-making process. While some methods of reconstruction may entail an unacceptable period off work for, say, the manual worker, whose main concern may be for strength and durability, all will require a large measure of pain-free, sensate dexterity. Irrespective of work or leisure pursuits, all will still need to perform delicate, precise tasks, such as writing and doing up fastenings and buttons, touching spouse and offspring. Most will be disturbed by an unattractive extremity on display.
Since the hand is the part most frequently involved in work-related injuries, the issue of personal injury claims and the cloud of possible compensation frequently hangs over the outcome of repair and reconstruction.
The growing hand presents special challenges on a number of fronts. Any repair must take into account the facilitation of growth of soft tissues and skeletal elements. Scarring and contracture, a perennial problem in the hand, assume an added importance. To these factors must be added the factor of parental anxiety and elements of guilt and regret centered on the occurrence of the injury in the first place. In general, the management of the child’s hand involves the management of the family.
These various factors should all figure in the assessment of injury, the “feel” of patient compliance and cooperation, the choice and planning of repair and reconstruction, and the required aftercare. All too often these injuries are downgraded in the queue of surgical priorities – many still consider that “all soft tissue injuries of the pulp heal” without regard to the quality of function of such healing. Injuries that can lead directly to significant loss of function, persistent pain, and compromised appearance are still, regrettably, considered trivial and meriting little surgical input. They are often misguidedly delegated to inexperienced members of the surgical team with little appreciation of their complexity and functional significance.
Assessment
The challenge of reconstruction in the hand lies in the assessment and decision-making, not in the technique, however immaculately executed is the latter. In assessing any injury (and the patient) one brings to bear experience and a big repertoire so that, as far as possible, questions are answered before the start of surgery. This is not to say that plans may not change when the examination reveals more detail, but it is the planning and selection of technique that is the focus and the essential to a good outcome.
In the field of reconstruction, there are no recipes, only principles. In the management of reconstruction challenges of the digits, one vital principle is the appreciation that not all areas of the hand are of equal functional value.
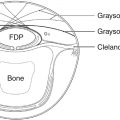
Observation of the hand in action soon reveals that all digits have leading and trailing aspects. While one would not suggest that any part of the hand is of lesser importance, in reconstructive terms these could also be considered “high premium” and “low premium” territories ( Fig. 46.1 ).
The leading edge is the more commonly used in contact with a held object or contact with a surface. The trailing edge is less often in contact, and tends to have less developed discriminatory abilities or needs. This principle is most true of the thumb: the ulnar pulp “leads” and is involved in virtually all dexterous activity and certainly all precision actions, since it is this area which faces the long digits most effectively. By contrast, the radial pulp “trails” during most tasks coming into play with relatively unspecialized tasks such as tapping on a horizontal surface or keyboard. The principle is least true of the index, both of whose aspects are frequently involved in common activity.
Once this principle is accepted, one can start to assess the functional significance of a specific defect and the availability of suitable methods of reconstruction:
- 1.
High premium areas require the best possible reconstruction, preferably sensate, glabrous pulp skin taken if possible from the same digit.
- 2.
Injury to a low premium area may be reconstructed acceptably and reliably with relatively nonspecialized cover, such as a skin graft or an insensate skin flap.
- 3.
Low premium areas can be considered for transfer to high premium areas, preferably on the same digit, as for instance the reconstruction of ulnar pulp in the thumb using radial pulp ( Fig. 46.2 ).

Fig. 46.2
Pulp exchange flap. (A) The defect involves the entire leading (ulnar)surface of the thumb pulp. (B) The trailing (radial) aspect of pulp is intact and an island flap is deigned on this pulp. (C) The flap is entirely islanded, leaving ample fat around the nerve and artery. (D) The island is transposed to reconstruct the ulnar pulp. (E) The secondary defect is resurfaced with a skin graft, in this case a full-thickness graft taken from the amputated part, which was de-fatted. (F,G) Final result at 3 months.
These observations are proposed as factors to be taken into account, and are certainly not absolute. They are amongst many that should be considered, including the requirements of the patient overall, likelihood of compliance, as well as special requirements for a particular patient, such as the playing of musical instruments or professional sport.
In few other areas of reconstruction is collaboration with the patient as essential. This element needs careful assessment if one is to obtain a good outcome – in this situation a good outcome is the maximum restoration of function (and hence appearance) and an acceptance by the patient of any limitations consequent on the injury.
Detailed informed consent also needs to take into account the time and effort investment required of the patient, particularly in the more complex reconstructions. The extension of the site of injury and/or the involvement of distant donor sites are all factors to be included in the detail of the process of informed consent.
Finally, in the process of assessment, the surgeon must also have a realistic and honest assessment of his/her capabilities. Many methods of reconstruction are attractive to the surgeon since they fulfill a natural mechanical neatness and challenge of construct. The seduction of such methods must be resisted in the absence of expertise or adequate guidance (and, preferably, also assistance) by those more experienced.
It cannot be overemphasized that the method selected must suit the defect and the level of expertise of the surgeon. In this regard one must mention that it may be entirely appropriate to select a temporary method known to be insufficient for long-term wear and restoration of function (such as a dressing or a split-skin graft on pulp), leaving all options open for reconstruction with the availability of appropriate expertise. If this approach is selected, it is wise to present this to the patient as a two-stage procedure so that he/she is prepared for the second surgery and it does not come as a “salvage,” or adjustment, of the first.
Healing by Secondary Intention
Both pulp and palmar skin have remarkable powers of regeneration, as evidenced by the reliable healing of the open palm technique advocated by McCash.
Large defects of pulp will heal reliably provided a number of important criteria are observed:
- 1.
The defect must be suited to this method. No vital structure, such as tendon, bone, or joint, must be exposed. Severely contaminated or crush defects must be thoroughly debrided of all contamination or necrosis.
- 2.
The hand must be elevated.
- 3.
The patient must understand that the method requires careful adherence to instruction and compliance with treatment. (Many patients will only remember that “It needs no surgery” and this is rapidly translated into “It needs no care”).
- 4.
Nonadherent dressings require regular change, preferably on alternate days. Exception is made for children, where it is routine to leave a dressing undisturbed for a week, after which the wound can be left exposed, in order to avoid the trauma of painful dressings.
The dressing in direct contact with the wound is a matter of personal preference. Tulle gras (paraffin impregnated gauze) is traditional. It is cheap and easily available or can be improvised, but dries rapidly and tends to adhere more than one might expect. Many, superior, alternatives are available, such as thin, perforated silicone sheeting (e.g., Mepitel, Mölnlycke Healthcare, Gothenburg, Sweden), which is resistant to all adherence. Chitin (Beschitin, Unitika, Osaka, Japan), and other natural substances, have their advocates. The important aspects are: nonadherence, a barrier to contamination, and assiduous care and compliance.
Surgical Options for Cover
Amputation
In cases where a significant part of the digit is crushed with accompanying disruption of the nail complex and/or the distal interphalangeal joint, amputation with closure of locally available skin may be the indicated option. In this situation, it may be appropriate to elect to ablate any nail elements which, regenerating, will be unsupported, nonadherent, unattractive or likely to lead to functional problems such as snagging on clothing.
Much morbidity results from amputation performed without proper regard to indications and points of technique. There is a natural tendency to preserve length at all costs. The aim should be to achieve a nontender digit covered by good-quality skin, irrespective of length. It is better to elect for a slightly shorter length, with good quality, mobile skin cover, than to preserve length at all costs but with a tight and painful digit end. A digit with tense, painful, skin cover may well be excluded from function, resulting in an effective loss of all useful length. This is particularly true of the index, which is readily substituted by the middle finger and regularly requires subsequent revision. It is a wise surgeon who seeks to prevent the cycle of pain, tenderness, and exclusion.
There are three generally indicative levels of amputation of the fingertip ( Fig. 46.3 ):
Level 1: involves loss of skin and only a minimal loss of nail and distal phalanx. In this case all of the tip vital structures are preserved and skin cover is indicated.
Level 2: involves loss of skin and most of the distal phalanx/nail complex. In this case the nail should be ablated and the next proximal structures to preserve are the tendon insertions. Just enough bone should be left, to preserve these insertions which will preserve power and elements of proprioception.
Level 3: has lost all nail elements and the tendon insertions. The condyles of the middle phalanx can be removed to prevent an unattractive, spatulate stump shape. The phalanx is shortened to a level where tension-free, good skin cover can be achieved. One should not be tempted to anchor the tendons, or to suture them to each other. This invariably leads to an imbalance and most frequently to a flexion contracture.
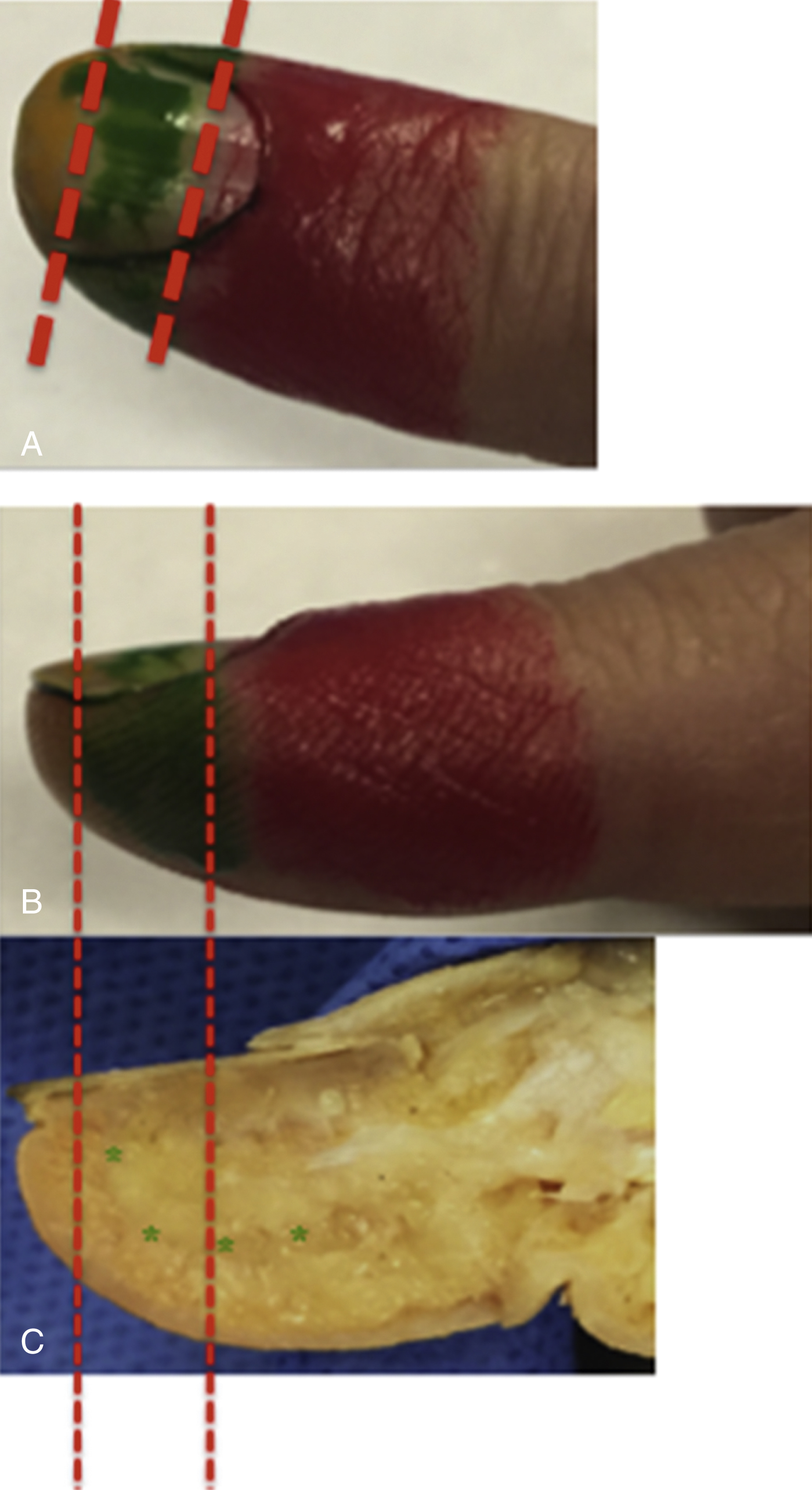
All amputations require attention to the nerve ends. One should take the opportunity of any skeletal shortening to keep the nerve ends long and to transpose them dorsally, away from contact areas.
Options for Skin Cover
If skin cover is required the options are:
- 1.
Skin graft, or
- 2.
Flap cover.
Reconstruction most often involves moving tissue around from one site to another, with the added, vital, phrase “and keeping it alive.” Blood supply is paramount. A skin graft requires a bed capable of angiogensis, the essential process of “take.” “Take” is the establishment of a blood supply to support a graft. A flap requires no such bed – it brings its own blood supply and can be placed over any surface, including metalwork. Provided this principle is observed, the decision can then be taken on what form of cover will best restore function and structure. The concept of the “reconstructive ladder” with its implications that one chooses the simplest reconstruction available, is outdated – one chooses what is appropriate and best restores form and function.
It follows that the surgeon must have in his/her repertoire as large a variety of reconstruction as possible, in order to match the reconstruction to the defect, and patient, and not the other way around. This, incidentally, is another strong reason for involvement of experienced, senior surgeons. All too often this process is left to those with one or two methods at their disposal; this invariably results in the dispensation of a method which the surgeon knows, rather than that which is appropriate.
Skin Grafts
Provided the bed will ensure take, a split-thickness skin graft (STSG) provides excellent temporary cover or permanent cover of a “low priority” area, including a secondary defect, from flap harvest. Many wounds involve crushing or bursting mechanisms and it is difficult, at first view, to be sure of viability unless one is wastefully radical with excision. In such situations, a flap may be the appropriate skin cover but its territory may itself lie in the area of trauma. Proceeding with immediate flap cover may lead to flap loss and failure with waste of a reconstructive option. A skin graft may provide comfort, initiate healing, resolve inflammation, and will keep all other options open.
In some situations, skin graft provides good definitive cover. These include the trailing aspects of digits and the secondary defects from the raising of a flap. It need hardly be added that a flap donor source is chosen from an area that can be closed directly, can take a skin graft, or can be left to heal by secondary intention.
Skin grafts do not provide good definitive cover in the pulp, where accurate, pain-free sensibility and good mechanical properties are required. In such a situation, the skin graft will lead to unacceptable hyperesthesia, poor cosmesis, and troublesome long-term fissuring.
The choice between split- and full-thickness skin graft (FTSG) is a matter of balance of various factors. A full-thickness graft requires a better quality bed, since there is a larger cell population to nourish. Take of a split-skin graft is more reliable on a poorer bed. Conversely, split-skin grafts contract more significantly than full-thickness grafts – an important factor in cover of mobile areas crossing joint creases and anywhere in the growing hand.
Points of Technique
Split-Thickness Skin Graft
- 1.
Donor site: Small grafts can be taken from the hypothenar mound. The skin here is thick enough to permit harvest of the dermis while replacing the epidermis. Larger grafts can be taken from the proximal inner aspect of the forearm, where it can be unattractive and/or tender or from the thigh. With both STSG and FTSG, the opportunity to harvest skin, or indeed any other element, from a finger that is to be discarded should not be lost (the concept of “the bank digit”, see below).
- 2.
A guarded skin graft knife is used, such as the Watson, Humby, Silvers knife or, for larger areas, the electric dermatome.
Full-Thickness Skin Graft
- 1.
Donor site: Avoid harvest from the wrist skin crease – scars here can be misinterpreted as the outcome of self-inflicted wounds and can prove tender and troublesome with the wearing of watches or bracelets. The cubital fossa provides ample skin for most needs in the hand and digits. It is usually hairless, and is in the same bloodless field, which speeds up proceedings and makes harvest more accurate. Hairy donor sites should be avoided – harvest from the groin crease in children before the distribution of pubic hair is evident provides a common pitfall.
- 2.
The graft should be taken thin, without subcutaneous fat, or thinned just before final detachment.
- 3.
The graft should be sutured tense over the recipient site (suture of a graft provides the only instance when suture under tension is permissible) and larger areas require a tie over dressing.
Finally, one may mention the composite graft as a form of skin grafting. This is particularly applicable in the child’s hand, when the section is clean and the segment uncrushed. It is more successful the fresher the injury and the younger the child. The amputated part should be applied rapidly, with minimal dissection of either surface and with accurate alignment of landmarks, such as nail fold and even print ridges. Parents are warned that the method is not guaranteed and that reconstruction may be required if it fails. The part often appears to necrose and perish, only to reveal accurate resurfacing some 3 weeks later when the carapace falls off or is peeled off.
Flap Cover
The indications for flap cover may be summarized:
- 1.
When bone, joint, and tendon are exposed, or when metalwork needs cover. In some situations one has no choice but to apply a skin graft to intact tendon sheath or paratenon, or even direct to cancellous bone where somewhat surprisingly, it frequently takes. These are relative indications – by and large, exposure of such structures requires flap cover.
- 2.
When deeper structures are not exposed and the defect is capable of nourishing a graft, but sensibility, mechanical quality or cosmesis are relevant requirements.
Flaps have been classified in all manner of ways. In the hand, the most relevant classifications are two:
- 1.
The basis of the blood supply – preservation of continuity of blood supply is paramount. This may be either left unidentified in the flap base (e.g., the Hueston flap or the cross finger flap ) or formally dissected free, as in the islanded flaps. In general, the latter type of designs are the more mobile and versatile, but demand a higher level of technical expertise.
- 2.
The presence of sensibility – for classification purposes, one may consider “sensate” flaps those which maintain pulp quality and replace lost pulp with sensate pulp. One should not consider adequately “sensate” the cross finger flap, which regains some sensibility despite the numerous reports of recovery of “excellent” two-point discrimination. , Nor should one consider that the transfer of an island of dorsal skin (e.g., the kite flap) to replace adequate pulp quality sensibility.
On this basis, one may classify the commonly available flaps thus:
- •
Relatively insensate flaps
- •
Kite flap
- •
Delayed flaps: cross finger, thenar, distant flaps, e.g., groin flaps, random flaps
- •
Free venous flaps
- •
- •
Relatively sensate flaps
- •
V–Y advancements
- •
Thenar advancement
- •
Bipedicle homodigital
- •
Homodigital islands (Segmuller, Venkataswami, Joshi )
- •
Heterodigital (Littler )
- •
Free flaps, e.g., hemipulp transfer from toe or from a bank digit. The recovery of sensation is inversely proportional to age in these examples.
- •
This definition of sensate/insensate is a working classification serving to underline the importance of replacing like with like. It sorts out flaps rather too harshly on the basis of restoration of pulp quality sensation. Many studies report recovery of 2-point discrimination approaching normal in flaps that cannot transfer nerve continuity, such as the cross finger flap. , In this context, one should note that our methods of assessment of sensory discrimination remain relatively crude and subject to significant operator variability and subjectivity.
The description of flap qualities is not intended to label any flap superior or inferior to others. All are useful in context and the wise reconstructive surgeon will master all, and will amass a large repertoire on which to draw when analyzing each individual defect. It cannot be repeated too often that each defect will have qualities that will be met by this or that flap, and one should have all at one’s disposal, so as to be able to produce a flap that matches the defect, not the other way around. In this regard, one should resist the tendency to refer to this or that flap as a “workhorse” or to apply the same, favorite, flap to a wide variety of defects. Conversely, it is also ill advised for the inexperienced to be captivated by a clever flap and to resolve to “try” it.
The account below cannot be exhaustive. Representative flaps in each category have been selected which illustrate the principles of selection, technique, flap attributes that form part of the analysis, planning, and execution of skin cover of the digit.
Flaps with Less than Pulp-Quality Sensation
The Kite Flap
This flap was originally designed, with a wide base pedicle, by Holevitch. Vilain and Michon developed this design, narrowing the pedicle to about 1 cm, including the vascular axis, and this design was named the “flag flap.” It was Foucher who islanded the skin flap, denuding the pedicle of skin and conferring a greater degree of mobility as well as the potential for tunneling of the pedicle. The island of skin is raised in a plane just superficial to the extensor tendon parateneon (which must be left intact so as to receive a graft). The pedicle includes the first dorsal metacarpal artery, local veins, as may be found (usually plentiful), and any superficial branches of the radial nerve that are identifiable ( Fig. 46.4 ).