Introduction
The modern management of facial trauma had its origins in the trenches of World War I, when disciplines united to deal with the devastating results of missiles. Plastic surgeons, neurosurgeons, dentists, and anesthetists worked together in a structured environment to deal with this complex situation. A great boost to the management of facial trauma occurred when Paul Tessier successfully advocated the extended multidisciplinary care of the craniofacially deformed.
This chapter deals with trauma to the naso-fronto-orbital region, the middle third of the face, encompassing the upper jaw and zygomas, the mandible, and panfacial fractures.
The principles of treatment are set out for each fracture type and from them flow the descriptions of operative management, conservative management, and long-term care.
Frontal Bone and Naso-orbital Fractures
The frontal bone and naso-orbital region constitute the upper third of the face. Trauma to this region of the face is often accompanied by brain injury and damage to the cranial nerves. The impacting forces may be transmitted to the base of the skull, producing a range of effects from transient loss of consciousness to loss of life. The injuring force may impact directly on the frontal bone, causing blunt or penetrating brain injury. With this in mind, it becomes obvious that the treating surgeon should be part of a team capable of assessing and treating such injuries. The injuries therefore fall into three categories: injuries to the bone without cerebral involvement, externally compound fractures or penetrating wounds with underlying dural and cerebral injury, and internally compound fractures often of the cribriform plate region resulting in a cranionasal fistula with or without cerebrospinal fluid (CSF) leak.
Some of the causes of craniofacial trauma include falls, assaults, sporting injuries, industrial accidents, and missile injuries. The epidemiology varies with the community, so when organizing multidisciplinary care and planning preventative strategies, an understanding of the causes and incidences in a particular community is essential.
Anatomy
The anterior cranial fossa is formed in the front and at the sides by the frontal bones , and they are attached to the facial skeleton at the front nasal, frontomaxillary, and frontozygomatic sutures ( Fig. 34.1 ). The frontal bone also articulates with the ethmoid bone in the anterior cranial fossa, which bone forms part of the orbit and its vertical plate forms part of the nasal septum and indeed is said to play a part in facial development. Laterally, the anterior fossa forms the thin superior orbital plates; they dip down medially to articulate with the cribriform plate of the ethmoid, the posterior articulation of which is the body of the sphenoid bone. The lesser wings of the sphenoid bone form the crescentic posterior borders of the anterior fossa. The optic canal is formed by the two roots of the lesser wing of the sphenoid and runs forward and laterally in the superolateral wall of the sphenoid sinus to the orbital apex.

The complex sphenoid bone is the keystone of the craniofacial skeleton; it forms part of the anterior cranial fossa, the middle cranial fossa, the lateral orbital wall, where its articulation with the zygoma is an important landmark in the reduction of orbitozygomatic fractures, and the infratemporal fossa.
The rest of the facial skeleton is composed of the lacrimal bones, the nasal bones, the ethmoids, the zygomas, the maxillae, and the mandible. It is customary to describe the face as being divided into three thirds. The upper third is formed mostly by the frontal bone, which forms the orbital rooves. The middle third contains the maxillae, zygomas, and the nasoseptal complex with a contribution from the lacrimal bone and the ethmoid. These elements articulate laterally with the zygomatic processes of the temporal bones, and serve as a good measure of the anterior projection of the face. Posteriorly they articulate with the sphenoid to form the orbit and centrally and laterally with the frontal bone. The lower third is said to be formed by the mandible, however this is somewhat of a convention as the body only is in the lower third, the ramus in the middle third, and the temporomandibular joint has a major component formed by the base of skull.
The midfacial skeleton is designed to transmit the powerful forces of mastication to the base of skull. The horizontal elements in the maxilla, the alveolus, and hard palate support three paired vertical buttresses, at the pyriform margins, at the zygomatico-maxillary junction, and more posteriorly at the pterygo-maxillary junction. The two pairs of anterior buttresses provide the best places for internal fixation with plates and screws.
The orbital cavity is formed of seven bones in the shape of a four-sided pyramid. There is a relatively strong rim anteriorly, four more flimsy walls, and a thick apex. The zygoma contributes to the lateral and inferior orbital margins, the lateral orbital wall, and the orbital floor. The maxillary component of the orbital floor medial to the zygoma is thin and delicate (lamina paparycea).
The anterior orbital floor medial to the infraorbital canal is concave downwards, but posterior to the globe it becomes convex upward. A point to be noted for successful restoration of the orbital floor after injury: the medial wall is composed of the lacrimal bone anteriorly and the thin lateral plate of the ethmoid posteriorly.
The paranasal air sinuses are rudimentary at birth and do not reach adult proportions until puberty. The degree of pneumatization varies, particularly that of the frontal sinus. They range from being barely pneumatized to extending superiorly in the frontal bone for a variable distance; laterally they can go as far as the lateral margins of the orbit and also extend into the orbital roof.
The frontonasal ducts open inferomedially and drain into the frontal recess of the nasal cavity.
The ethmoid sinuses constitute an interconnected series of thin-walled cells that lie between the upper lateral nasal cavity and the orbit, and are separated from the orbit by the thin lateral wall. Their roof forms part of the anterior fossa lateral to the cribriform plate. The ethmoid sinuses are related to the maxillary sinuses inferiorly, the frontal sinuses superiorly, and the sphenoid sinuses posteriorly.
The sphenoid sinuses are within the body of the sphenoid and may sometimes spread into the lesser wing of the bone; they are divided by a septum and may be asymmetrical. They lie under the central part of the floor of the anterior fossa and are closely related to the internal carotid artery, the pituitary gland, and the optic nerve. They connect through their anterior wall with the upper nasal cavity.
The maxillary sinuses usually fill the entire body of the maxilla and may extend into the zygoma and below the floor of the nose; their walls are fragile and easily broken. They also are rudimentary at birth.
Management Principles
Management involves investigation and treatment, and should be based on a thorough knowledge of the pathophysiology .
With respect to the cranial cavity , the dura is firmly attached around the cribriform plate through which the filaments of the olfactory nerve pass sheathed by arachnoid. A dural arachnoid tear with a fracture communicating with the nose or paranasal sinuses will lead to CSF leak.
The frontal lobes of the brain are particularly vulnerable to the effects of frontal impact, and by anterior fossa fractures, when the orbital rooves are shattered or buckled. Bilateral frontal lobe injury can result in long-term neuropsychological problems.
The olfactory nerve filaments may be damaged by fractures crossing the cribriform plates resulting in anosmia as well as CSF leak.
The optic nerve may be compressed by a displaced fracture through the optic canal, by shearing forces that devascularize the nerve, by contusion or hematoma within the canal without a fracture, or by direct injury to the orbit.
The orbit itself may be fractured directly or indirectly as part of frontal, nasoethmoid, and midface or zygomatic fractures.
In addition to the pathophysiology, it is essential to have knowledge of the effects resulting from the various mechanisms of injury.
Frontal impact is the most common mechanism of craniofacial injury; it may result in linear fractures or depressed fractures, and the forces may be transmitted to the cranial base and cause fracturing there.
Fractures of the skull base are rarely significant in themselves, however the force required in producing such a fracture is considerable and is often associated with injuries of the soft tissues, brain, cranial nerves, major vessels, etc.
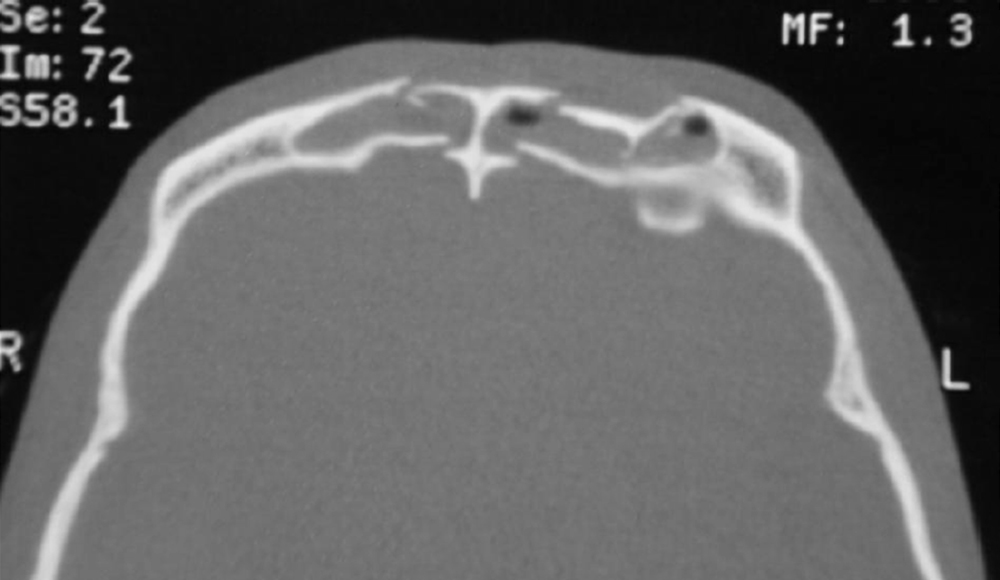
The pattern of fracture lines resulting from blunt trauma follows the points of weakness and in the frontal bone is influenced by the extent of the frontal sinuses and the particular honeycomb structure of the particular sinus ( Fig. 34.2 ). The age of the patient is a significant influence, younger bones being more pliant and less brittle. Fracture patterns, however, rarely conform to a predictable formula.
Penetrating and missile wounds have no particular pattern. The tissue damage resulting from low-velocity penetration is confined to the pathway of the penetrating agent.
Gunshot wounds may be penetrating, perforating or ablative, depending on the velocity and nature of the projectile: the higher the velocity, the greater the damage. High-velocity missiles cause massive avulsion with loss of bone and soft tissue, which is often more extensive than immediately apparent because tissues may be devitalized or injured by the traction of avulsion. The eyes and brain may be injured directly or by vascular injury, which can be delayed. Crushing injuries may result in severe fracturing of the frontal bone and skull base; however, in infants and children the pliability of the bones means that the pattern of fracture is different, with greenstick fractures.
Initial Management
Remember to save the patient! Fractures of the frontal bone and nasoethmoid complex can occur in isolation but more commonly are associated with other facial and systemic trauma. Severe craniofacial injuries often pose an immediate threat to life. Airway obstruction, displaced dentures, and collapse of the mandibular arch with retrodisplacement of the tongue may cause severe hypoxia. Particular care should be taken with cases of frontofacial fractures, where the possibility of a breach in the anterior cranial fossa exists, not to forcibly insufflate the patient or to pass tubes via the nose.
Emergency Assessment and Resuscitation
The primary survey, setting the priorities for management, follows resuscitation, secondary survey, and stabilization, and in the craniofacial region these are: airway, breathing, and circulation.
Airway
The following is a list of problems that may be encountered when trying to secure the airway in severe frontofacial fractures. These same problems also potentially occur in fractures of other regions of the face.
- •
Distortion of the bony facial skeleton
- •
Swelling of the lips, tongue, and floor of mouth
- •
Broken teeth and dentures
- •
Multiple fractures of the mandible with loss of tongue support
- •
Hemorrhage into the soft tissues of the neck hindering cannulation of the airway
- •
Disruption of the anterior cranial fossa
- •
Trismus
- •
Blood and vomit in the airway
- •
Fracture of the larynx
Breathing
Associated chest injuries must be excluded. A brain injury may cause central problems with breathing, as can the overzealous or inappropriate use of pain relief. It therefore behooves the treating team to assess and secure the airway safely and soon. This may be difficult and intubation requires a skilled and experienced anesthetist. Nasal intubation in patients with fractures potentially involving the anterior base of skull should be undertaken with great care. There are various anesthetic strategies to minimize the risks.
Tracheostomy in an awake patient under local anesthesia may be considered, however if the neck tissues are suffused, cricothyroidotomy can be used.
Circulation
Craniofacial injuries, especially those of the midface, can involve severe bleeding from the branches of the external carotid artery that supply the region. Superficial arterial bleeding may be controlled by pressure or by wound exploration and ligation of the bleeding vessel. Packing may control bleeding from the nasal cavity or oropharynx. In the rare case when this cannot be achieved, arterial ligation may be considered, the maxillary artery via a transantral approach and/or ligation of the anterior ethmoidal artery, which is a branch of the internal carotid system and enters the orbit through the medial orbital wall. Interventional radiological techniques are emerging as useful tools in controlling deep bleeding in this area.
Clinical Assessment
This assessment applies to all fractures of the craniofacial skeleton and precedes the special investigations.
The neurological state should be determined early using the Glasgow Coma Scale to record consciousness. It is necessary to examine the cranial nerves, and careful ophthalmological assessment may lead to urgent consultation with an ophthalmologist. Testing for light touch in the various zones identifies facial sensory nerve function. The facial nerve is tested by observation and by response to painful stimuli.
The face should be examined for lacerations and contour deformities. Bruising around the orbits may indicate an anterior fossa fracture, and bruising around the mastoid process indicates a temporal bone fracture. CSF leakage should be suspected, but in the presence of blood and mucus it is very hard to identify with certainty at this early stage.
Jaw movements and the muscles of facial expression are tested; the cervical spine is palpated for tenderness or deformity and the scalp for lacerations and hematomas.
Each facial region should be palpated systematically from the frontal bone to the mandible, looking for evidence of deformity or abnormal movement. Cooter has described a systematic sequence of examination by palpation. Palpation of the inferior orbital margin may help differentiate isolated fractures of the zygoma, where the lateral rim is depressed, from nasomaxillary fractures, where the medial rim is depressed.
The mandible is examined with the patient’s mouth slightly open; the margins of the bones are palpated externally. Intraorally, with a gloved finger the alveolar ridges and the hard palate are palpated. Grasping the maxillary alveolar ridge or pressing on the anterior hard palate behind the teeth and applying a rocking movement while palpating the face with the other hand can elicit abnormal movements of the midface.
Imaging
Early Imaging
- •
Computed tomography (CT) : A cranial CT is performed after the initial resuscitation to assess for possible brain injury. It may be extended to include other areas of suspected injury. Fractures of the anterior fossa may warrant fine-cut bone windows at this stage, but it is the later investigations that will give the definitive information.
- •
Angiography : At this stage, angiography is indicated for penetrating injuries in the region of major vessels or blunt injuries where there is suspicion of vascular damage.
Later Imaging
The detailed diagnostic imaging is usually planned after full clinical investigation is complete. It has become regular practice for the first and principal investigation to be a CT scan, however some of the standard radiographic projections can be most useful and in some circumstances essential (e.g., the panoramic radiograph (orthopantomogram, OPG) that shows the mandible, temporomandibular joints, and teeth).
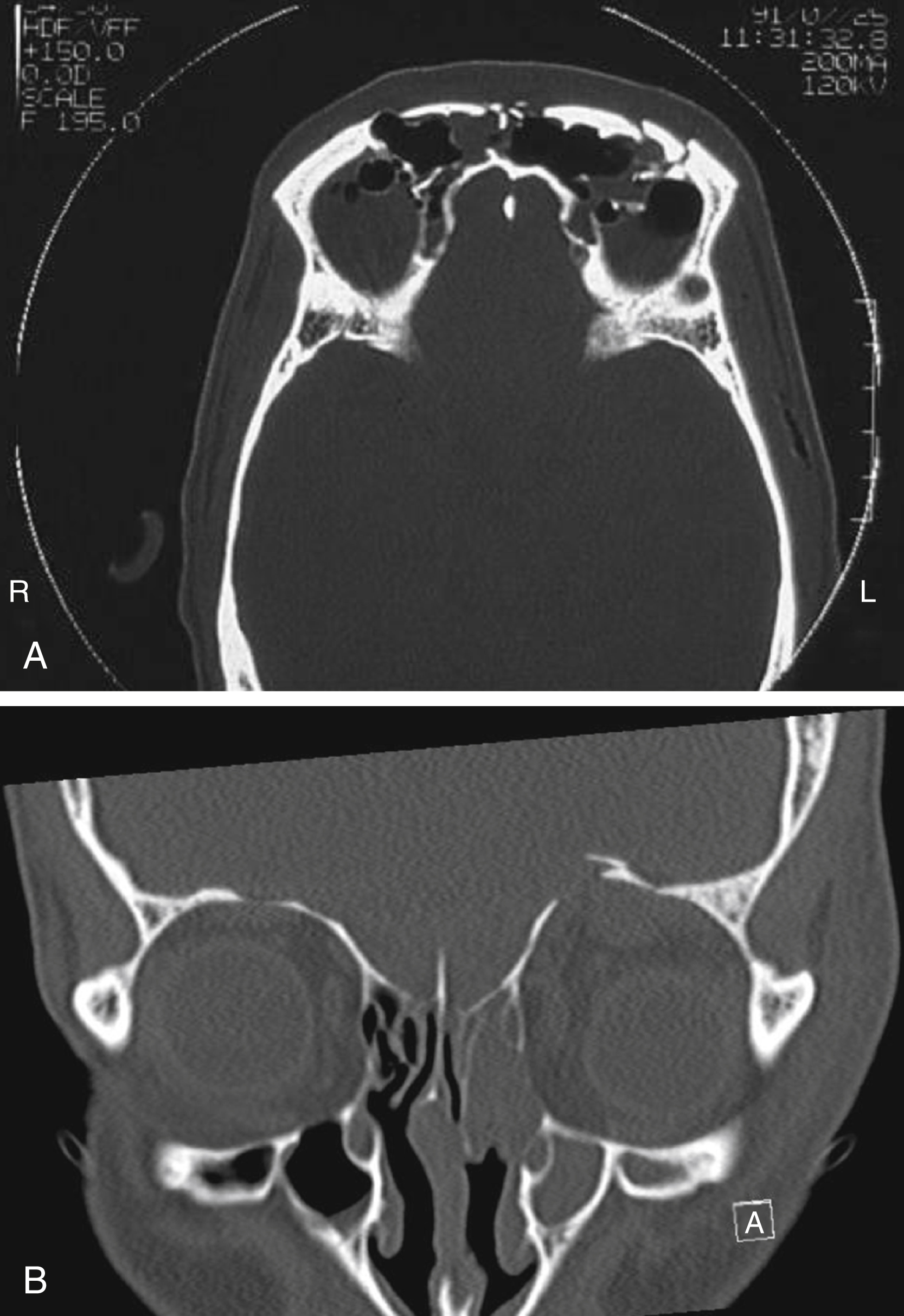
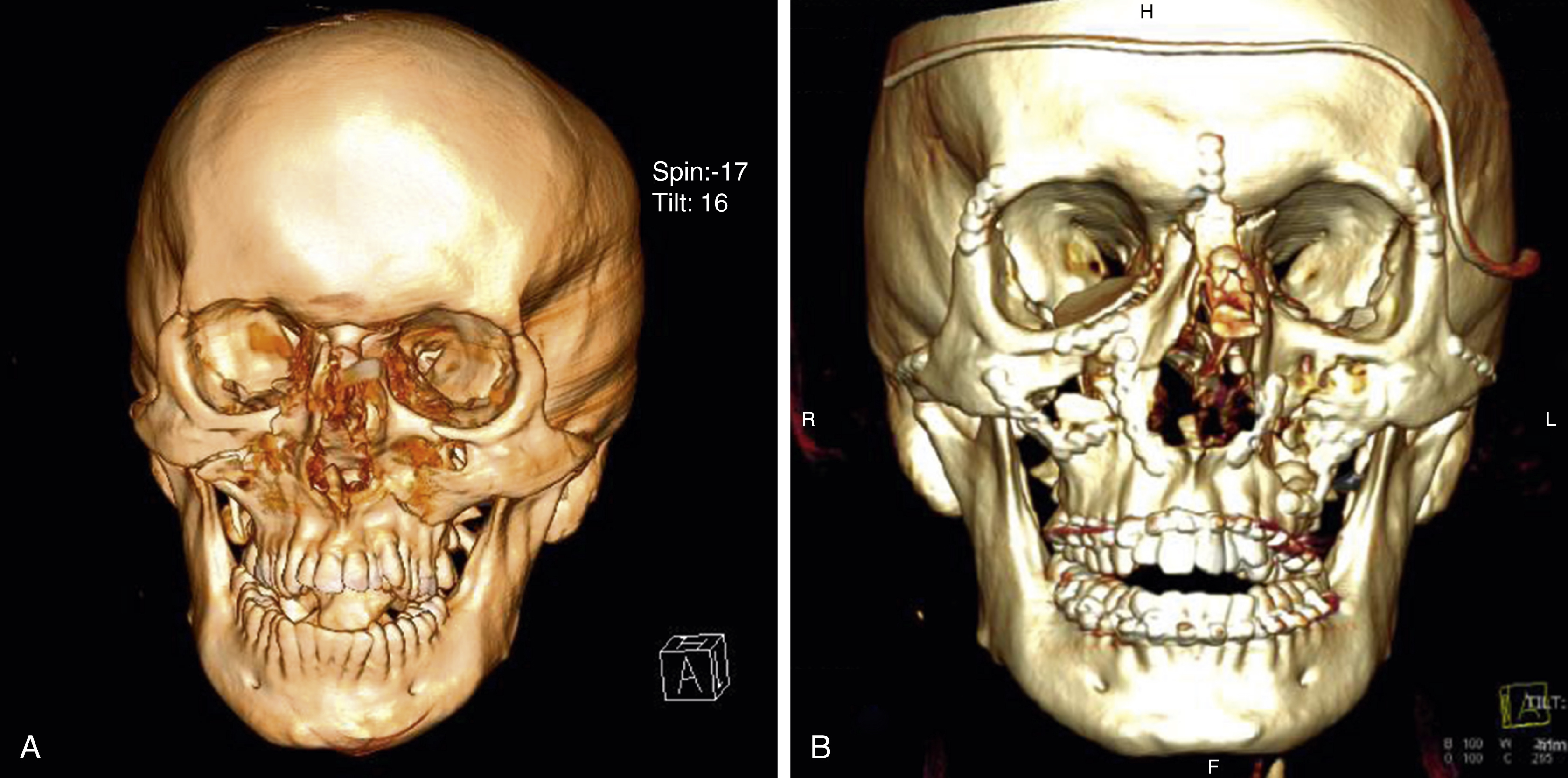
Axial CT scanning is vital in managing severe craniofacial trauma of the frontal and nasoethmoid region. Fine-cut two-dimensional CT is the best method for assessing craniofacial fractures around the fronto-orbito-ethmoid region and the fractures are seen most clearly on the scan at right angles to the bone that is fractured. The acquired CT slices, usually axial, can be used to produce a three-dimensional image of the skeleton and/or soft tissues. These images can be rotated and viewed from all angles and are indispensable for surgical planning.
These data can be used to create solid nylon models of the injured skull, which can be sterilized and used for reference at surgery or for mock surgical planning.
Magnetic resonance imaging (MRI) is often useful later in tracking the origins of CSF leakage. It is used to assess ocular injuries and also to identify nonmetallic foreign material, especially wood.
Definitive Management
Having resuscitated the patient, established the presence of brain injury, established an infection control regimen, and made a clinical and radiological diagnosis, the next step is to establish the priorities in managing the craniofacial injury, in this case the frontal and naso-orbital fractures. Urgent surgical intervention within hours is indicated by the presence of acute neurosurgical problems of intracranial bleeding, penetrating brain injuries or externally compound fractures. Otherwise, delayed treatment is preferred, by an appropriate team after full investigation and planning in the “cold light of day.”
Urgent operative intervention may be necessary for injuries to other body systems, and appropriate discussions will determine what parts of the management can be done simultaneously.
Operative Surgical Principles
Modern craniofacial surgical technique is based on wide exposure of the craniofacial skeleton, the capacity to reduced bony fragments precisely and implement rigid interfragmentary fixation with titanium mini- and microplates. Where there is absence of bone from the trauma, primary bone grafting of defects is undertaken at this stage.
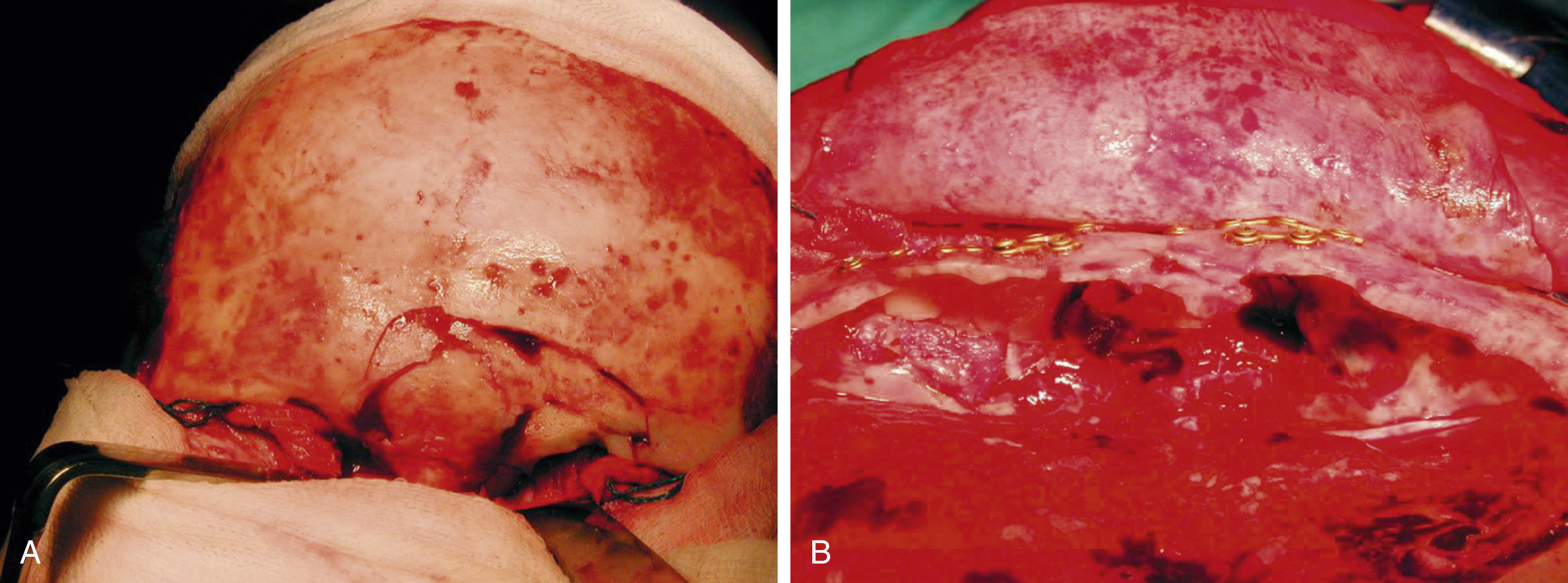
The most effective and commonly used approach to the naso-orbito-frontal region is the coronal scalp flap ( Fig. 34.3 ). The incision is placed well behind the hairline and is made in a wavy or zigzag fashion to better disguise the scar. The flap is raised in the subgaleal plane down to a level about 2 cm above the orbital margins or the site of any fractures of the frontal bones. The dissection then proceeds subpericranially, scraping the bone, and extends over the orbital rim into the orbit. The supraorbital neurovascular bundle is preserved and, if necessary, chiseled out of its canal. More medially, the dissection disconnects the trochlea without obvious deleterious effect.

Laterally, it is important to dissect strictly against the temporal fascia beneath the fatty layer directly superficial to it in order to preserve the frontalis branch of the facial nerve. Within the orbit the periorbita may be safely dissected to within 1 cm of the apex, however in traumatic cases the walls may be breached, the periorbita torn and orbital fat trapped in fracture lines, making dissection more difficult.
Medially, in the region of the glabella, the dissection can be taken down over the nose, anteriorly and posteriorly to the canthal ligaments and nasolacrimal ducts. These structures, so often injured, must be identified and preserved.
Access to the anterior part of the medial orbital wall can be obtained via a transcaruncular approach. The floor is exposed by subciliary eyelid incisions or best by transconjunctival incisions with or without lateral canthotomy.
Bone Grafting
Bone loss demanding early replacement can occur over the frontal sinus, in the orbital walls, especially medial, and the floor, and after comminuted depressed fractures of the nasal pyramid. In the middle third of the face the vertical bony pillars may need to be grafted to secure midfacial height.
The common donor sites for harvesting bone are the iliac crest and medial surface of the ilium, the ribs (both bone and cartilage), and the calvaria. The most important factors for the survival of bone grafts are: rigid fixation, good soft tissue coverage, a well-vascularized bed, and absence of hematoma.
There is a wide selection of all plastic materials to reconstruct the midface and orbits, none of which are favored by this author. In particular, their use in relation to open sinuses should be avoided.
Donor Sites
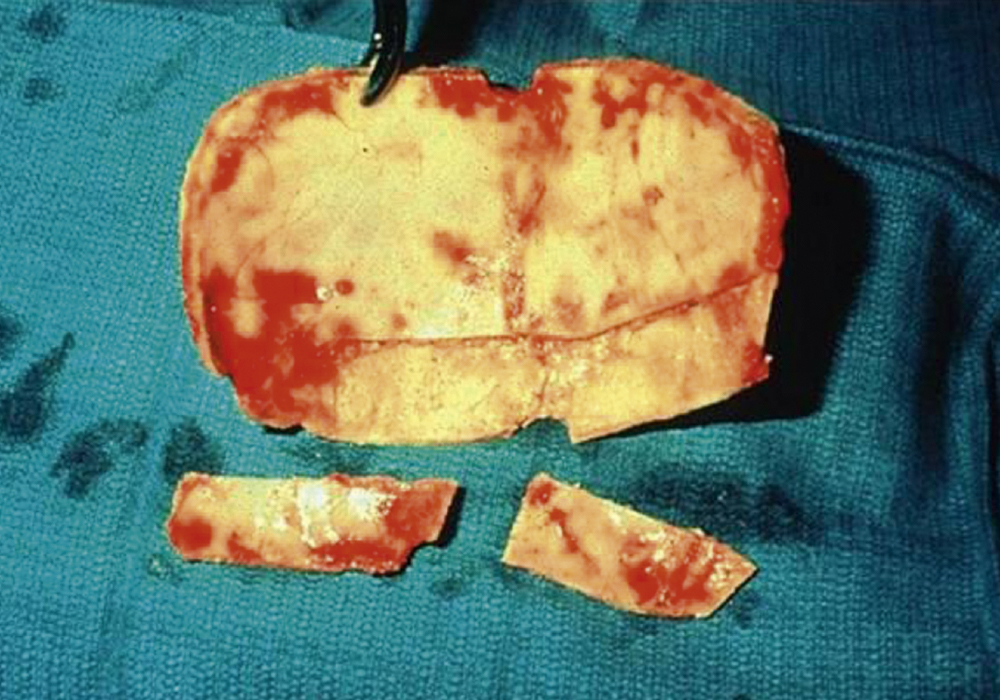
Hip grafts provide strong malleable bone ( Fig. 34.4 ). The inner table can be harvested, and additional cancellous bone scooped out for packing (e.g., the nasofrontal duct). The full thickness of the ilium can be used but it is important to preserve the crest in both adults and children.

Rib grafts are harvested through a submammary incision, cartilage can be taken in the form of the costochondral junction for use in the nose and the temporomandibular joint. Ribs can be used whole or more usually split for calvarial or orbital reconstruction ( Fig. 34.5 ).

Calvarial grafts have the disadvantage of being less malleable than hip or rib grafts. Small portions can be taken from the outer table where the skull is thick enough, obviating a need for extra visible scars, however contour defects of the skull are often a problem as are complications arising from damage to the underlying dura and brain arising from inexperienced operators. The inner table can be harvested when a craniotomy is being performed and the bone is thick enough. Good quantities of high-quality bone can be obtained in this fashion ( Fig. 34.6 ).
Operative Management
This depends on the nature of the fracture pattern. Each case must be managed on its merits but there are a number of consistent and significant variations, such as:
- •
A fracture or the outer table of the frontal sinus with skin intact and a contour defect of the forehead
- •
A compound fracture with the outer table involvement as above
- •
A compound depressed fracture involving the anterior and posterior walls with suspected involvement of dura and brain
- •
Depressed fractures of the frontal bone lateral to the sinus with or without involvement of the orbital roof.
Penetrating wounds need separate consideration due to the extreme risk of contamination.
The simple depressed fracture with a contour defect can be approached via a coronal flap; the fragments can be repositioned and secured with microplates or fine wires. If there is an overlaying or adjacent wound this can be debrided and the same procedure undertaken.
A compound depressed fracture involving both walls is also approached through a coronal scalp flap ( Fig. 34.7 ). A small frontal craniotomy is made above the sinus area to expose the posterior wall, the depressed fracture being approached extradurally. If the dura is torn, the posterior wall of the sinus is nibbled and drilled away (cranialized) and the sinus mucosa meticulously stripped. The dura is repaired in a watertight manner by primary suture and may be augmented by a graft of temporalis fascia or pericranium ( Figs. 34.8–34.10 ).
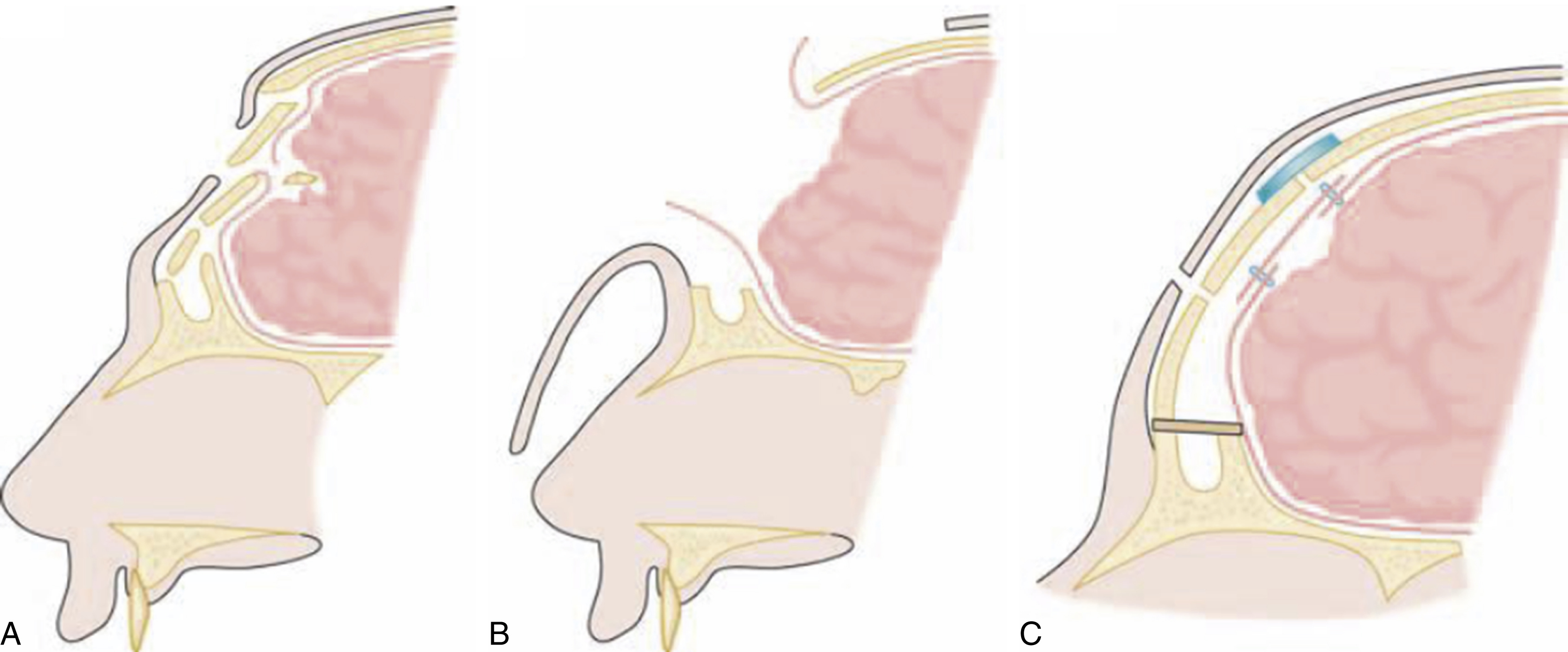
The frontonasal duct can be plugged with muscle and/or bone chips. A pericranial flap pedicled inferiorly is turned in and sutured to the dura in order to seal the frontal sinus. The anterior wall of the sinus is preserved and, if fragmented, treated as in the case of a simple depressed fracture.
Closed anterior and posterior wall fractures associated with CSF leakage are treated expectantly and if the leak persists for more than a week dural repair is performed.
Depressed fractures lateral to the sinuses are usually managed by the neurosurgical team by elevation and if necessary repair of any underlying dural or cerebral damage; however, if the orbital rim and roof is involved, a combined craniofacial approach is often used to reposition the orbital margins and graft the roof.
Penetrating injuries are likely to be associated with contamination along the wound track and consideration must be given to opening the wound track and removing foreign material. Remember that wood is often best visualized by an MRI scan. A frontal craniotomy is performed and if the wound is orbitocranial, the frontal crown can be removed for greater access and replaced. Where there is dural repair under an orbital roof defect, a bone graft will add additional security.
Central depressed fractures of the frontal region may be associated with naso-orbito-ethmoid fractures that extend to the floor of the anterior cranial fossa, hence often complicated by CSF rhinorrhea. A combined neurosurgical/craniofacial approach is needed to deal with this situation. The anterior fossa is explored and the fistula repaired intradurally and the naso-orbito-ethmoid fractures are repaired in sequence from posteriorly to anteriorly with grafts, fixation plates and canthopexies ( Fig. 34.11 ).
Naso-orbito-ethmoid Fractures
These fractures occur as a result of direct trauma to the midface and, although they can occur in isolation, are frequently associated with other craniofacial fractures. Management is challenging because of the intricate and complex skeletal anatomy in close juxtaposition with the canthal ligaments, the nasolacrimal apparatus, and the cribriform plate and brain above. Exposure, reduction and maintaining fixation have always been and still remain difficult.
Classification
These fractures may be unilateral or bilateral, simple or comminuted, closed or compound; they may occur in isolation or in association with more extensive damage to the craniofacial skeleton.
Multiple classifications have been proposed. Markowitz et al proposed Types I–III with increasing measure of complexity in each group. Gruss attempts to relate to the fractures in adjacent bones. The problem with classifications in this area is the complexity and the difficulty of finding a language that reflects the reality of each clinical situation. The author’s view is that the closest method that is useful for measurement and comparison is one of alphanumeric scoring, which quantifies the extent and pattern of bony damage in a global fashion.
Principles of Treatment
Historically, these fractures were treated by closed reduction and external splintage; the results were not only poor but rendered the secondary corrective surgery very difficult. Credit must be given to Mustardé, Dingman and Natvig, and Stranc for identifying the need for open reduction and internal fixation, at the time, with wire. However restricted access and limited radiological assistance with diagnosis meant that the results remained suboptimal.
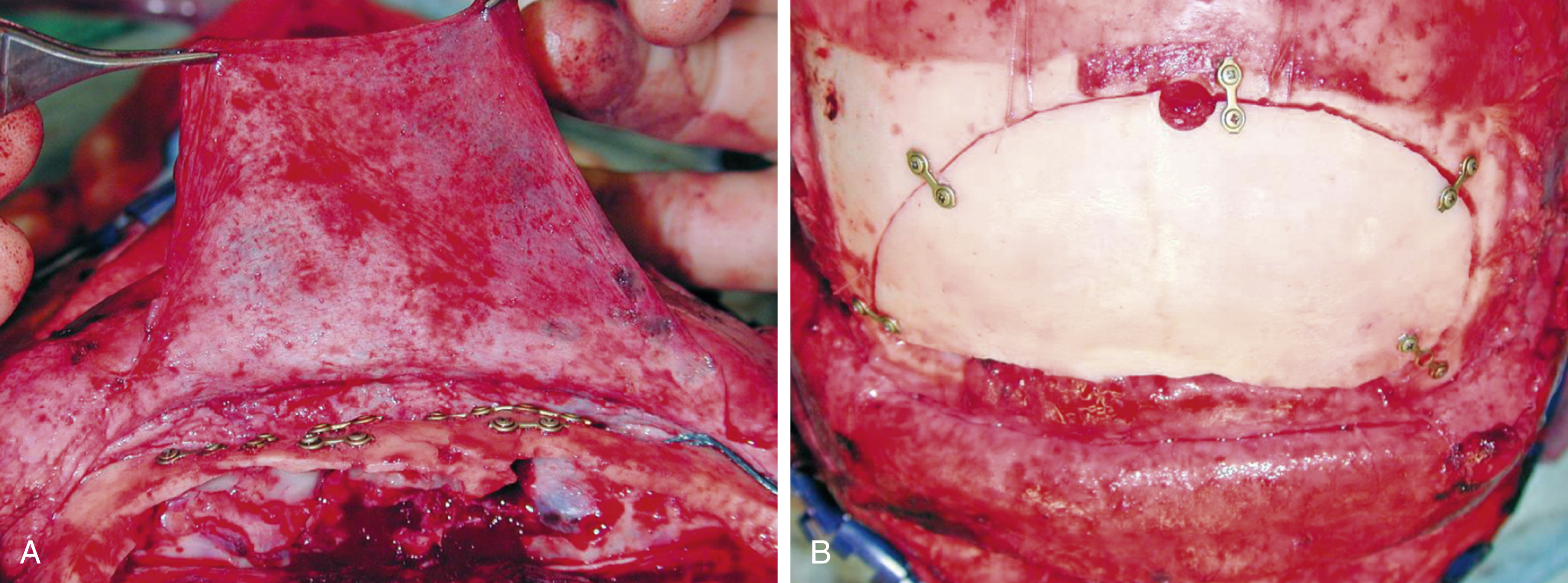
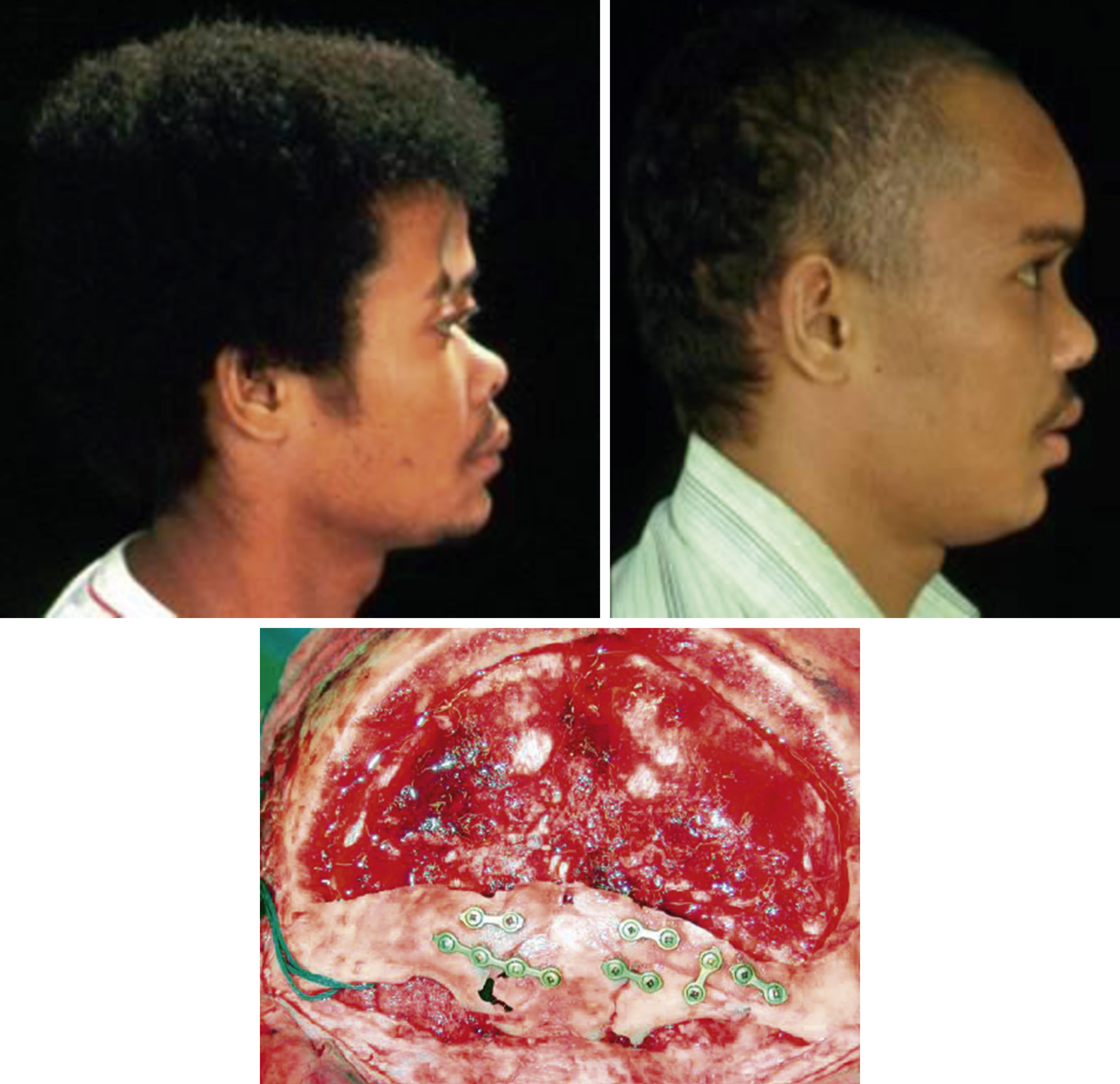
The modern approach is much aided by CT scanning, involves wide exposure using the coronal approach, accurate anatomical reduction becomes possible and fixation with micro- and miniplates and screws ensures stability. In addition, primary bone grafting to delicate medial walls and graft support for the depressed comminuted nasal pyramid has vastly improved patient outcomes ( Fig. 34.12 ).

Operative Management
The coronal scalp flap extended to the supraorbital margin then subperiosteally into the orbit will give tension-free exposure of the medial orbital walls, nasal bones, and frontal processes of the maxillae as well as the orbitofrontal region. Care must be taken to preserve whatever bony attachment there is of the medial canthal ligament.
Transconjunctival incisions or subciliary lower eyelid incisions are used to expose the inferomedial orbital wall and orbital floor. An upper buccal sulcus incision exposes the nasomaxillary buttress and the margins of the pyriform aperture. In the case of compound fractures, local lacerations may be useful for access.
When the naso-orbito-ethmoid complex is fractured and displaced en bloc the fragments can be reduced and controlled by plate and screw fixation to the adjacent stable skeleton. In these cases the canthal attachments in continuity with the major bony fragment and its correct position is restored. In the more severe comminuted cases it is necessary to determine if the canthal ligament is attached to a fragment of bone. If this is so, this attachment is preserved and may be used to maintain the correct intercanthal distance. Transnasal wiring of the canthi is achieved by placing the wires posterior and superior to the lacrimal fossa. The wires are tightened; if there is much loss of bone the wire that is attached to the ligament can be passed through a small bone graft on one or both sides. Reconstruction of the medial walls is usually necessary; the author prefers thinned out inner table of ilium for this purpose. It is important to remember to reconstruct this area before tightening the intercanthal wires thus denying you access! The repair proceeds from back to front ( Figs. 34.13 and 34.14 ).
In the comminuted cases, use of a costochondral graft fixed as a cantilever restores the nasal bridge projection and maintains the soft tissue expansion, which aids and minimizes secondary reconstruction, which is so often necessary in this condition.
With respect to the nasal septum, primary open reduction is not attempted beyond centralization by closed manipulation.
The associated frontal sinus and cranial fractures are repaired at the same time. This implies a team working in harmony. It is the author’s experience that a written preoperative plan setting out the sequence of events from beginning to end of the procedure facilitates harmony.
Management of nasolacrimal injuries does not usually involve early exploration, except where there is an obvious lacrimal system transection in an external laceration. Repairing this over a silicone tube is the preferred option. Despite its intimate proximity to the fractures, the nasolacrimal system is not often damaged, even with severe injuries. When late obstruction does occur, it is usually in the bony nasolacrimal canal. The more accurate the initial reduction, the less need for later dacryocystorhinostomy (see Fig. 34.14 ).
Zygomatico-maxillary Fractures
The face is generally described as having an upper, middle, and lower third. The middle third is formed mostly by the maxillae, zygomatic bones, and the nasoseptal complex. This section deals with fractures of the zygoma and maxilla. As these bones articulate with each other, form part of the orbit, and the tooth-bearing maxillae form the upper jaw which articulates with the base of skull and occludes with the mandible, fractures of this complex may not be simple. Trauma to the middle third of the face has the potential for severe functional, psychosocial, and esthetic consequences. Whereas fractures of the mandible remain the most common form of single facial fracture, the zygoma is the commonest when multiple facial fractures occur. The ratio of males to females remains high, 3–4:1.
Anatomy
The zygoma and maxillae are part of the face between the lower jaw and the base of skull that, together with the nasoethmoid complex, compose the majority of the bones generally described as the middle third. It is important to understand the blood and nerve supply to the maxilla and upper dental arch. This assists with planning, safe incisions, and for understanding the patterns of numbness of the skin and palate associated with maxillary fractures. The greater palatine canal transmits the greater palatine artery and nerve, which supplies all of the bone and mucosa of the hard palate. Branches of the maxillary artery and maxillary nerve pass into the posterior maxilla through small foramina to become the posterior superior alveolar artery and nerve. This nerve supplies the molar teeth with a dental plexus. Branches from the infraorbital artery and nerve enter the anterior maxillary bone from the orbital floor and supply the anterior teeth. Fractures of the orbital floor and the anterior maxilla may result in numbness of the anterior teeth, whereas fractures extending low in the maxilla posterior to the first molar region may result in numbness of the posterior teeth. It is important to know that the maxilla gains blood supply from the gingival attachments to the alveolar bone and through its attachments to the soft palate from the pharyngeal palatine branches of the facial artery and the ascending pharyngeal branches of the external carotid artery. Both the trauma and the surgical exposure may significantly compromise the blood supply to fracture fragments.
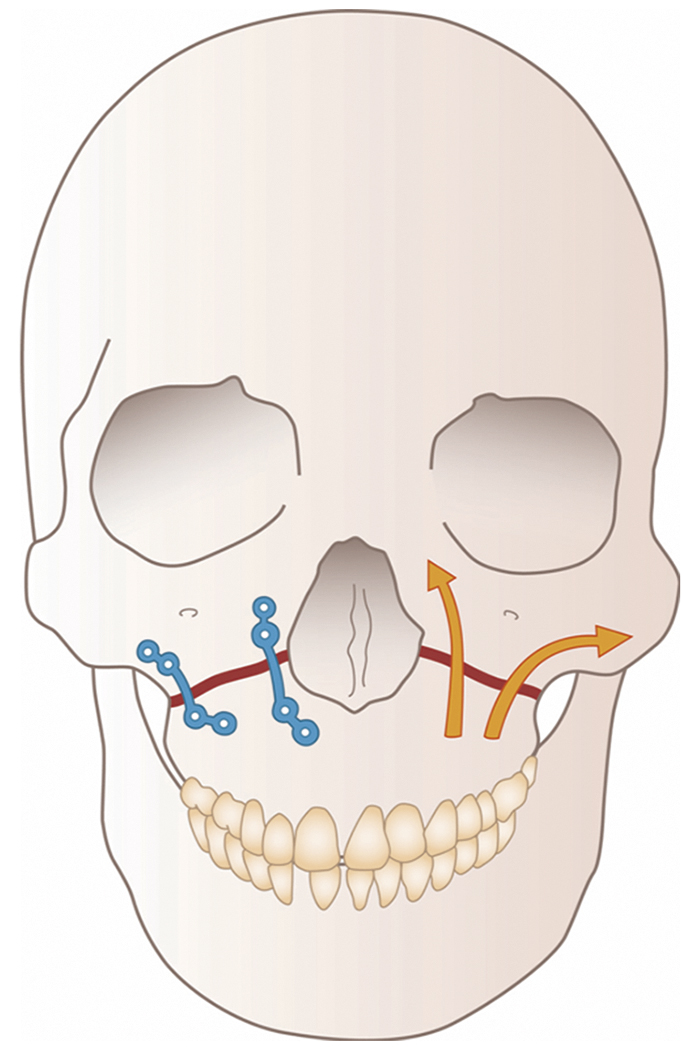
There are strong horizontal elements in the maxillae, alveoli, and hard palate which make up a foundation to support the three paired vertical bony condensations or buttresses ( Fig. 34.15 ). The most anterior of these extends from the dentoalveolar arch in the region of the lateral incisor/canine region superiorly along the pyriform margin to the medial orbital rim and frontomaxillary suture. The middle buttress extends from the first molar tooth to the body of the zygoma and through this bone as the lateral orbital wall to the frontozygomatic suture. The posterior buttress is represented by the attachment of the maxillary tuberosity to the pterygoid plates and hence to the sphenoid bone.

The biomechanical stresses in the midface have been harder to assess than those in the mandible; however, the load paths for distribution of force appear to be the buttresses described above.
The zygoma makes a key contribution to the orbital contour, facial width, and projection. Comprising as it does the inferolateral orbital rim, the zygoma articulates with the frontal bone superiorly, the maxilla inferiorly and medially and with both sphenoid and temporal bones posteriorly and laterally.
Four bony processes radiate from the zygomatic bone, providing strong articulations with the frontal, maxillary, and temporal bones as well as the greater wing of the sphenoid bone. The bony junction between the temporal process of the zygoma and the zygomatic process of the temporal bone constitutes the zygomatic arch. The temporal fascia and masseter muscle are attached to the arch. These muscles are usually considered to be the major deforming force in maintaining displacement of a depressed zygomatic fracture. The superficial temporal vessels and frontal branch of the facial nerve lie immediately superficial to the arch. Deep to it pass the internal maxillary vessels, temporalis muscle and coronoid process. It is important to understand the value of maintaining the zygomatic arch when locating the zygoma appropriately in relation to the skull base in an anteroposterior, vertica, and transverse dimension.
Classification
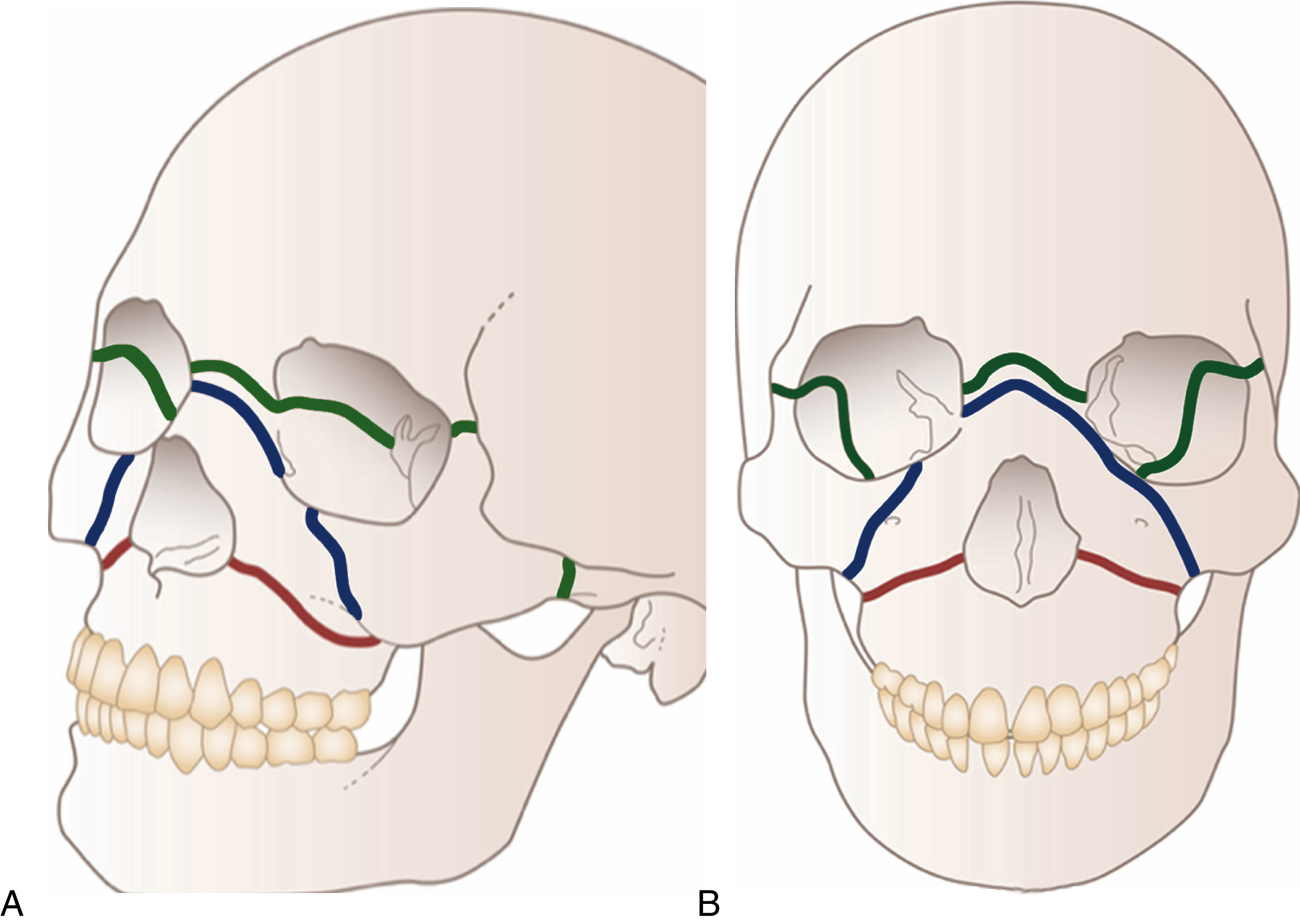
In classifying occlusal fractures of the maxilla we seem to be stuck with Le Fort’s original description. The Le Fort I pattern is a low horizontal fracture through the pyriform aperture and the zygomatic buttresses and pterygoid plate. The Le Fort II fracture has the upper detachment at a fracture line running across the nasal bones, through the inferior orbital rims and through the zygomatic buttresses and pterygoid plates. The Le Fort III pattern has the upper jaw detached from the base of skull at a fracture line running through the nasofrontal suture, ethmoid bone, frontozygomatic suture and arches of the zygomas, and the pterygoid plates.
The language associated with this form of description is now so embedded that it ceases to be scientifically meaningful; it does not take into account the degrees of comminution and displacement of fragments, nor does it mention the parasagittal fractures of the hard palate and the smaller dentoalveolar segment fractures of the upper jaw. It certainly does not relate the severity of the maxillary fracture to other areas of the craniofacial skeleton. It is the author’s belief that alphanumeric classifications are superior in this respect.
Classifications of zygomatic fractures are many and varied. With the advent of CT scanning together with improved methods of operative exposure and fixation of the orbital zygomatic region, the extent rather than the pattern of fracturing was seen to be of greater significance. Gruss recognized the role of the zygomatic arch in accurate reduction and classified these injuries according to the level of bony damage to the zygomatic body and zygomatic arches. Cooter and David quantify the degree of bony comminution of each element of the zygoma as well as the level of displacement of the skeletal articulations.
Clinical Assessment
With respect to fractures of the maxilla , the signs depend on the degree of displacement and comminution and indeed whether the fracture extends into the orbits and skull base, and whether the zygomas are involved as well. Intraoral examination may show the upper dental arch to be intact or it may be fragmented. There may be mobile dental alveolar segments as well. Malocclusion may be evident: the patient may notice it or it may be obvious on inspection. It is important to be mindful of preexisting occlusal disharmony. In the typical fracture of the upper jaw with an intact alveolar arch, posterior and inferior displacement the occlusal surface will result in an open bite.
The external examination shows cheeks that are typically swollen, and there may be bleeding from the nose and bruising. There may also be emphysema from the air forced out of the paranasal sinuses. If the fracture extends into the orbit, swelling and bruising of the eyelids may be a dominant feature. A gloved figure on the hard palate exerting an upward and rocking force may elicit pain, crepitus, and abnormal mobility. Diastases at the fracture sites may be felt at the nasofrontal and frontal zygomatic sutures.
When managing fractures of the zygoma, it is important to record the mechanism, direction, and particularly the force of the impact, as this will assist in understanding the pattern of fracture. These observations may be very important in later medicolegal proceedings, particularly in cases of interpersonal violence. The association of zygomatic fractures with other midface injuries, in particular fractures of the maxilla, has been noted above (see Fig. 34.15 ).
The symptomatology typically relates to the effect of the displaced zygomatic bone on the surrounding soft tissues. The orbital soft tissues manifest swelling, ecchymosed and subconjunctival hemorrhages, particularly laterally. Double vision or blurred vision may be complained of due to orbital soft tissue swelling, ocular dystopia or primary ocular injury. Numbness or altered sensation in the distribution of the infraorbital nerve indicates a fracture in the region of the orbital rim. If the zygoma is medially displaced, trismus and complaints of malocclusion are noted when the arch fractures impinge on the underlying temporalis muscle. Patients sometimes complain of altered occlusion and in this situation occlusal disturbance by extension of the zygomatic fracture into the maxillary alveolar process must be excluded by careful intraoral examination.
Physical examination and especially palpation will readily identify displacement. Observation from above the patient provides an impression of loss of the zygomatic prominence.
The examining fingers are placed on the prominent part of the zygomatic body and will give a comparison with the noninjured side. When there is displacement of the inferior rim, there may be a palpable step at the infraorbital margin and this is usually painful. In isolated fractures of the zygomatic arch there may be a depression which is palpable. When the zygomatic fractures are part of extensive midface fracturing, for example in conjunction with maxillary fractures, the zygomatic arches bow outwards and the anteroposterior projection of the zygomatic prominence is diminished.
Intraoral examination shows bruising in the upper buccal sulcus. Alveolar extensions of the fracture or malocclusion caused by trismus or associated with midfacial and mandibular fractures can be noted at this time.
It is important to have a detailed ophthalmological examination similar to that necessary in isolated fractures of the orbital walls.
Imaging
Fractures of the middle third of the face were once investigated by plain radiology. This has almost completely disappeared and the most useful radiological investigation has become the CT scan with axial, coronal, and three-dimensional reformatting. This is the standard radiological examination for fractures of the upper jaw and orbit and all but the most simple fractures of the zygoma.
Axial cuts show fractures of the posterior wall of the maxillary antrum and of the pterygoid plates. It is possible to identify midline fractures of the hard palate as well as dentoalveolar segmental fractures. Coronal CT scans of the midface give detailed information of the anterior maxilla and the relationships with nasoethmoid and orbitozygomatic fractures. When the fractures are primarily of the orbitozygomatic region, then the radiological analysis is similar to that described in the section on orbital fractures.
Principles of Management
The mainstay of surgical treatment for zygomatic fractures was for many years the Gillies technique of elevating by leverage from an incision in the hair-bearing scalp of the temple. The Dingman and Natvig variation or elevation from a lateral eyebrow incision is a more useful and elegant method as it also affords access to the lateral orbital wall and allows for frontozygomatic interfragment fixation.
An intraoral upper buccal sulcus approach gives access to the arch and body of the bone which can be elevated and fixation can be made at the zygomatico-maxillary buttress. Because of the pull of the masseter muscle, it became common practice, in order to prevent relapse, to add fixation using a wire at the frontozygomatic suture. It is now standard practice to employ miniplate fixation. Miniplate or microplate fixation together with wide operative exposure of the orbitozygomatic skeleton allows anatomical restoration of the zygomatic prominence with fewer positional disturbances of the globe, such as enophthalmos and vertical global dystopia.
Following clinical examination and CT confirmation of the fracture pattern, it becomes important to identify fracturing and comminution in and around the zygomatico-maxillary buttress and the inferior orbital rim, disruptions of the arch and at the zygomatico-frontal suture. Because of the deforming and displacing effects of the masseter muscle, the placement of adequate mini- or microplate fixation is necessary. The techniques of exposure, reduction, and fixation are now well described. It becomes logical to subdivide fractures of the zygoma to those where there is no orbital wall involvement (the isolated zygomatic arch fracture) and the more common orbitozygomatic fracture and also those associated with other midfacial fractures, or the panfacial fracture.
Isolated Zygomatic Arch Fractures
These result in the main from low-velocity injuries and the characteristic symptoms are those of trismus and a depression at the site of impact. This injury is usually best treated by the Gillies technique of closed reduction. A short oblique incision in the hair-bearing temple allows passage of an elevator deep to the temporalis fascia behind the depressed arch. This technique produces a stable reduction in the majority of cases. If the arch fracture is not corrected, the cosmetic deformity remains and in extreme cases there is some long-term disturbance of jaw opening.
Orbitozygomatic Fractures
An undisplaced fracture does not need operative intervention. Displaced orbitozygomatic fractures require careful open reduction and internal fixation on an individualized basis. Exposure via an eyebrow incision, a lower eyelid subciliary skin muscle flap or transconjunctival incision reveals the zygomatico-frontal suture, lateral orbital wall inferior orbital rim, orbital floor, and interior zygomatic arch. An upper buccal vestibular incision permits exposure of the zygomatico-maxillary articulation and anterior attachment of the masseter muscle to the zygoma. Following fracture mobilization and elevation, either by the intraoral approach or by using the elevator through the eyebrow approach, an anatomical restoration is achieved by visualizing the zygomatic articulations and checking the alignment of the zygoma with the greater wing of sphenoid. Miniplate fixation in the zygomatico-maxillary buttress is effective, however there may be comminution in this area and sometimes the bony attachments of the plate are thin. The zygomatico-frontal suture on its own is often not enough but it does provide the strongest bone for miniplate fixation. Two-site fixation will provide sufficient stability in the majority of fractures. When the orbital floor needs exploring then the orbital rim can be plated as well through the lower lid or transconjunctival incision.
Comminuted and grossly displaced orbitozygomatic fractures seldom occur in isolation and are almost always the result of high-velocity impacts producing major midface fractures involving the maxillae. In those cases, recognizing the disruption and restoring the arch is key to restoration of zygomatic projection and hence a very good marker for fixation of adjacent fractured bones. In these cases a coronal scalp flap facilitates exposure, mobilization, and reduction of the arch fractures.
Comminution and loss of bone at the major articulations, the anterior maxillary wall, the orbital floor, and the lateral orbital wall demands careful operative exposure, reduction, and reconstruction by primary bone grafting to avoid enophthalmos and orbito-ocular dystopia.
When dealing with maxillary fractures , it is important to have a preoperative dental assessment. Impressions of the dental arches and teeth can be used to cast a plaster model which is then cut through the site of the fractures. Restoration of the premorbid occlusion can be planned and an acrylic bite wafer constructed, which can be used intraoperatively and postoperatively to maintain correct occlusal relationships.
There is some discussion in the literature about the timing of definitive treatment of maxillary fractures. The desirability of performing surgical correction of midface fracture as early as possible after injuring has been championed by Gruss and Mackinnon and Manson et al, their argument being that early accurate bony reconstruction will prevent the development of soft tissue contractures and hence post-traumatic deformity.
It is the author’s belief that there are other factors that must be considered when deciding on the correct timing of surgery.
The foremost of these is consideration of the priorities of management of other injuries, such as associated brain injuries and other associated limb and intraabdominal problems. It is also useful to have time to properly plan and assemble an operative team to be able to give the appropriate time and expertise to the restoration of the facial injury.
Airway management may be compromised with other jaw fractures and great care needs to be taken when considering placement of endotracheal tubes at the time of surgery. Particular care should be taken with panfacial fractures, which may extend through the cranial base. Where there is massive craniofacial disruption with hemorrhage then there is a role for tracheotomy.
Fracture reduction by disimpaction used to be carried out using somewhat brutal forceps inserted with one prong in the nasal cavity, the other in the oral cavity so as to grip the palate bilaterally. It is possible to inflict further damage with this instrument. With the advent of wider exposure through coronal, buccal, and conjunctival approaches, more delicate instrumentation can be used to disimpact the fracture sites.
Stabilization of fractures is of course now achieved with miniplate fixation and when there is comminution and loss of bone at the buttresses, primary bone grafting is performed.
Once the impacted displaced maxilla has been reduced, the upper and lower jaws are stabilized in the pretraumatic occlusion using arch bars, the wafer, and intermaxillary wiring. Where the zygomas are also fractured, these should be reduced as described above. They then provide a reference point for reestablishing the vertical buttresses.
In the case of an uncomplicated Le Fort I fracture, the vertical height can be determined easily by opposing the vertical buttresses at the pyriform margin and zygomatico-maxillary region, which can then be plated. Even when there are other fractures of the midface, at least one of the four anterior vertical midface buttresses will usually not be severely comminuted and so provide a guide for the correct vertical relationship. Once this has been established, miniplates are used to stabilize the reduced fracture using at least two screws on either side of the fracture. If there is loss of bone then bone grafting may be needed in one or more of these vertical buttresses. Once the vertical height has been established and stabilized, with or without bone graft, the maxillary fixation can be released, the surgical fields irrigated, and the wounds closed. The jaw opening is controlled with light elastics and the wafer removed after several days when the patient is able to bite in the correct position ( Figs. 34.16–34.18 ).