Fig. 28.1
Set of disposable FAMI ™ cannulas
Each blunt-tipped cannula is made for a muscle or group of muscle or bone surface (Table 28.1). It is obvious that the beginner surgeon in FAMI™ cannot practice on his or her patients. He or she needs to understand perfectly the anatomical details and 3D relationship between approach port and muscle origin or insertion. Training on frozen preserved human faces followed by dissection is mandatory to double-check the safety of the injections.
Table 28.1
List the cannulas developed for a full face FAMI on the basis of one cannula for one specific muscle
Cannulas | Object |
|---|---|
Cannula # I | For the levator labii superioris muscles |
Cannula # II | For the orbicularis oculii muscle |
Cannula # III | For the risorius muscle |
Cannula # IIIa | For the platysma in lateral part of the Cheek |
Cannula # IV | For the zygomaticus minor cheek part |
Cannula # IVa | For the zygomaticus minor lip part |
Cannula # V | For the buccinator, depressor anguli oris |
Cannula # Va | For the platysma and neck bands |
Cannula # VI | For the corrugators and procerus muscle |
Cannula #VII | For the depressor labii inferioris and mentalis |
Cannula # IX | Dissecting cannula for scar undermining |
Cannula # X | For the zygomaticus major |
Cannulas P1.P2.P3 | For subperiosteal injections |
The FAMI™ ultracentrifuge includes three preset programs 1, 2, and 3 which correspond to the three different structures, bone, muscles, and fat pads. In FAMI™, we get a good concentration of stromal vascular fraction (SVF) in destroying the adult fat cells. This concept by itself makes a big difference between FAMI™ and lipofilling of Fournier, Guerrerosantos, or Coleman. After this text, the reader will better understand the numerous differences which prove the originality of the FAMI™ technique and why it will be the ultimate fat transfer technique of the future.
28.2.2 Procedure
Numerous articles have been published on fat injection; therefore, we will only describe the points that make FAMI™ so specific. After analysis of aging changes or other defects, an individualized plan of the injection pattern to be used is formulated, selecting subperiosteal (bone), intramuscular, and fat pad locations to be addressed and noted on a form.
Subperiosteal injections are usually 0.5–1.0 mL in one pass, intramuscular 1.0–2.0 mL with exceptions (procerus 0.5 mL, mentalis 3.0 mL, platysma up to 5.0 mL) in two passes, and fat pads 1.0–5.0 cc in three to five passes. A circulator records the graft volumes as they are administered.
28.2.3 Harvesting
Diet-resistant donor areas are chosen with the patient in standing position, most frequently using the inner part of the knees or the love handles region that are genetically present in men and women.
Injection with Klein’s solution begins within the deep supra-aponeurotica plane followed by the subcutaneous space, making the central fat deposit relatively free of anesthetic solution. (According to Klein, 0.1 % lidocaine with 1:1,000,000 epinephrine into the subcutaneous tissues of a concentration of 35 mg/kg is safe.) The disposable harvesting cannula is connected to a 10 mL Luer-Lok syringe. A negative pressure in the syringe body is created by pulling the syringe plunger two 1 mL graduations. The harvesting FAMI™ cannula of the set is made with a round-tipped, two-hole stainless steel tube making the samples bloodless. The fatty connective tissue is gently aspirated with a movement going back and forth to reproduce a multiple biopsy piercing more than a conventional liposuction.
28.2.4 Centrifugation
To prevent any leakage and air mixture during the spinning process, an aluminum cap seals the 10 cc syringes. After removal of the syringe from the centrifuge, we can observe (Fig. 28.2), on top, a layer of less density, yellow in color, mainly composed of the oil of destroyed fat cells; this layer can measure up to 5 cc in program 1 (bone program). In the bottom, the pink layer is mainly constituted of blood, lidocaine, and saline with debris. The middle layer is composed of an accumulation of tissues: free fat cells, fat cells within a stromal vascular fraction (SVF) that contain the mesenchymal stem cells, and a lower white crescent of pure collagen.


Fig. 28.2
After centrifuging, the top layer is of less density, yellow in color, and mainly composed of the oil of destroyed fat cells. The middle layer is composed of an accumulation of tissues: free fat cells, fat cells within a stromal vascular fraction (SVF) that contain the mesenchymal stem cells, and a lower white crescent of pure collagen. The bottom layer is pink and is mainly constituted of blood, lidocaine, and saline with debris
Sticking to the opening of the syringe, an accumulation of platelets is present in bloody samples. This fraction is always removed when present; it contains PGF or platelet growth factors which are added to the SVF.
Different programs are used according to the facial tissue to be augmented: bone, muscle, or fat pad (Table 28.2). Lipoaspirates centrifuged at higher G force (13,680) tend to be more liquid and are injectable subperiosteally. Intermediate G force (5,000) is used for muscle injection. Lower G force (1,200) processing is done when larger-volume corrections with lobulated fat aggregations are desired, such as in the fat pads.
Table 28.2
Shows the different g-force applied on lipoaspirates to obtain purified tissues for restoration of bone, muscle, and fat pads
Spinning speed/1 or 2 min in g-forcea | Tissue to repair |
|---|---|
10,000–13,000 G | Subperiosteal |
5,000–6,000 G | Muscles |
1,000 G | Fat pads |
28.2.5 Anesthesia
Complete trigeminal sensory nerve block is administered using Naropin 0.5 % (ropivacaine 5 mg/100 ml—AstraZeneca) along with cervical sensory branches if neck bands are to be addressed. Lorazepam 0.5 mg PO or similar sedative and clonidine 0.1–0.2 mg are useful adjuncts preoperatively.
28.2.6 Access Ports
Access ports (Fig. 28.3) are made with a tapered tip awl, which minimizes any dermal bleeding and avoids suture. From any of them, one can enter the origin or the insertion of each muscle with fewer traumas. These locations are free of vessels and nerves. Rarely bleeding coming from severed venous capillaries is stopped by few minute compressions.
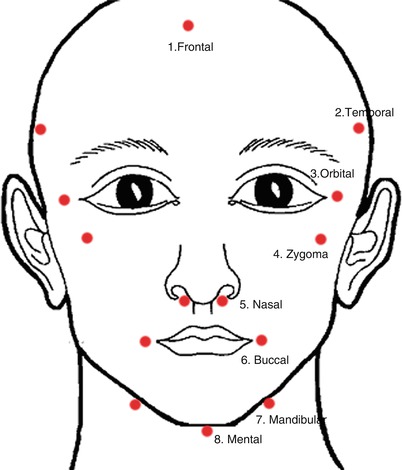
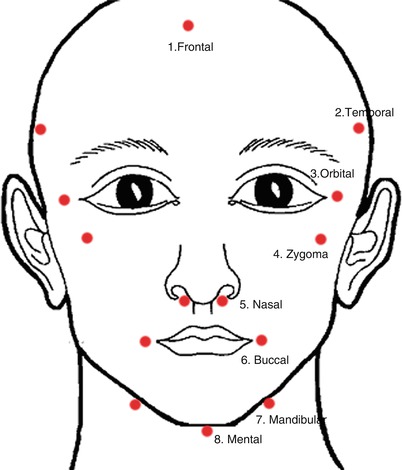
Fig 28.3
Schematic drawing of the 13 basic access ports
28.2.7 Graft Placement
The processed lipoaspirates are transferred into 1 and 3 mL Luer-Lok syringes for injection with the appropriate cannula. Acquired technical skill and a detailed knowledge of the anatomy are necessary to successfully place the grafts (Table 28.3).
Table 28.3
Summary of injection from access ports
Approach site | Subperiosteal | Muscle | Fat pad |
|---|---|---|---|
1. Frontal | Frontalis corrugator procerus | ||
2. Temporal | Temporal crest | Superficial temporal | |
3. Orbital | Orbital rim | Orbicularis oculii zygomaticus minor | Brow/Charpy’s/ROOF SOOF |
4. Zygoma | Zygoma, zygoma orbital process, zygomatic arch | ||
5. Nasal | Nasal frame, nasal spine | Levator labii superior, Lev labii sup alaque nasi | |
6. Oral commissure | Alveolus superior and inferior | Levator anguli oris zygomaticus major orbicularis oris buccinator platysma | Bichat/buccal FP |
Buccinator FP | |||
7. Mandibular | Mandibular body | Platysma (neck bands) depressor anguli oris depressor labii inferioris, digastric | |
8. Mental | Chin | Mentalis | Submental FP |
How does the surgeon know that the cannula is inside the muscle envelope? This is a very recurrent question asked by non-anatomist surgeons. Under the facial skin, there is no dead space. If the cannula fails to enter the superficial musculoaponeurotic system (SMAS) envelope of each muscle, it is very difficult to inject due to the soft tissue resistance. Correct intramuscular placement is associated with no resistance at all; as the plunger is depressed, it becomes very easy to inject with each withdrawal. 1 or 2 passes are used for each muscle. The real quantity is evaluated with little experience. We feel a little resistance when the muscle is full. The systematization of the injections, from periosteum to skin, more superficial anatomical plane after deeper anatomical plane, is one more characteristic of the FAMI™ procedure.
28.2.8 Postoperative Care
Benzoin solution is applied after the procedure, and the patient is asked not to wash his or her face for 3 days. In the immediate postoperative period, the patient leaves the facility with no dressing and little postoperative discomfort. The bruising will appear on the first postoperative day around the approach sites and in the lower lid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








