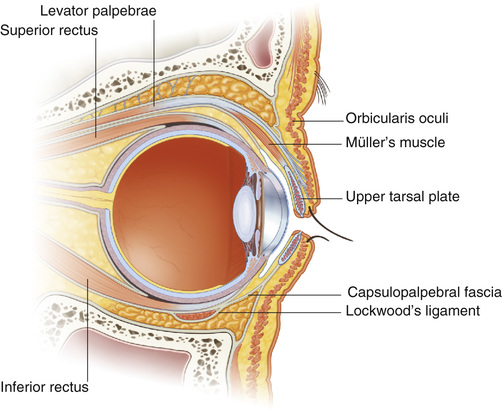
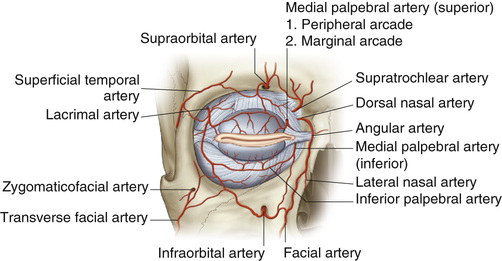
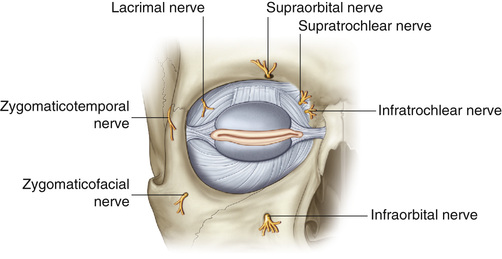
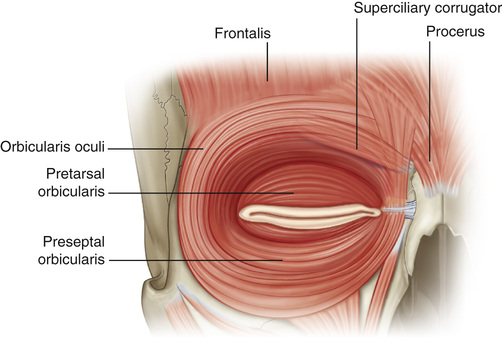
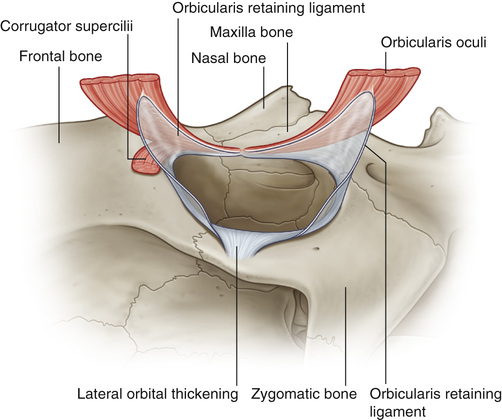
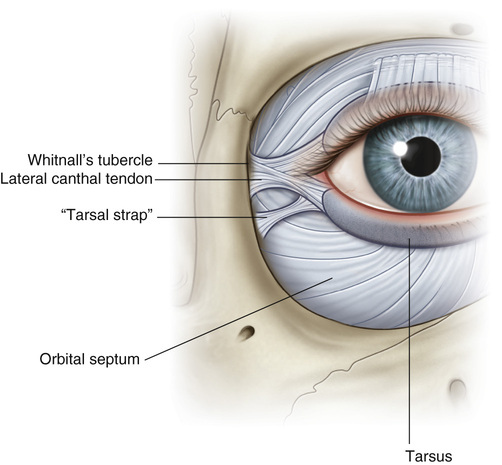
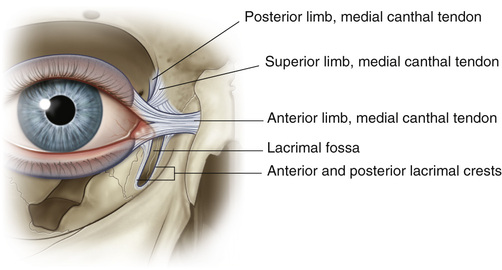
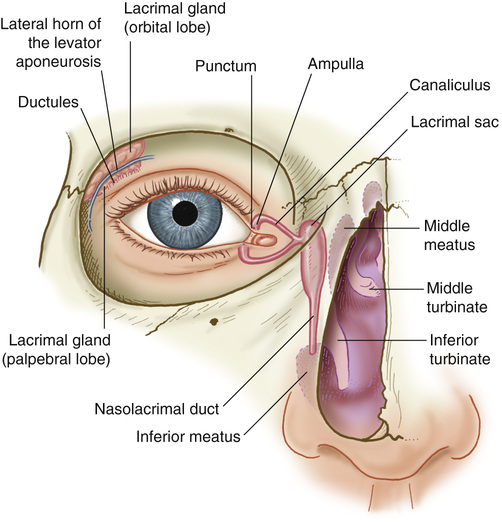
1. Upper eyelid layers (superficial to deep) 2. Lower eyelid layers (superficial to deep) 3. Orbital fat ▪ Two compartments: Medial and central ▪ Medial fat is pale in color. ▪ No lateral compartment, because the lacrimal gland occupies the lateral portion ▪ Three compartments: Medial, central, and lateral ▪ Medial fat is pale in color. ▪ Medial and central compartments separated by the inferior oblique m. 4. Vascular supply of the eyelids (see Figure 26.2) • Branches of the ophthalmic a. (medially) and lacrimal a. (laterally) via the internal carotid artery ▪ Form the medial and lateral palpebral a., which anastomose to create the arterial arcades of the lid ▪ The upper eyelid has two arterial arcades. ○ Marginal arcade runs along the surface of the tarsal plate, 2 to 3 mm above the eyelid margin ▪ The lower eyelid has only one well-developed marginal arcade. 5. Sensory innervation of the eyelids (see Figure 26.3): Via the ophthalmic (V1) and maxillary (V2) divisions of the trigeminal n. • Supraorbital n.: Upper eyelid and forehead skin ▪ Exits the orbit through the supraorbital notch or supraorbital foramen • Supratrochlear n.: Central forehead skin and medial upper eyelid • Infratrochlear n.: Medial upper and lower eyelid and medial canthal tendon • Lacrimal n.: Lacrimal gland, conjunctiva, and lateral portion of the upper eyelid • Zygomaticofacial n.: Lateral fat pad of the lower eyelid and lateral skin of the lower eyelid • Infraorbital n.: Lower eyelid, cheek, and upper lip 6. Orbicularis oculi m. (see Figure 26.4) • Divided into three anatomical portions: Orbital, preseptal, and pretarsal ▪ The orbital orbicularis m. is used in forced eyelid closure. ▪ Avoid injury to the pretarsal orbicularis. • A connective tissue structure that functions to contain the orbital contents • Attaches peripherally at the orbital rim via the arcus marginalis (the periosteal extension of the septum) and fuses centrally with the lid retractors at tarsal plates at the lid margins ▪ A transconjunctival approach to the lid/orbit can be performed in a pre- or postseptal plane. ▪ Originates at the orbital apex from the lesser wing of the sphenoid and travels horizontally until it reaches the Whitnall ligament, where it then changes to a more vertical direction before inserting onto the upper eyelid tarsal plate, orbital septum, and dermis via an aponeurosis ○ Müller’s muscle lies directly posterior to the levator m., superior to the tarsus. ▪ Motor innervation via the oculomotor n. (cranial n. [CN] III). ▪ Sympathetic smooth muscle of the upper eyelid ▪ Arises from the levator complex and inserts directly on the tarsus ▪ Positioned posterior to the levator m., directly superior to the tarsus ▪ Resection of Müller’s m. can provide 2 mm of eyelid elevation. ▪ Makes up the anteriosuperior portion of the lower eyelid retractors distal to the Lockwood ligament ▪ Divided during the transconjunctival incision • Located between the medial and central fat compartments of the lower eyelid, deep to the periosteum • Vulnerable to injury when performing fat excision or fat compartment manipulation during lower blepharoplasty or via inadvertent resection, cauterization, scarring, hemorrhage, edema, or suture injury while repairing the septum ▪ Depending on the extent of injury, symptoms, including diplopia, can be transient or permanent. 10. Orbitomalar ligament/orbicularis retaining ligament (see Figure 26.5) • Contributes to the lateral canthal ligament • Release is required to obtain access to the midface when approaching it from the lower eyelid. • Attaches laterally to the orbit at Whitnall’s tubercle (lateral orbital tubercle) • Analogous to the Whitnall ligament in the upper eyelid 13. Canthal tendons (see Figures 26.6 and 26.7) • Medial canthal tendon (or medial palpebral ligament) ▪ Fibrous band that is continuous with the tarsal plates and attaches the lid to the orbital rim ▪ Three limbs: Anterior, posterior, and superior ○ Posterior, or deep limb, attaches to the posterior lacrimal crest ▪ Intimately related to the pretarsal and preseptal orbicular oculi m. and lacrimal system • Lateral canthal tendon (or lateral palpebral ligament) 1. The lacrimal drainage system (see Figure 26.8) • Consists of the lacrima gland, punctum, ampulla, canaliculi, lacrimal sac, and nasolacrimal duct 2. Eyelids open • The lacrimal sac is collapsed and empty, and the canaliculi are patent. • The lacrimal puncta are closed. ▪ The canaliculi open to allow collection of tears. ▪ Tears are milked lateral to medial ▪ The deep heads of the preseptal muscles contract, which ○ Shortens the canaliculi and closes their ampullae. 5. Lacrimal pump failure can be caused by anatomic obstruction and/or functional failure. • Anatomical obstruction may occur at any point along the lacrimal drainage pathway and may be congenital or acquired. ▪ Primary acquired lacrimal duct obstruction: Occurs in elderly patients secondary to fibrosis ▪ Secondary acquired obstruction may be caused by tumors, trauma, or mechanical obstruction. • Jones tests: Two tests used to evaluate for and discern among functional and obstructive etiologies of poor tear flow ▪ Jones-I test: Fluorescein dye is injected into the punctum, and the examiner looks for presence of fluorescein dye drainage from the nose. ○ A positive test means that there is drainage. ▪ Jones-II test: Performed after a negative Jones-I test and involves cannulation of the punctum and irrigation with 1 mL of saline 7. Treatment options for lacrimal pump failure • Can perform nasolacrimal duct dilation or stent placement in cases of distal functional pump failure. ▪ Contraindicated in cases of complete obstruction • Conjunctivodacryocystorhinostomy (CDCR): Performed in cases of flaccid canaliculi, paralysis of the lacrimal pump, and when the site of obstruction is proximal (punctum, canaliculi, lacrimal sac) ▪ CDCR is not required when these structures are intact. • Dacryocystorhinostomy (DCR): Performed in cases of distal obstruction (nasolacrimal duct)
Eyelid Anatomy, Reconstruction, and Blepharoplasty
General Anatomy (see Figure 26.1)
Lacrimal/Eyelid Physiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Eyelid Anatomy, Reconstruction, and Blepharoplasty
Chapter 26