Erythema Nodosum
Michelle T. Chevalier
David C. Reid
I. BACKGROUND
Erythema nodosum (EN), the most common type of panniculitis (fat inflammation), is a reactive inflammatory condition. It occurs in association with a broad range of predisposing factors and disease processes and is most commonly attributed to an immune complex-mediated or type IV delayed hypersensitivity response to an inciting antigen. Various infections, drugs, systemic disease states, and malignancies have been associated with EN (Table 15-1). The relative frequency of etiologic agents varies by geographic location. Approximately 50% of cases are thought to be idiopathic. Pathologically, neutrophilic infiltration leads to the release of reactive oxygen species and oxidative tissue damage.
Upper respiratory tract infection secondary to β-hemolytic strep (Streptococcus pyogenes, Lancefield Group A) is the most common infectious cause of EN and the most frequent etiology in children. Other common etiologies include coccidioidomycosis and gastroenteritis secondary to Yersinia, Salmonella, or Campylobacter infections. Additional infectious causes such as tuberculosis must be considered in patients from endemic areas or with other risk factors.
Pharmaceutical agents that are commonly reported as causes of EN include estrogen-containing medications (e.g., oral contraceptives), sulfonamides, penicillin, and halogens (bromides and iodides). The incidence of oral contraceptive-associated EN has decreased with reduction in the hormone levels in these products. The high hormonal state of pregnancy can also trigger EN.
Sarcoidosis is the most common underlying inflammatory disease state associated with EN. Other less frequent etiologies include inflammatory bowel disease (Crohn disease > ulcerative colitis), Behçet’s disease, and Sweet syndrome. Various malignancies have also been associated (Table 15-1).
II. CLINICAL PRESENTATION
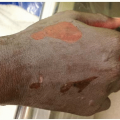
EN most commonly presents with a rapid onset of bilateral, erythematous, warm, tender nodules, and plaques on the pretibial lower legs (Fig. 15-1). Less common sites of involvement include the thighs and extensor forearms. Rarely, lesions on the head, neck, or trunk may be seen. These cutaneous findings are often preceded by a prodrome of fever, malaise, arthritis, and arthralgias (1 to 3 weeks prior to eruption). Associated cough, headache, gastrointestinal upset, ocular findings (conjunctivitis and episcleral lesions), lymphadenopathy, hepatosplenomegaly, and pleuritis have also been reported. While disease onset can occur at any age, EN most often presents between the second and fourth decades of life. There is a strong female predisposition, with a reported female to male ratio as high as 6:1 among adults.
Individual lesions of EN persist for approximately 2 weeks, followed by slow resolution without scarring. Although ulceration is extremely rare, subcutaneous hemorrhage often does occur, leading to a bruise-like appearance (erythema contusiformis) in late-stage lesions. Additional new crops of lesions may erupt for as long as 6 weeks after the initial presentation. Rare, chronic variants of EN have also been described (EN migrans and subacute nodular migratory panniculitis). Arthralgias and rheumatoid factor-negative arthritis have been reported to persist in the absence of recurrent EN lesions.
TABLE 15-1 Reported Causes of Erythema Nodosuma | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|